Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Contact dermatitis is an eczematous dermatitis caused by exposure to substances in the environment. Those substances act as irritants or allergens and may cause acute, subacute, or chronic eczematous inflammation. To diagnose contact dermatitis one must first recognize that an eruption is eczematous. Contact allergies often have characteristic distribution patterns indicating that the observed eczematous eruption is caused by external rather than internal stimuli. Elimination of the suspected offending agent and appropriate treatment for eczematous inflammation usually serve to manage patients with contact dermatitis effectively. However, in the many cases in which this direct approach fails, patch testing is useful.
It is important to differentiate contact dermatitis caused by irritation from that caused by allergy. An outline of these differences is listed in Table 4.1 .
| Irritant | Allergic | |
|---|---|---|
| People at risk | Everyone | Genetically predisposed |
| Mechanism of response | Nonimmunologic; a physical and chemical alteration of epidermis | Delayed hypersensitivity reaction |
| Number of exposures | Few to many; depends on individual's ability to maintain an effective epidermal barrier | One or several to cause sensitization |
| Nature of substance | Organic solvent, soaps | Low-molecular-weight hapten (e.g., metals, formalin, epoxy) |
| Concentration of substance required | Usually high | May be very low |
| Mode of onset | Usually gradual as epidermal barrier becomes compromised | Once sensitized, usually rapid; 12–48 h after exposure |
| Distribution | Borders usually indistinct | May correspond exactly to contactant (e.g., watchband, elastic waistband) |
| Investigative procedure | Trial of avoidance | Trial of avoidance, patch testing, or both |
| Management | Protection and reduced incidence of exposure | Complete avoidance |
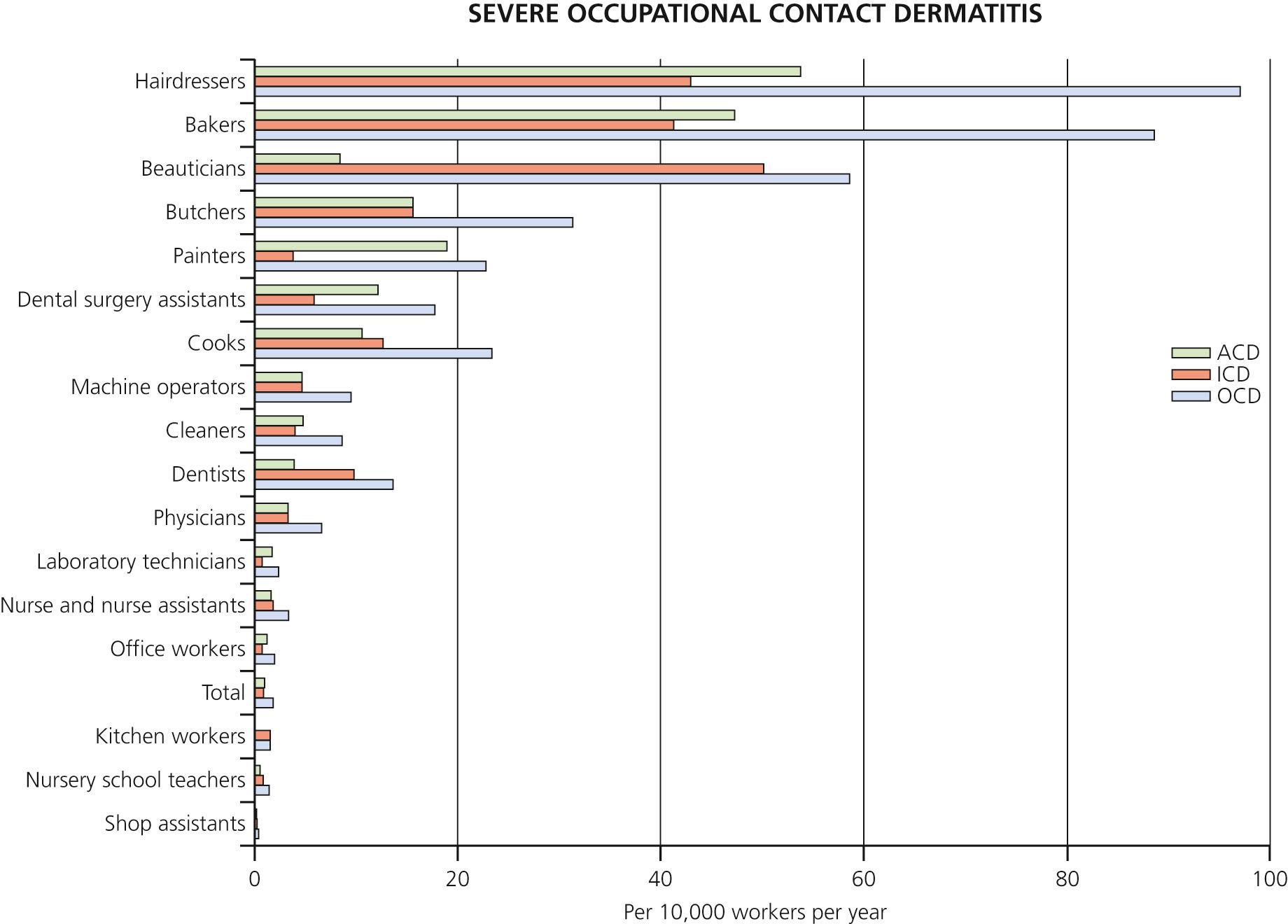
Occupational contact dermatitis occurs when a chemical contacts the skin causing a rash. Estimates indicate that the skin of 13 million workers in the United States is exposed to chemicals. Cutaneous occupational disease is the most common occupational related disease, accounting for annual costs of over 1 billion dollars annually. To study occupations at risk, investigators from Copenhagen University examined 