Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Intraoperative and frozen section analyses are relatively uncommon for genitourologic surgery with about 5.4% of all urologist-generated specimens at our institution being submitted for intraoperative consultation (IOC). General indications include: 1) evaluation of resection margins, 2) diagnosis or classification of lesions, and 3) ruling out metastasis in a lymph node or tumor. Diagnostic issues related to the first two topics are specific for each genitourinary (GU) organ and addressed under their respective headings. Evaluation for metastatic disease is relatively similar across each organ system and will be addressed under its own heading at the end of the chapter.
Intraoperative analysis is requested on 15% of nephrectomy specimens at our institution. In the setting of a renal mass, consultation might include: 1) evaluation of resection margins on a partial nephrectomy, 2) identification and classification of a mass, 3) determination of urothelial versus renal cancer primary, and 4) evaluation of lymph node or extrarenal mass for metastatic tumor.
The number of partial nephrectomies has increased as radiographic imaging has increased the number of small, incidentally detected renal tumors. Perhaps one of the most common indications in genitourinary pathology is evaluation of resection margins from a partial nephrectomy (Berdjis et al, 2006). Intraoperative positive margin usually necessitates additional tissue resection (Kubinski et al, 2004).
Tissue from the resection margins may be sent either as a separate specimen or requested on the nephrectomy itself. Tissue designated as margin may be sent without specific orientation and therefore totally embedded; the presence of tumor within the section is determined to be positive. When handling a partial nephrectomy specimen, inking the resection surface and 5-mm (or smaller) serial sections perpendicular to the margin ( Figure 16-1 ) is recommended to find the closest approach to the margin (Hagemann et al, 2009). The blade is rinsed or wiped clean as sections are made to prevent accidental carryover of tumor. Preference of gross evaluation only or examination with frozen section can vary with urologists and specifics of the case. During surgery the urologist is usually able to recognize gross violation of the tumor and modify the resection plane. In the setting of a small tumor with clinically wide margins, the urologist might consider gross examination sufficient, with a measurement of the distance to the margin, i.e., Tumor grossly approaches inked resection margin by 3 mm . The added utility of frozen section examination in this setting is arguably limited, with the disadvantage of longer turnaround time. Although the false positive rate should be minimal with gross evaluation, a urologist might prefer microscopic confirmation by frozen section. In this situation, the tumor must be in contact with the inked or cauterized surface to be considered a true positive margin. If tumor cells are very close to the margin, it may be useful to report the distance to the margin (i.e., tumor cells present 0.5 mm from margin of resection) because additional marginal tissue might be obtained for greater clearance.
Generally, sophisticated imaging and/or biopsy techniques characterize most renal lesions sufficiently for purposes of surgery, and intraoperative management is not altered by frozen section. Occasionally, an IOC may be requested simply to confirm the presence of a mass (usually with a small lesion), in which case a gross consultation may suffice. Occasionally, a request for specific histologic diagnosis is made. In either situation, careful gross examination is critical, and the prosector must properly orient the specimen and margins and apply ink to critical margins as appropriate. Once the specimen is cut, the size and location of the mass, its relationship to the cortex and pelvis, exophytic versus infiltrative growth pattern, color, consistency, encapsulation, and circumscription should be recorded. Often the pathologist is asked to differentiate between a benign and malignant lesion. The surgeon may have encountered a critical structure, such as the renal pelvis or main renal vessel, and continued resection to achieve a negative margin would require a total nephrectomy. If organ preservation with a partial nephrectomy is critical, IOC can dictate the surgical outcome. Clinical history, knowledge of imaging studies, and good communication with the surgeon is imperative for the pathologist to fully understand the subtleties of each case and his or her role in diagnosis and guiding intraoperative management. Gross photography and retrieval of fresh tissue for biobanking for future studies should also be considered prior to specimen fixation.
The differential diagnosis of renal masses is broad and requires correlation of gross and clinical findings. Considerations typically include renal cortical neoplasms (renal cell carcinoma, adenoma), angiomyolipoma (AML), urothelial carcinoma, extrarenal metastasis, and nonneoplastic lesions such as cyst, abscess, scars, granuloma, xanthogranulomatous pyelonephritis, or malakoplakia.
