Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Evaluation of the placenta, umbilical cord, and cervix is an important component of the second and third trimester obstetrical ultrasound examination. Ultrasound facilitates assessment of placental location and appearance, relationship of the placenta to the cervix, umbilical cord insertion, umbilical cord coiling and vessel number, and cervical length.
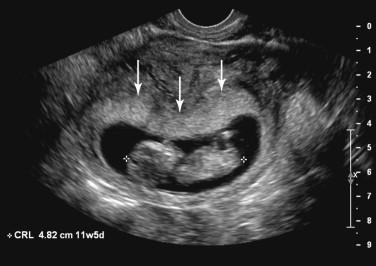
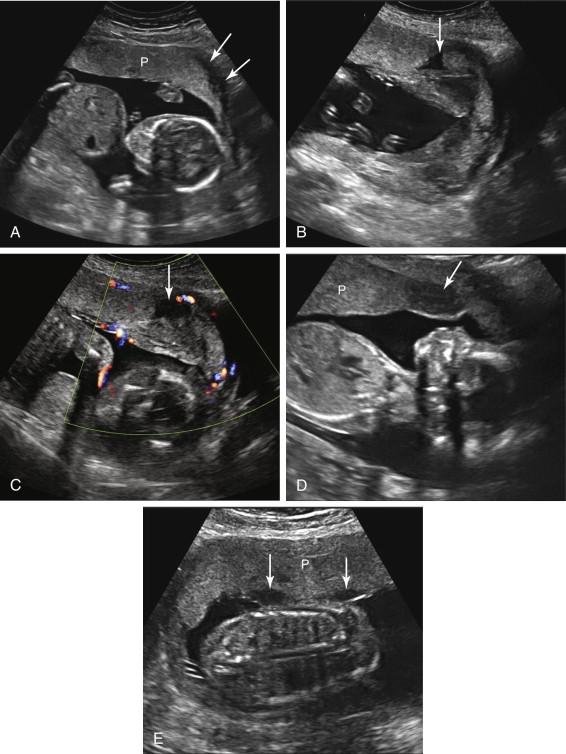
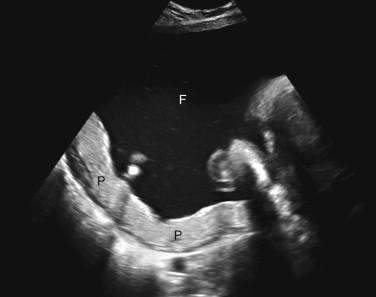
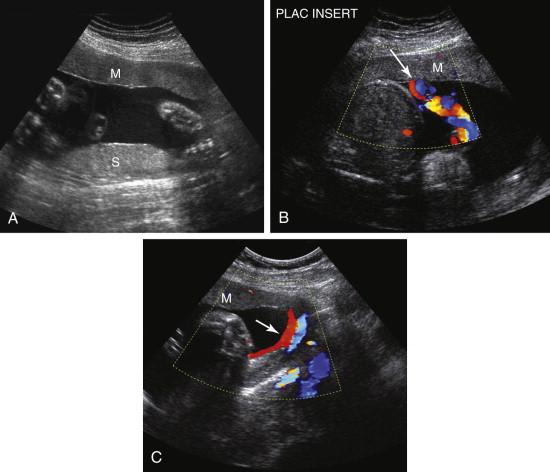
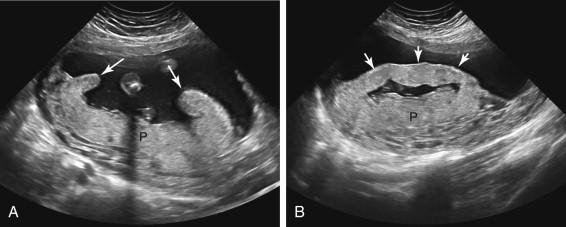
The placenta is visualized by the end of the first trimester, when it is depicted as a layer of echogenic tissue abutting the gestational sac ( Fig. 20-1 ). By the mid second trimester a well-defined, hypoechoic retroplacental layer composed of myometrium and uterine blood vessels can be visualized when imaging parameters are optimized to depict it ( Fig. 20-2A ). Additional hypoechoic areas are frequently seen in and around the normal placenta. Scattered hypoechoic regions corresponding to normal intervillous spaces (also termed placental lakes or venous lakes ) are commonly identified, and typically are small and few in number (see Fig. 20-2B ). Swirling echoes are frequently seen in these intervillous spaces at real-time evaluation, although blood flow is often too slow to be depicted at color Doppler (see Fig. 20-2C ) ( ![]() ). A hypoechoic area termed the marginal sinus is sometimes visualized at the edge of the placenta and also may have swirling echoes or flow at color Doppler evaluation (see Fig. 20-2D ). Fibrin deposition beneath the chorionic membrane on the fetal surface of the placenta causes hypoechoic areas along the fetal surface of the placenta (see Fig. 20-2E ). Cystic structures termed decidual cysts are also occasionally seen in the substance of the placenta.