1000 consecutive patients. Females who were cooks, butchers, beauticians, bakers, and hairdressers were at risk for occupationally induced dermatitis at rates of 23.3 to 96.8 cases per 10,000 workers per year. Men who worked as painters, cooks, mechanics, locksmiths, and bakers developed occupational dermatitis at rates of 16.5 to 32.3 cases per 10,000 workers per year ( Fig. 4.1 ).
Irritation of the skin is the most common cause of contact dermatitis and is increasing in prevalence. The epidermis is a thin cellular barrier with an outer layer composed of dead cells in a water–protein–lipid matrix. Any process that damages any component of the barrier compromises its function, and a nonimmunologic eczematous response may result. Extraction of lipids from the skin can be caused by repeated use of strong alkaline soap or industrial exposure to organic solvents. Acids may combine with water in the skin and cause dehydration. When the skin is compromised, exposure to even a weak irritant sustains the inflammation. The intensity of the inflammation is related to the concentration of the irritant and the length of exposure. Mild irritants cause dryness, fissuring, and erythema; a mild eczematous reaction may occur with continuous exposure. Continuous exposure to moisture in areas such as the hand, the diaper area, or the skin around a colostomy may eventually cause eczematous inflammation. Strong chemicals may produce an immediate reaction. Skin lesions of irritant contact dermatitis are confined to the cutaneous area of exposure, unlike allergic contact dermatitis where the rash extends beyond the area of exposure. Figs. 4.2 through 4.5 show examples of irritant dermatitis.




Patients vary in their ability to withstand exposure to irritants. Some people cannot tolerate frequent hand washing whereas others may work daily with harsh cleaning solutions without any difficulty.
Avoid exposure to irritants by using protective equipment, such as gloves.
Topical steroids are used to initially control inflammation but there is some evidence that they may compromise barrier function. Some experts recommend that the use of topical steroids should be avoided.
Moisturizers used generously and frequently increase skin hydration, and their lipid component improves the damaged skin barrier. Lipid-rich moisturizers both prevent and treat irritant contact dermatitis.