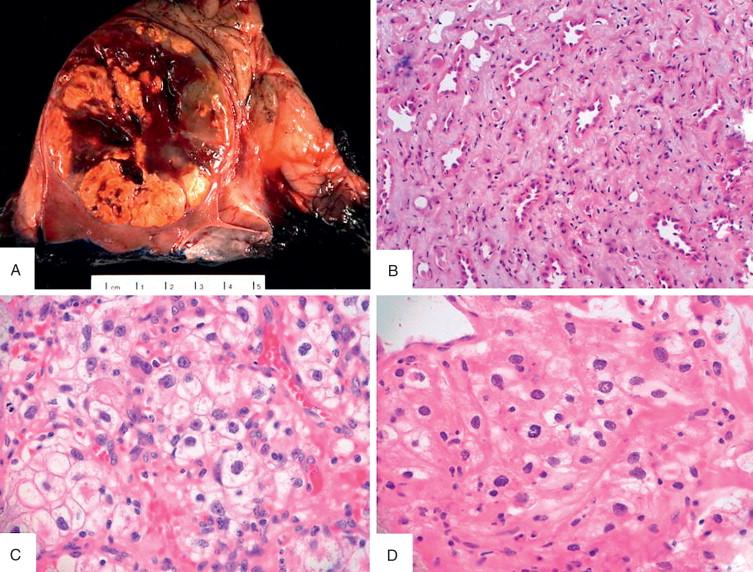
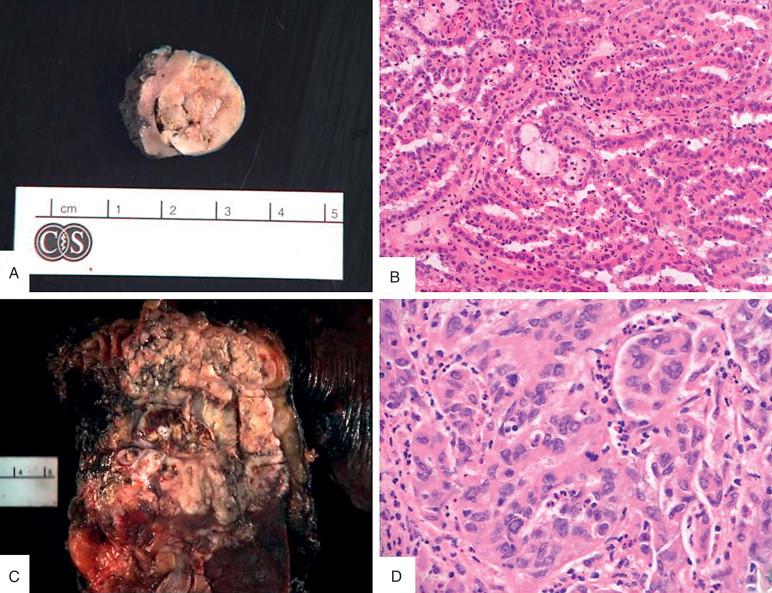
Renal cell carcinoma (RCC) is the most common cortical mass removed at our institution, followed by cysts and angiomyolipomas. RCC subtypes include clear cell, papillary, chromophobe and sarcomatoid, although sub-classification is usually not necessary as it does not typically impact intraoperative management. Therefore, in most cases, the diagnosis of renal cell carcinoma is sufficient. Nonetheless, the common subtypes of renal cell neoplasms have characteristic gross and microscopic findings that can be useful intraoperatively. One important challenging differential both on gross and histologic examination is chromophobe renal cell carcinoma versus oncocytoma, and caution should be exercised when confronting this scenario, with significant clinical impact. Features of renal cell neoplasms are highlighted in Table 16-1 and Figures 16-1, 16-2 , and 16-3 .
| Gross | Microscopic | |
|---|---|---|
| Clear Cell RCC | Golden-yellow, commonly with necrosis, hemorrhage, cystic change | Nested clear cells with prominent sinusoidal vasculature; vacuolated or clear cytoplasm; higher grade tumors may appear more eosinophilic |
| Papillary RCC | Fibrous pseudocapsule, cut surface is variegated. Prominent necrosis hemorrhage, cystic change | Well-defined capsule, papillary or tubular architecture, occasionally solid. Vascular cores with foamy macrophages, psammoma bodies, hemosiderin deposition, variable cytoplasm |
| Chromophobe RCC | Well circumscribed, nonencapsulated, homogenous brown-tan, occasional central scar, can have hemorrhage and necrosis | Classically with "plant-cell" like appearance, pale flocculent cytoplasm, "raisinoid" nuclei, binucleation, perinuclear halos |
| Oncocytoma | Well circumscribed, mahogany brown to tan with central scar | Nests of eosinophilic cells with densely granular cytoplasm, regular round nuclei with central nucleoli |
Occasionally, questions regarding tumor stage arise, which can usually be addressed by close gross examination. Rarely is there a clinical need for histologic confirmation of this aspect. Similarly, there is little clinical utility for other histopathologic assessment of prognostic parameters such as tumor grading or sarcomatoid change.