). A hypoechoic area termed the marginal sinus is sometimes visualized at the edge of the placenta and also may have swirling echoes or flow at color Doppler evaluation (see Fig. 20-2D ). Fibrin deposition beneath the chorionic membrane on the fetal surface of the placenta causes hypoechoic areas along the fetal surface of the placenta (see Fig. 20-2E ). Cystic structures termed decidual cysts are also occasionally seen in the substance of the placenta.
The appearance of the placenta evolves as it matures with advancing gestation, becoming heterogeneous in echotexture. This maturation process results in development of sonographically visible calcifications in some placentas during the third trimester ( Fig. 20-3 ). Early or accelerated placental calcification has been associated with fetal growth restriction, preeclampsia, chronic hypertension, and smoking. A placental grading system was previously used to classify the stage of placental maturation based on ultrasound features; however, this system is no longer widely used.

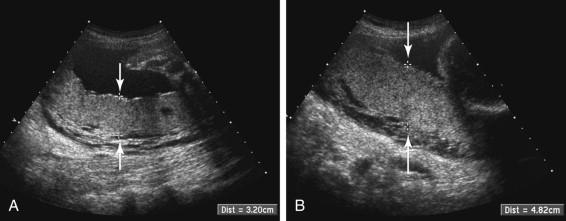
Placental thickness is assessed subjectively. Thickness is not routinely measured if the placenta subjectively appears normal. Measurements of placental thickness are performed in the midportion of the placenta, perpendicular to its long axis ( Fig. 20-4A ). An oblique measurement or a measurement near a uterine contraction or fibroid may result in a spuriously elevated value (see Fig. 20-4B ). Placental thickness between 2 and 4 cm is considered normal during the second and third trimesters of pregnancy.
The differential diagnosis for a thick placenta includes gestational diabetes, hydrops, infection, maternal anemia, intraplacental hemorrhage, placental mass, and placenta accreta ( Fig. 20-5A and B ; ![]() ) ( Box 20-1 ). In addition, gestational trophoblastic disease, triploidy, and Beckwith-Wiedemann syndrome should be considered in the setting of a thick placenta with multiple cysts.
) ( Box 20-1 ). In addition, gestational trophoblastic disease, triploidy, and Beckwith-Wiedemann syndrome should be considered in the setting of a thick placenta with multiple cysts.
Gestational diabetes
Hydrops
Infection
Maternal anemia
Intraplacental hemorrhage
Placental mass
Placenta accreta
Gestational trophoblastic disease
Triploidy
Beckwith-Wiedemann syndrome
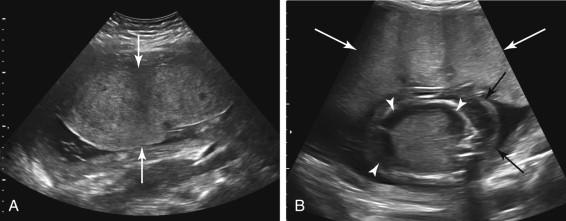
Placental thinning occurs due to maternal vascular disorders such as insulin-dependent diabetes and chronic hypertension and is associated with an increased risk for fetal growth restriction ( Box 20-2 ). Placental thinning also is seen in the setting of marked polyhydramnios, due to stretching and compression of the placenta along the inner surface of the enlarged uterus ( Fig. 20-6 ).