Barrier creams containing dimethicone or perfluoropolyethers, cotton liners, and softened fabrics prevent irritant contact dermatitis.
Cool compresses are used for acute inflammation. They suppress vesiculation and decrease inflammation.
Hands should be washed in cool or tepid water.
Repeated low-level ultraviolet (UV) exposures may be effective for long-term resistant cases.
Even after the skin appears normal, it takes approximately 4 months or more for barrier function to normalize.
Allergic contact dermatitis is a delayed type IV inflammatory reaction that follows absorption of antigen applied to the skin and recruitment of previously sensitized, antigen-specific T lymphocytes into the skin. The antigens are usually low-molecular-weight substances that readily penetrate the stratum corneum. Most contact allergens require repeated exposure before sensitization occurs. Strong antigens, such as poison ivy, require only two exposures for sensitization.
Interaction between antigen and T lymphocytes is mediated by antigen-presenting epidermal cells (dermal dendritic cells and Langerhans cells) and is divided into two sequential phases: an initial sensitization phase and an elicitation phase.
An antigen applied to the skin surface penetrates through the epidermal barrier (stratum corneum) and activates the innate immune system, through keratinocyte release of cytokines (interleukin [IL]-1α, IL-1β, tumor necrosis factor alpha, and others). Langerhans cells and dermal dendritic cells take up the allergen, migrate to regional lymph nodes and activate antigen-specific T cells, which in turn enter the circulation and return to the site of exposure. Dermal dendritic cells are effective in recruiting naive T cells in the lymph node, inducing antigen-specific sensitization, while Langerhans cells stimulate regulatory T cells and promote tolerance to antigens.
The elicitation phase occurs in previously sensitized patients. Upon re-exposure to the allergen, sensitized T cells activate an inflammatory cascade, producing intense itch and rash. Allergic contact dermatitis develops within 12 to 48 hours of an antigen exposure and persists for 3 or 4 weeks.
An allergen, the chemical structure of which is similar to that of the original sensitizing antigen, may cause inflammation because the immune system is unable to differentiate between the original and the chemically related antigen. For example, the skin of patients who are allergic to balsam of Peru, which is present in numerous topical preparations, may become inflamed when exposed to the chemically related benzoin in tincture of benzoin.
Systemic contact dermatitis results from the exposure to an allergen by ingestion, inhalation, injection, or percutaneous penetration in a person previously sensitized to the allergen by cutaneous contact. Patients allergic to poison ivy develop diffuse inflammation following the ingestion of raw cashew nuts ( Fig. 4.6 ). Cashew nut oil is chemically related to the oleoresin of the poison ivy plant. Persons allergic to balsam of Peru and/or fragrance mix benefit from dietary avoidance of balsams. Systemic contact dermatitis should be suspected when patients have refractory or persistent allergic contact dermatitis, despite avoiding the allergens. The most common clinical presentation is vesicular hand dermatitis due to ingestion of metals (nickel, cobalt, and chromium), balsam of Peru, garlic, and food preservatives. Pruritic papules on the extensor surface of the elbows and knees can also occur. Prior sites of contact dermatitis can re-inflame after ingestion of an allergen. Sesquiterpene lactones such as herbs, spices, and flowers such as chamomile, chicory, lettuce, and echinaceas can flare eczema. Aspartame can cause systemic contact dermatitis in formaldehyde-allergic patients because it is converted to formaldehyde in the liver. Sorbic acid found in strawberries, prunes, and cheeses can cause perioral dermatitis. Garlic can cross-react with balsam of Peru and can cause chronic and vesicular hand eczema. Propolis allergy is increasing in prevalence and can cross-react with balsam of Peru. Propylene glycol is used as a thickening agent in foods and may cause systemic contact dermatitis.