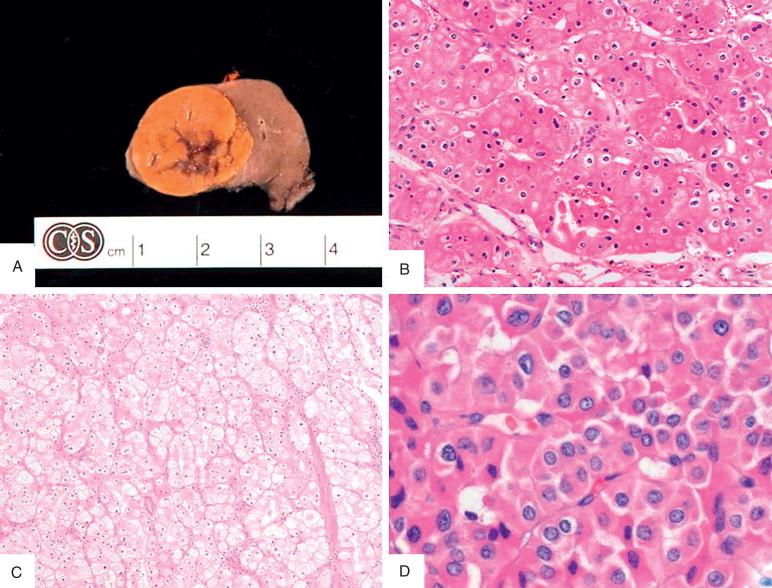
Angiomyolipomas (AML) of the kidney are common incidental findings, and the presence of multiple lesions is highly associated with tuberous sclerosis. CT imaging is often diagnostic given the presence of fat within the lesion. However, the variability of AML histology, with leiomyomatous or fat-poor subtypes, can yield equivocal findings on imaging. Lesions are usually well circumscribed and unencapsulated ( Figure 16-5A ). Diagnosis of AML requires the classic triphasic histology of adipose tissue, thick-walled hyalinized vessels, and smooth muscle fibers ( Figure 16-5B ). Generally, AML connotes a benign diagnosis, although the presence of epithelioid components (a very rare scenario) is associated with malignant potential.
Evaluation of spindled cell lesions can be particularly challenging on frozen section. The differential includes sarcomatoid change in RCC, urothelial carcinoma, mucinous and tubular spindle cell carcinoma, cystic nephroma, or mesenchymal tumors, including AML. The degrees of nuclear atypia, presence of mitosis, and necrosis are all important factors in discriminating between benign and malignant lesions. The diagnosis of spindled cell lesion may be all that is possible on frozen section, and diagnosis would need to be deferred to further studies. In the setting of marked nuclear anaplasia, frequent mitoses, and necrosis, a sarcoma or sarcomatoid dedifferentiation of a carcinoma should be suggested, but definitive characterization is best deferred to permanent sections and potential special studies.
Nonrenal neoplasms must also be considered, particularly in cases with unusual features. Superior pole lesions may be adrenocortical adenoma or carcinoma encroaching into the kidney. Retroperitoneal tumors can displace and invade renal parenchyma. Metastasis to the kidney should be considered in any renal tumor that lacks the typical histology of renal cell carcinoma, particularly those with infiltrative growth, high-grade features, or glandular or neuroendocrine differentiation. With consideration of metastatic tumor, the differential would include high-grade renal cancers such as unclassified renal cell carcinoma, medullary, collecting duct carcinoma, and urothelial carcinoma. The frozen section interpretation should clearly state the findings descriptively and suggest a broad differential (e.g., Infiltrative carcinoma with glandular morphology, favor renal primary but cannot rule out metastasis ). Again, in this setting, clinical knowledge of any prior or concurrent malignancy is helpful. Lymphoma should always be considered in the setting of a mass with atypical lymphocytes percolating around existing renal tubules. Suspicion of lymphoma typically warrants triaging fresh tissue for ancillary studies. Again, with any particularly challenging or diagnostically uncertain case, one should consider procuring fresh tissue at the time of the frozen section for potential future molecular/cytogenetic studies.