Insulin-dependent diabetes
Chronic hypertension
Marked polyhydramnios causing stretching and compression of the placenta
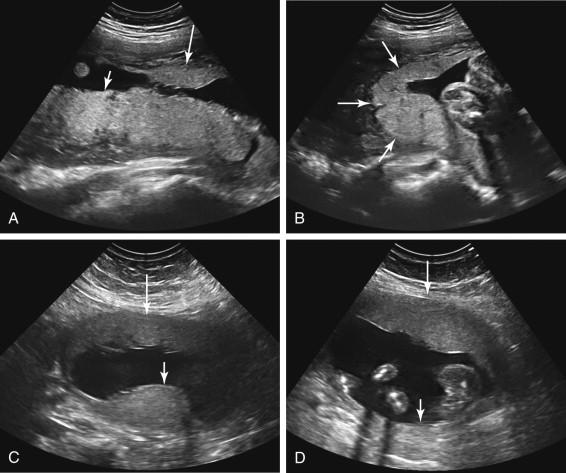
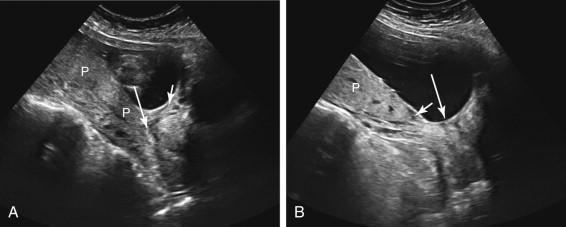
Succenturiate lobe is a common abnormality of placental configuration in which there are two or more distinct placental lobes with no placental tissue bridging the lobes ( Fig. 20-7A ). The umbilical cord inserts into the main placental lobe and the succenturiate lobe receives its blood supply from the main lobe (see Fig. 20-7B and C ). It is important to identify succenturiate lobes at antenatal sonography because if a succenturiate lobe is not expected at delivery, it may be inadvertently retained. The presence of a succenturiate lobe increases the risk of vasa previa (discussed below in the “ Umbilical Cord Insertion and Vasa Previa ” section of this chapter). In addition, a succenturiate lobe can implant directly over the cervix, resulting in placenta previa even when the main placental lobe is located at a distance from the cervix. Potential false positives for succenturiate lobe include imaging the anterior and posterior components of a normally shaped placenta that wraps around the lateral uterine wall ( Fig. 20-8A and B ) and mistaking a uterine contraction for a placental lobe (see Fig. 20-8C and D ).
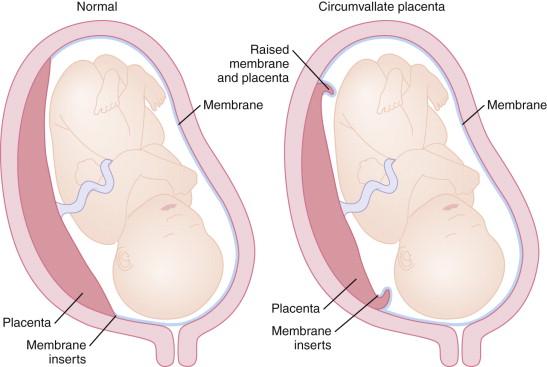
Circumvallate placenta occurs secondary to aberrant insertion of the amniochorionic membranes on the placenta. The membranes normally insert at the edge of the placenta, but in the setting of circumvallate placenta they attach to the anterior surface of the placenta, central to the placental edge ( Fig. 20-9 ). This results in a raised, rolled layer of thickened chorioamniotic membranes and placental tissue termed a placental shelf , in which the edge of the placenta exhibits a characteristic clublike appearance ( Fig. 20-10A ; ![]() ). In oblique scan planes, ultrasound depicts this layer as a linear band of tissue that can resemble a uterine synechia (see Fig. 20-10B ). Circumvallate placenta may be complete (affecting the entire margin of the placenta) or partial. Patients with complete circumvallate placenta are at increased risk of adverse perinatal outcomes such as fetal growth restriction, placental abruption, and preterm delivery.