The shape and location of the rash are the most important clues to the cause of the allergen ( Table 4.2 ). The pattern of inflammation may correspond exactly to the shape of the offending substance ( Figs. 4.7 to 4.12 ). The diagnosis is obvious when inflammation is confined specifically to the area under a watchband, shoe, or elastic waistband. Plants (e.g., poison ivy) produce linear lesions.
| Location | Material |
|---|---|
| Scalp and ears | Shampoos, hair dyes, topical medicines, metal earrings, eyeglasses, rubber ear plugs |
| Face | Cosmetics (preservatives, emulsifiers, fragrances) Acne medications (e.g., benzoyl peroxide), aftershave lotions Respirators, masks, aerosolized mists (machinists), volatile organic substances (e.g., amine hardeners in the plastic industry) Chemicals (hair dyes) applied to scalp spread to face, ears, and neck – spares scalp (scalp is resistant) Airborne allergens (poison ivy from burning leaves, ragweed) Photoallergic reactions – spare upper lip and have sharp cut-off at jawline (sunscreen ingredients – oxybenzone, benzophenone no. 3) |
| Eyelids | Nail polish (transferred by rubbing), cosmetics, contact lens solution, metal eyelash curlers, make-up sponges (rubber) Lower lids (topical medications) Periocular area (goggles) |
| Upper and lower eyelids | Cause is usually not allergic (atopic dermatitis, seborrheic dermatitis, psoriasis) |
| Facial and eyelid accentuation | Airborne contact dermatitis (ragweed, volatile organic substances, fragrances, chemicals in smoke) Products applied to hands and transferred to face (nail enamels) |
| Mucosal | Most patients allergic to allergens applied intraorally have cheilitis but not stomatitis; individual who reacts to nickel, mercury, palladium, or gold in dental amalgams presents with a systemic contact dermatitis with or without a localized stomatitis |
| Neck | Necklaces (metals, exotic woods), airborne allergens (ragweed), perfumes, aftershave lotion; cosmetic allergens; textile dermatitis (dyes, formaldehyde resins in clothing) |
| Trunk | Textile (sparing of axillary and undergarment areas) Azoaniline dyes (color clothing) Urea formaldehyde resins (wrinkle-resistant clothing) N ote : p -Phenylenediamine (PPD) and formaldehyde are not adequate screens for patch testing for allergy to textile dyes and resins Rubber allergens: Elasticized waist bands, spandex bras N ote : Standard rubber patch test allergens may be negative; patch test with a portion of elastic band from a garment that has been bleached Generalized reactions Fragrances, preservatives in moisturizing lotions, topical medication, sunscreens; poison ivy; plants (phototoxic reactions); metal belt buckles Laundry detergents rarely cause allergic contact dermatitis |
| Scattered, generalized dermatitis | “Systemic contact dermatitis” – an individual who has been sensitized topically to an allergen and is subsequently re-exposed systemically (drug/chemical introduced intramuscularly, intravenously, orally, rectally, or vaginally), foods, medical or dental devices that contact mucosal surfaces or that have been implanted surgically into body Cinnamic aldehyde and balsam (cosmetics, topical medications, suppositories, dental liquids, and flavorings) or parabens (food preservatives) Contaminants in foodstuffs, such as nickel |
| Arms | Same as hands; watch and watchband Photosensitive process (rash ends at mid-upper arm) Soap, moisturizing creams |
| Fingertips | Hairdressers – glyceryl monothioglycolate in permanent solutions or p -phenylenediamine in hair dyes Nurses – glutaraldehyde in disinfectants Dental and orthopedic personnel – glue (methylmethacrylate) Many chemicals penetrate standard gloves |
| Axillae | Deodorant (axillary vault), clothing (axillary folds) |
| Hands | Soaps and detergents, foods, spices, poison ivy, industrial solvents and oils, cement, metal (pots, rings), topical medications, rubber gloves in surgeons |
| Genitals | Poison ivy (transferred by hand), rubber condoms, diaphragms, pessaries |
| Anal region | Hemorrhoid preparations (benzocaine, Nupercaine) |
| Lower legs, popliteal fossa, and inner thigh | Topical medication (benzocaine, lanolin, neomycin, parabens) Fragrances, preservatives, and vehicles in moisturizers and cosmetics Dyes in pantyhose (especially blue disperse dyes in darker-colored hose and disperse yellow no. 3 in skin-colored hose) Textiles |
| Feet | Shoes – p-tert -butylphenol formaldehyde resin (a component of shoe glues), rubber components, and chromate (used to tan leather) Cement spilling into boots |





Unfortunately most allergic reactions do not conform precisely to the areas contacting the allergen. A woman allergic to an ingredient in her facial cosmetic typically presents with a patchy facial eczema, rather than with a diffuse dermatitis involving all areas of the face to which the cosmetic was applied. An allergen may be spread to other sites by inadvertent contact. The scalp, palms, and soles are resistant to allergic contact dermatitis and may show only minimal inflammation despite contact with an allergen that produces dermatitis in adjacent areas.