It is critical for both the urologist and the pathologist to understand the importance of tissue sampling, high-quality histologic preparations, and the limitations imposed at the time of IOC. In particular, oncocytic and cystic renal lesions require extensive tissue sampling with high-quality histologic preparations for definitive classification, beyond what can be achieved by intraoperative evaluation. The differential diagnosis of an oncocytic renal tumor includes oncocytoma, eosinophilic variants of chromophobe and clear cell renal cell carcinoma, and epithelioid AML. AML is suggested if all three elements of fat, aberrant vasculature, and smooth muscle are present. Clear cell RCC will have a more solid appearance, higher grade nuclei, and increased vascularity. The distinction between oncocytoma and chromophobe is more challenging due to considerable overlap of gross and histologic features ( Table 16-2 and Figures 16-3 and 16-4 ).
| Oncocytoma | Chromophobe | |
|---|---|---|
| Gross | Well circumscribed, brown, often with central scar | Brown, occasional central scar |
| Architecture | Round regular nests and/or tubules, myxoid background | Complex nests, diffuse solid areas |
| Nuclei | Round regular, one nucleoli often present, atypia is rare | Binucleation common, irregular "raisinoid" nuclear atypia |
| Cytoplasm | Densely eosinophilic | Flocculent eosinophilic with perinuclear cytoplasmic clearing, distinct cell borders |
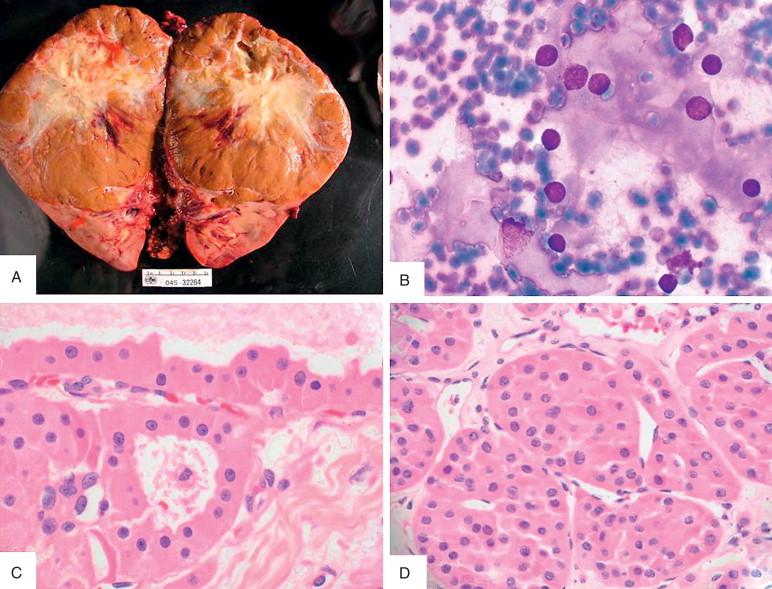
Since extensive sampling, good histology, and immunohistochemical studies may be necessary for definitive classification of oncocytic tumors, it is recommended to generally classify the lesion and defer the intraoperative classification, i.e., Oncocytic renal tumor, differential includes…defer to permanent sections and potential future studies.