). In oblique scan planes, ultrasound depicts this layer as a linear band of tissue that can resemble a uterine synechia (see Fig. 20-10B ). Circumvallate placenta may be complete (affecting the entire margin of the placenta) or partial. Patients with complete circumvallate placenta are at increased risk of adverse perinatal outcomes such as fetal growth restriction, placental abruption, and preterm delivery.
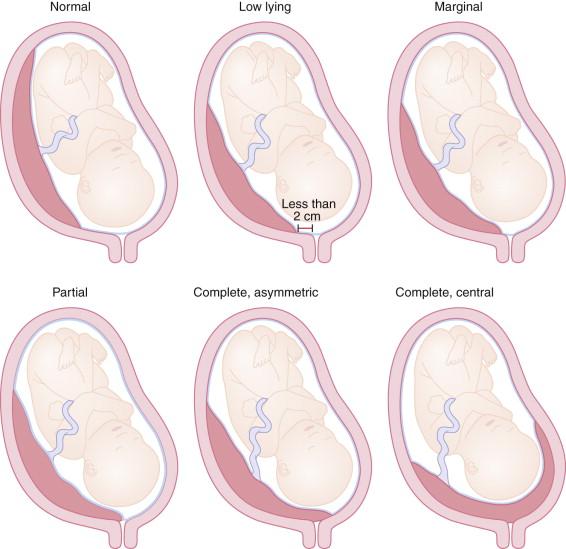
Placenta previa refers to placental tissue overlying the cervix. The classic clinical presentation is painless vaginal bleeding, although many patients are asymptomatic at the time ultrasound first reveals the abnormal placental location. Placenta previa is categorized by its severity. The classification varies among practices. A representative classification scheme is as follows: Complete placenta previa, internal cervical os completely covered by the placenta; partial placenta previa, internal cervical os partially covered by the placenta; marginal placenta previa, the placenta covers part of the internal surface of the cervix without overlying the internal cervical os; and low-lying placenta, distance between the inferior edge of the placenta and the internal cervical os less than 2 cm ( Fig. 20-11 ). The 2-cm threshold for a low-lying placenta was adopted because vaginal delivery is likely to be successful (assuming the absence of other problems) when the placental edge is located more than 2 cm from the internal os. Complete placenta previa is further subdivided into asymmetric complete placenta previa and central complete placenta previa. Asymmetric complete placenta previa occurs when the inferior edge of the placenta is eccentrically situated over the internal cervical os, completely covering the os but not extending significantly beyond the cervix. Central complete placenta previa indicates that the central portion of the placenta is implanted over the internal cervical os ( ![]() ). A common variation of the classification scheme excludes the partial placenta previa category because distinguishing between contiguous degrees of placenta previa (e.g., marginal placenta previa vs. partial placenta previa) may not be possible. The relationship of the inferior margin of the placenta to the cervical os may appear different in varying scan planes. For example, if placental tissue covers only the right side of the cervix, the right parasagittal view of the cervix will show placenta previa whereas the left parasagittal view of the cervix will not demonstrate placenta previa.
). A common variation of the classification scheme excludes the partial placenta previa category because distinguishing between contiguous degrees of placenta previa (e.g., marginal placenta previa vs. partial placenta previa) may not be possible. The relationship of the inferior margin of the placenta to the cervical os may appear different in varying scan planes. For example, if placental tissue covers only the right side of the cervix, the right parasagittal view of the cervix will show placenta previa whereas the left parasagittal view of the cervix will not demonstrate placenta previa.
The relationship between the inferior placental edge and the cervix may be assessed by transabdominal, transvaginal ( ![]() ), or transperineal ultrasound ( Figs. 20-12 to 20-14 ). Transvaginal sonography typically provides superior visualization, although transabdominal and transperineal ultrasound are often sufficient to diagnose or exclude placenta previa. The transperineal approach is also referred to as translabial ultrasound because it is performed with the transducer positioned on the perineum between the labia majora. The caudal portion of the cervix may be obscured by gas in the rectum at transperineal ultrasound (see Fig. 20-14 ). Transperineal ultrasound is typically used when transabdominal images are nondiagnostic and transvaginal ultrasound is undesirable (e.g., in the setting of ruptured membranes or when the cervix is fully dilated).