Aeroallergens inflame the exposed skin and spare clothed areas. Clothing allergens cause dermatitis of clothed areas. Table 4.2 lists substances that are common causes of inflammation in specific body regions. Table 4.3 lists substances commonly encountered in specific professions.
| Occupation | Irritants | Allergens |
|---|---|---|
| Beauticians | Wet work (shampoos) | Hair tints, permanent solution, shampoos (formaldehyde) |
| Construction workers | Fuels, lubricants, cement | Cement (chromium, cobalt), epoxy, glues, paints, solvents, rubber, chrome-tanned leather gloves |
| Chefs, bartenders, bakers | Moist foods, juices, corn, pineapple juice | Orange and lemon peel (oil of limonene), mango, carrot, parsnips, parsley, celery; spices (e.g., capsicum, cinnamon, cloves, nutmeg, vanilla) |
| Farmers | Milker's eczema (detergents), tractor lubricants and fuels | Malathion, pyrethrum insecticides, fungicides, rubber, ragweed, marsh elder |
| Forest products industry | Wet work (wood processing) | Poison ivy and oak, plants growing on bark (e.g., lichens, liverworts) |
| Medical and surgical personnel | Surgical scrubbing | Rubber gloves, glutaraldehyde (germicides), acrylic monomer in cement (orthopedic surgeons), penicillin, chlorpromazine, benzalkonium chloride, neomycin |
| Printing industry | Alcohols, alkalis, grease | Polyfunctional acrylic monomers, epoxy acrylate oligomers, isocyanate compounds (all used in a new ink-drying method) |
The failure of an eczematous dermatitis to respond to standard treatments and worsening of a previously stable dermatitis also suggest that the dermatitis is allergic and not irritant.
The intensity of inflammation depends on the degree of sensitivity and the concentration of the antigen. Strong sensitizers such as the oleoresin of poison ivy may produce intense inflammation in low concentrations, whereas weak sensitizers may cause only erythema. The appearance also depends on location and duration. Acute inflammation appears as macular erythema, edema, vesicles, or bullae. Chronic inflammation is characterized by lichenification, scaling, or fissures. Contact allergies may have noneczematous patterns that include the cellulitis-like appearance of dermal contact hypersensitivity, lichenoid variants, contact leukoderma, contact purpura, and erythema multiforme.
Acute and chronic dermatitis results from allergens and irritants suspended in the air. The face, neck, V region of the chest, forearms, and hands, including the palms are commonly affected areas. Allergens fall on surfaces and clothing and when patients touch the surfaces, the palms become involved. Allergens can also collect on the upper eyelids, posterior ears and submandibular regions. These locations assist in differentiating an airborne contact dermatitis from a photodermatitis, since these areas are not photodistributed.