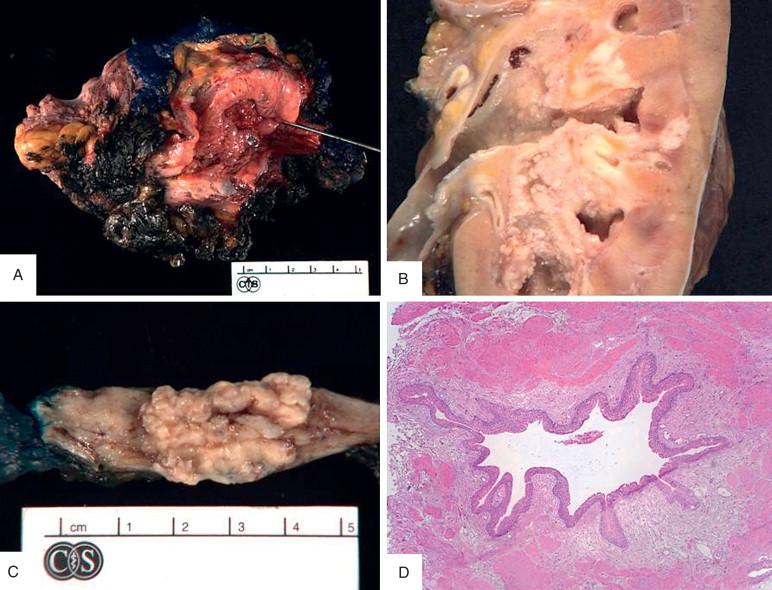
Cystic lesions are also potentially problematic because it is usually necessary to submit multiple tissue sections for proper classification. Fortunately, intraoperative requests for diagnosis are rare because little is to be gained at the time of surgery. Lesions can be sent either whole and intact or as an “unroofing” or enucleation. If received intact, inking of the outer surface allows easier orientation. The emphasis in gross examination is on multiloculated versus uniloculated; thick septations or mural nodules; fluid characteristics; and smooth-walled versus papillary excrescences. The complexity of the lesion directly correlates with its likelihood of being malignant. Differential diagnosis includes renal cell carcinoma with cystic change, multiloculated cystic renal cell carcinoma, cystic nephroma, and benign cysts (possibly with clear cell lining or papillary hyperplasia). Sampling should be targeted to any solid nodules or thick septations if present. Any large expansile nodules favor a carcinoma. If carcinoma is not evident, definitive diagnosis may necessitate multiple sections ( Figure 16-5C, D ). The time and resources to submit all such sections for frozen section rather than routine submission should be considered because it may not be practical for larger more complex lesions. Frozen section diagnosis may be stated as multilocular cystic clear cell lesion, no expansile nodules present in sampled tissue, defer to additional sections.
Nonneoplastic lesions may include areas of infarction, inflammation, abscess, and scar/fibrosis. In this setting, a quality hematoxylin-and-eosin (H&E) frozen section should point to the correct diagnosis.
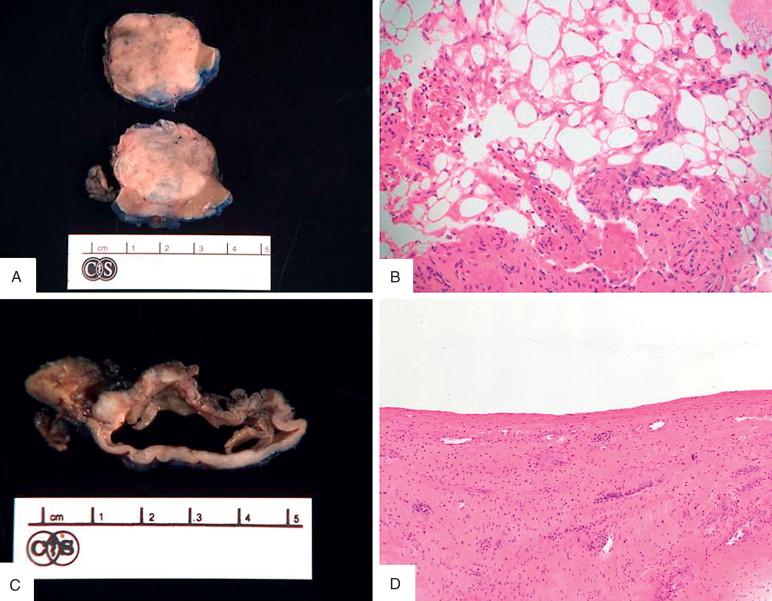
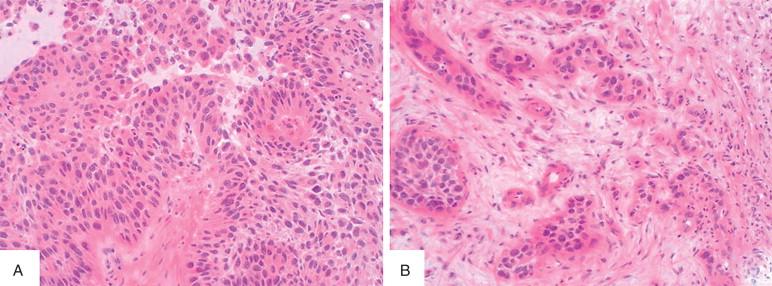
In some settings, the preoperative clinical features of a primary renal tumor may not be clear (renal cell versus urothelial cancer), and the urologist may request IOC for confirmation. The distinction between malignancy of the urothelium and renal parenchyma is critical; for renal cell carcinoma, a radical nephrectomy is performed; however, for urothelial carcinoma, the kidney, the entire ureter, and even a cuff of bladder surrounding the ureteral orifice are removed. Gross findings can be helpful. As such, the nephrectomy resection margins should be identified and inked prior to bivalving. Tumor location in the parenchyma versus pelvic mucosa usually can be determined ( Figure 16-6B ). The section for frozen evaluation ideally should include the base of the mass in the renal pelvis with renal parenchyma and any papillary or exophytic mucosal component. If an infiltrating component is present, the gross distinction can be challenging. Evidence of a papillary tumor ( Figure 16-8A ) or carcinoma in situ (may be represented as an erythematous mucosal irregularity) supports the conclusion that an invasive component is also urothelial in origin. Distinguishing features are given in Table 16-3 .
| Renal Cell Carcinoma | High Grade Urothelial Carcinoma | |
|---|---|---|
| Gross | Centered in kidney parenchyma | Papillary mass based in pelvic mucosa |