), or transperineal ultrasound ( Figs. 20-12 to 20-14 ). Transvaginal sonography typically provides superior visualization, although transabdominal and transperineal ultrasound are often sufficient to diagnose or exclude placenta previa. The transperineal approach is also referred to as translabial ultrasound because it is performed with the transducer positioned on the perineum between the labia majora. The caudal portion of the cervix may be obscured by gas in the rectum at transperineal ultrasound (see Fig. 20-14 ). Transperineal ultrasound is typically used when transabdominal images are nondiagnostic and transvaginal ultrasound is undesirable (e.g., in the setting of ruptured membranes or when the cervix is fully dilated).

It is important to directly image both the lower edge of the placenta and the cervix when assessing for placenta previa. A potential source of false negative for placenta previa occurs when the lower edge of the placenta is demonstrated to be superior to the expected location of the cervix, but the cervix is not imaged. Without direct visualization of the cervix it is not possible to exclude a succenturiate lobe of the placenta overlying the cervix.
A majority of potential placenta previas identified by ultrasound early in the second trimester resolve before delivery ( Fig. 20-15 ). This phenomenon was previously referred to as placental migration, but the term migration is potentially misleading because resolution of the placenta previa is not likely attributable to actual placental movement. A leading hypothesis is that resolution occurs secondary to disproportionate growth of the lower uterus, thereby increasing the distance between placental tissue and cervix. An alternate theory is that there is regression of placental tissue in poorly perfused areas and preferential growth in better vascularized regions, a phenomenon termed trophotropism. The later the scan is performed and the more severe the placenta previa, the more likely it will persist to term. When ultrasound reveals a potential placenta previa in the second trimester, follow-up scanning should be performed later in pregnancy.
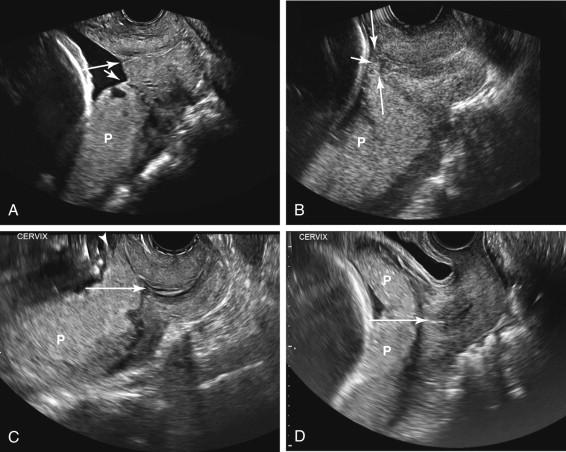
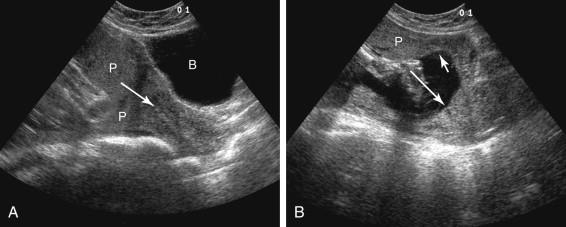
Additional etiologies for a false-positive diagnosis of placenta previa include a distended maternal urinary bladder, lower uterine contraction, and subchorionic hematoma overlying the cervix ( Box 20-3 ). A full bladder should not routinely be required for second and third trimester obstetric ultrasound because the cervix can be seen with an empty bladder. An overdistended maternal bladder potentially compromises the examination by compressing the cervix and lower uterus, giving the impression of an elongated narrow cervix. A normally located placenta in the lower uterus can then appear to cover the cervix ( Fig. 20-16A ). If there appears to be a placenta previa when the bladder is full, the examination should be repeated after emptying the bladder (see Fig. 20-16B ). Unfortunately, emptying the bladder often causes a lower uterine contraction, further confounding assessment for placenta previa.