Sprays, perfumes, chemical dusts, and plant pollen (e.g., sesquiterpene lactones found in ragweed, goldenrod, sunflowers, and chrysanthemums) are possible sources. Almost all published causes are occupationally related ( Table 4.4 ). The sources are drugs (e.g., by crushing drugs for the elderly), plants (e.g., urushiol found in poison ivy, poison oak and poison sumac), natural resins and woods, plastic, metals (nickel, silver, mercury, gold, arsenic salts), rubber and glue components, cement (potassium dichromate) and preservatives (methylisothiazolinone and methylchloroisothiazolinone).
| Agent | Products | Occupations/Industries |
|---|---|---|
| Ammonia | Disinfectants, fertilizers, bleaching agents, baking flour | Farming, homemaking, cleaning services |
| Chrome | Cement, concrete mix, cosmetics, paint, alloy metals | Construction, building, stonemasonry, metal working, paper industry |
| Epoxy resin | Glues, adhesives, paint, polyvinyl chloride products, electric insulators, plastics | Painting, paint manufacture, construction, building, carpentry |
| Fiberglass | Boats, cars, aircraft, building insulation, clothing, helmets | Automotive and aviation industries, insulation manufacturing, building, construction |
| Formaldehyde | Fabric finishes, cosmetics, toiletries, embalming, disinfectants, paper products | Textile industry, sanitary paper production, builders, construction |
| Gold | Jewelry, plating, cell phones, electronics, dental and orthodontic appliances | Jewelry, plating, photography, electronics manufacture, dentistry and dental hygiene |
| Isothiazolinones | Preservatives in cleaning products, cosmetics, paint | Homemaking, cleaning services, health care, painting |
| Natural rubber latex | Tires, gloves, adhesive tape, balloons, condoms, paint | Latex product manufacture, health care, hairdressing |
| Nickel | Plating, alloy metals including stainless steel, coins | Refining, electronics manufacture, hairdressing, cashier work, metal work |
| Medications | Azathioprine, budesonide, famotidine, lansoprazole, methotrexate | Pharmacy, pharmaceutical manufacture, health care |
| Wood dust | Tropical and domestic wood | Carpentry, building, construction, furniture manufacture, sawmills |
Inflammation from airborne sensitizers tends to be more diffuse. Volatile substances can collect in clothing, producing a rash. Phosphates, metal dusts, carbon fiber and fiberglass, epoxy resin, ammonia, cleaning products, anhydrous calcium sulfate, and formaldehyde may cause irritant contact dermatitis.
Allergic contact dermatitis may account for as many as 20% of all cases of dermatitis in children. Poison ivy, nickel (jewelry), rubber (shoe dermatitis), balsam of Peru (hand and face dermatitis), formaldehyde (cosmetics and shampoos), and neomycin (topical antibiotic ointments) are the common allergens.
Minimize products for topical use.
Use ointments instead of creams (creams contain preservatives and are complex mixtures of chemicals).
Botanical extracts may be used in “fragrance-free” products.
When patch testing, also test the patient's consumer products.
Read product labels carefully. Many “dermatologist recommended” products contain sensitizers (e.g., lanolin, fragrance, quaternium-15, parabens, methylchloroisothiazolinone/methylisothiazolinone).
In the United States poison ivy, poison oak, and poison sumac produce more cases of allergic contact dermatitis than all other contactants combined. The allergens responsible for poison ivy and poison oak allergic contact dermatitis are contained within the resinous sap material termed urushiol. Urushiol is composed of a mixture of catechols. All parts of the plant contain the sap. These plants belong to the Anacardiaceae family and the genus Rhus . Other plants in that family, such as cashew trees, mango trees, Japanese lacquer trees, and ginkgo, contain allergens identical to or related to those in poison ivy. Thousands of workers on cashew nut farms in India develop hand dermatitis from direct contact with the irritating resinous oil from cashew nut shells. Poison ivy and poison oak are neither ivy nor oak species.