| Architecture | Varies by type but often solid, papillary, complex nested; may be infiltrating as in CDC or RMC | Irregular infiltrating nests, possible glandular or squamous differentiation |
| Nuclei | High nuclear grade with large prominent nucleoli | Pleomorphic, elongated to rounded, grooves, irregular nuclear outlines, irregular chromatin distribution, one to multiple nucleoli |
| Miscellaneous | Highly variable; may be sarcomatoid | Multiple variants: Can be rhabdoid, plasmacytoid, giant cell, sarcomatoid |
In some situations, the histology may not be definitive and immunohistochemistry can be helpful. A sample frozen section diagnosis for an equivocal case: Invasive carcinoma involving renal pelvis, no conventional urothelial carcinoma in sampled tissue, defer to permanent evaluation for classification.
Refer to section on lymph nodes.
Ureter resection for a tumor accounts for less than 1% of urologic surgical specimens at our institution and includes segmental ureterectomy and radical nephroureterectomy with and without bladder neck, almost always for urothelial carcinoma. Intraoperative consultation is requested on most resection specimens, primarily to assess margins for involvement but occasionally to identify and evaluate for the primary lesion. Many diagnostic and management issues of frozen section analysis in upper tract urothelial carcinomas are similar to pelvicalyceal tumors as discussed above in the renal section.
Margins are sent either as separate specimens or as requested on an intact, oriented ureterectomy or nephroureterectomy specimen (Gephardt and Zarbo, 1996). Unlike margins in nephrectomy specimens for renal cell carcinomas, microscopic evaluation is recommended given the multifocal “field effect” of urothelial carcinoma. Intact specimens require inking of the margin and outer surface around any palpable mass ( Figure 16-6 ). As tumors can be quite friable, displacement of a tumor during frozen section can complicate evaluation, and thus care must be used. A thin 1- to 2-mm en face section of the proximal or distal ureteral margin taken before opening the lumen minimizes this risk, and frozen section proceeds as if the margin was sent as a separate specimen. However if the tumor very closely approaches the margin, this method may result in “overcall” in some cases. Opening the ureter first to evaluate the lesion and its relationship to the inked margin and taking a perpendicular section at the area of closest approach arguably allows more accurate assessment ( Figure 16-6C ). If evaluation of a deep margin is requested, this approach is best. Diagnosis of a positive margin requires tumor at the ink; otherwise margin is reported negative ± measurement to margin. This method is more susceptible to sampling error. The preferred method is best determined on a per-case basis based on the pathologist's judgment call. If a bladder cuff is present in a nephroureterectomy and margin status is requested intraoperatively, an en face shave section will suffice.
Microscopic evaluation for carcinoma (papillary, invasive, carcinoma in situ, pagetoid spread) is similar to margins of cystectomies for bladder lesions. Refer to the bladder section for specific details.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here