Distended maternal urinary bladder
Lower uterine contraction
Subchorionic hematoma overlying the cervix
Ultrasound examination during the first or second trimester
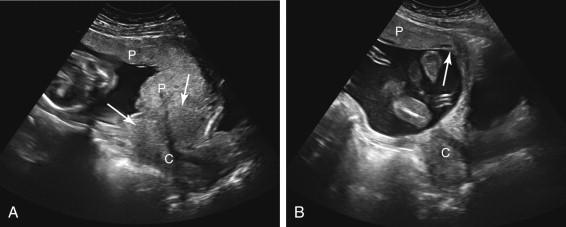
Asymptomatic uterine contractions are frequently depicted by ultrasound in normal pregnancies. A contraction in the lower uterus typically exhibits a circumferential configuration, narrowing the lower uterine cavity and pulling placental tissue into the inferior portion of the uterus. When the opposing sides of a circumferential contraction come into contact with each other, a linear region that resembles an endocervical canal may be seen, simulating the appearance of cervix covered by placenta ( Fig. 20-17A ). This pitfall should be suspected when the apparent cervix appears distorted and elongated with bulging upper margins, an appearance seen when both the cervix and adjacent contraction have been imaged together. In contrast, in the absence of a contraction, the normal cervix has a cylindrical configuration with a relatively flat upper surface. Delayed imaging once the contraction has resolved shows the inferior edge of the placenta above the cervix, confirming that the apparent placenta previa was due to a uterine contraction (see Fig. 20-17B ).
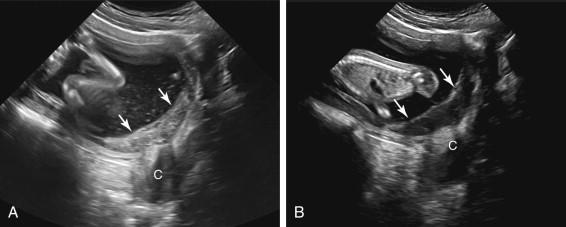
Subchorionic hematoma is an uncommon etiology for a spurious appearance of placenta previa. This pitfall occurs when the hematoma overlies the cervix and is imaged in an acute stage while it is echogenic, resembling the echotexture of placental tissue extending over the cervix ( Fig. 20-18A ). Color Doppler aids in distinguishing placental tissue from subchorionic hematoma, depicting vascularity in the placenta but not in a hematoma. Follow-up ultrasound depicts interval evolution in the echotexture of hematoma to a less echogenic appearance but little change in appearance of placental tissue (see Fig. 20-18B ).
Placenta accreta is characterized by abnormal adherence of the placenta to the uterus secondary to abnormally deep placental attachment. It is classified into the following three categories in order of increasing severity: placenta accreta, placenta increta, and placenta percreta. The term placenta accreta has dual usages, describing both the overall process of abnormal placental adherence and the specific case of the mildest form of abnormal placental attachment in which the placenta penetrates the decidua but does not invade the myometrium. Placenta increta is characterized by the placenta invading the myometrium, without involving the serosa. Placenta percreta is the most severe form, in which placental tissue penetrates through the myometrium into the serosa. Placenta percreta can invade adjacent organs, most commonly the urinary bladder.
Risk factors for placenta accreta include uterine surgery, instrumentation, and placenta previa. Cesarean section is a particularly important risk factor. The likelihood of placenta accreta increases exponentially with each additional cesarean section. The combination of prior cesarean section and an anterior placenta previa extending over the cesarean section scar is particularly concerning. It is important to assess for placenta accreta in patients at increased risk because failure of the placenta to separate normally from the uterus at delivery may lead to severe life-threatening hemorrhage necessitating emergency hysterectomy. With prior knowledge of placenta accreta, delivery strategies can be planned to decrease perinatal morbidity and mortality.