Rhus dermatitis occurs from contact with the leaf or internal parts of the stem or root and can be acquired from roots or stems in the fall and winter. The clinical presentation varies with the quantity of oleoresin that contacts the skin, the pattern in which contact was made, the susceptibility of individuals, and regional variations in cutaneous reactivity. Small quantities of oleoresin produce only erythema whereas large quantities cause intense vesiculation ( Figs. 4.13 to 4.17 ).





The highly characteristic linear lesions are created when part of the plant is drawn across the skin or from streaking the oleoresin while scratching. Diffuse or unusual patterns of inflammation occur when the oleoresin is acquired from contaminated animal hair or clothing or from smoke while burning the plant. The eruption may appear as quickly as 8 hours after contact or may be delayed for 1 week or more. The appearance of new lesions 1 week after contact may be confusing to the patient, who may attribute new lesions to the spread of the disease by touching active lesions or to contamination with blister fluid. Blister fluid does not contain the oleoresin and, contrary to popular belief, cannot spread the inflammation.
Washing the skin with any type of soap inactivates and removes all surface oleoresin, thereby preventing further contamination. Washing must be performed immediately after exposure. After 10 minutes, only 50% of urushiol can be removed; after 30 minutes, only 10% can be removed; and after 60 minutes, none can be removed.
The organoclay compound 5% quaternium-18 bentonite lotion (IvyBlock) prevents dermatitis in more than 50% of sensitized and exposed patients.
Blisters and intense erythema are treated with cold, wet compresses, and they are highly effective during the acute blistering stage. Cold compresses should be used for 15 to 30 minutes several times a day for 1 to 3 days until blistering and severe itching are controlled. Topical steroids do not penetrate through blisters. Short, cool tub baths with or without colloidal oatmeal (Aveeno) are very soothing and help to control widespread acute inflammation. Calamine lotion controls itching but prolonged use causes excessive drying. Hydroxyzine and diphenhydramine control itching and encourage sleep.
Mild to moderate erythema may respond to topical steroids. Group I to V creams or gels applied two to four times a day rapidly suppress erythema and itching.
Severe poison ivy is treated with prednisone. A single-dose treatment schedule is shown in Table 4.5 . Prednisone, administered in a dosage of 20 mg twice each day for at least 7 days, is an alternative schedule for severe, widespread inflammation. Tapering the dosage after this short course is usually not necessary. Patients who may have trouble adhering to a medication schedule may be treated with triamcinolone acetonide (40 mg) given intramuscularly. Commercially available steroid dose packs (e.g., Medrol Dosepak) should be avoided because they provide an inadequate amount of medicine and may cause recurrence of rash and pruritus after initial partial amelioration of symptoms during the first days of treatment (rebound dermatitis). Patients who do not initially seem to require medication may become much worse 1 or 2 days after an office visit; they should be advised that prednisone is available if their conditions worsen.
| Day | Dosage (mg/day) 10-mg Tablets, Taken as a Single Dose Each Morning |
|---|---|
| 1–4 | 60 |
| 5–6 | 50 |
| 7–8 | 40 |
| 9–10 | 30 |
| 11–12 | 20 |
| 13–14 | 10 |
* NOTE: It is common practice to prescribe prednisone as a single morning dose to avoid adrenal suppression. Dosing prednisone twice a day provides a more effective antiinflammatory effect. Prednisone, administered in a dosage of 20 mg twice each day for at least 7 days, is an alternative schedule for severe, widespread inflammation. Tapering the dosage after this short course is usually not necessary.
The diagnosis is usually obvious. The intense, often linear, vesicular eruption is highly characteristic. Patch testing is not done because there is a high risk of inducing allergic reactions in individuals who have not yet been sensitized.
Allergy to natural rubber latex (NRL) is a national health problem. Groups at highest risk include health care workers, rubber industry workers, and persons who have undergone multiple surgical procedures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here