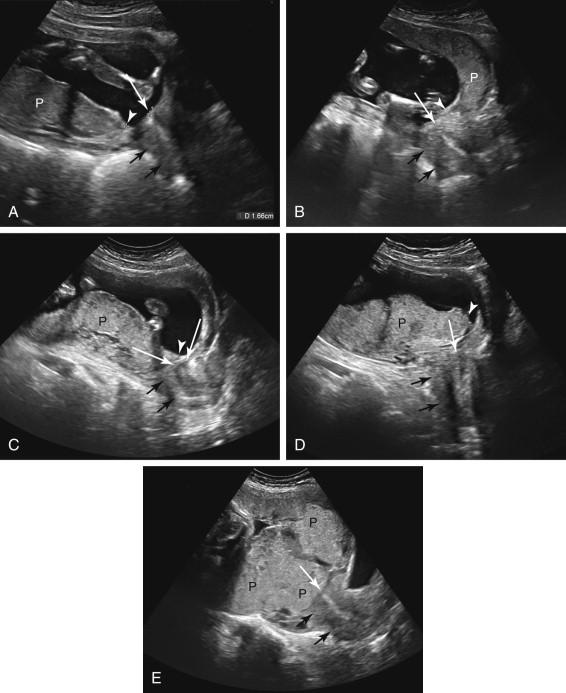
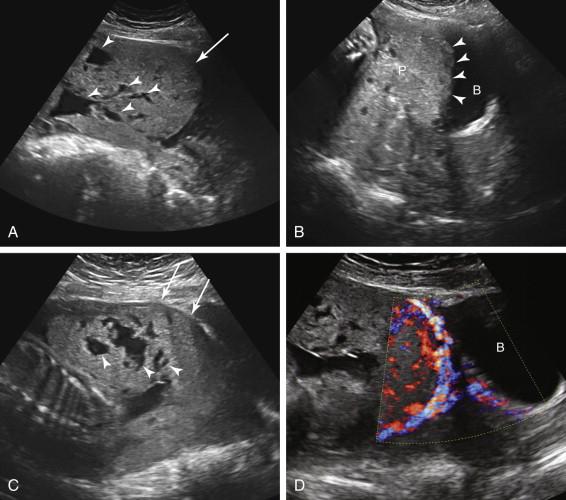
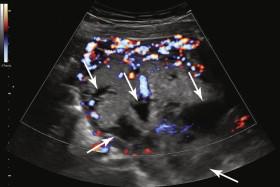
Ultrasound findings of placenta accreta include placental lacunae, increased intraplacental and retroplacental vascularity, thickening and bulging of the placenta toward the bladder, nonvisualization or reduced thickness of the myometrium underlying the placenta, disruption or loss of the echogenic uterine serosa-bladder interface, irregular outpouchings of placental tissue into the bladder, and loss of the normal hypoechoic retroplacental space ( Box 20-4 and Fig. 20-19 ). A full bladder is helpful in assessing the bladder for invasion by placenta percreta. Placental lacunae correspond to irregularly shaped vascular spaces with turbulent flow in the placenta and have been reported to be the most predictive ultrasound finding of placenta accreta. They frequently exhibit flow at color Doppler or on gray-scale cine clips ( ![]() ; e-Fig 20-1
; e-Fig 20-1 ![]() ). Lacunae are distinguished from normal intervillous spaces in the placenta by their larger size and number and irregular configuration, sometimes resulting in a Swiss cheese appearance to the placenta. Lacunae tend to become more prominent as pregnancy progresses. Placenta accreta should not be diagnosed based solely on loss of the normal hypoechoic retroplacental space, particularly in low-risk patients because demonstration of this space is dependent on scan plane and it is not always seen behind the normal placenta. Loss of the hypoechoic retroplacental space is best used as a supporting feature when seen in the appropriate clinical setting in conjunction with other suggestive ultrasound findings of placenta accreta.
). Lacunae are distinguished from normal intervillous spaces in the placenta by their larger size and number and irregular configuration, sometimes resulting in a Swiss cheese appearance to the placenta. Lacunae tend to become more prominent as pregnancy progresses. Placenta accreta should not be diagnosed based solely on loss of the normal hypoechoic retroplacental space, particularly in low-risk patients because demonstration of this space is dependent on scan plane and it is not always seen behind the normal placenta. Loss of the hypoechoic retroplacental space is best used as a supporting feature when seen in the appropriate clinical setting in conjunction with other suggestive ultrasound findings of placenta accreta.
Placental lacunae
Increased intraplacental and retroplacental vascularity
Thickening and bulging of the placenta toward the bladder
Nonvisualization or reduced thickness of the myometrium underlying the placenta
Disruption or loss of the echogenic uterine serosa-bladder interface
Outpouchings of placental tissue into the bladder
Loss of the normal hypoechoic retroplacental space (supporting feature that is dependent on scan plane)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here