Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the 1990s, diffusion-weighted imaging (DWI) has revolutionized the diagnosis of acute cerebral infarction, making it possible for patients to receive thrombolytic agents in emergency situations and escape death or severe chronic invalidity. This life-saving potential prompted manufacturers to rapidly incorporate diffusion magnetic resonance imaging (MRI) into their commercial products. On the other hand, DWI has also shown great potential to manage cancer lesions. Cerebral infarction and cancer have in common a decrease of the apparent diffusion coefficient (ADC, the standard biomarker of diffusion MRI; see Chapter 1 ), although the mechanisms (reduction of the extracellular space, cell proliferation in cancer, diffusion hindrance increase) are still under investigation. This means that stroke and cancer lesions appear as high-signal areas in DWI. However, DWI is much more difficult to use outside the brain because of its sensitivity to bulk motion. Especially in the torso and the abdomen, cardiac and respiratory motion can be a source of strong artifacts in DWI. Such artifacts can be mitigated in some ways, for instance, by using breath-hold. Therefore DWI of the body was always performed under the limitation of breath-hold and as a result greatly suffered from low signal-to-noise ratio (SNR).
Diffusion-weighted whole-body imaging with background body signal suppression (DWIBS) is the name of a DWI approach that intentionally uses free breathing scanning rather than breath-holding or respiratory triggering to visualize (moving) visceral organs. Similar to standard DWI, DWIBS also uses echo-planar imaging (EPI; see Chapter 12 ) with a fat-suppression technique, typically short tau inversion recovery (STIR). Another issue in the body is the presence of fat, as fat usually exhibits very low ADC and can contaminate fibroglandular tissue diffusivity measures and be misinterpreted as malignancy. Hence efficient fat suppression must be used in combination with EPI. The multiple signal acquisitions necessary to encode imaging render macroscopic motion incoherent across scans, but single-shot MRI encoding methods such as EPI can alleviate those motion artifacts. In principle, only random motion (incoherent motion) affects the contrast of DWI and not constant linear motion (coherent motion), such as respiratory motion. DWIBS uses this principle. Free breathing scanning allows for the acquisition of a thin-sliced data set (suitable for multiplanar reformats and maximum intensity projections [MIPs]) with a large anatomical coverage within a clinically reasonable scan time. Note that these targets cannot be achieved when using a breath-hold or respiratory-triggered DWI acquisition. The advent of DWIBS is similar to that of multislice CT around the year 2000 when arbitrary multiplanar reconstructions and MIPs could be obtained. The DWIBS method also relies on the MIP approach to display the distribution of cancer lesions in 3D or arbitrary multiplanar reformats ( Fig. 11.1 ). The latter is similar to fluorodeoxyglucose (FDG)-positron emission tomography (PET), which also provides a generally high lesion-to-background contrast and where MIP images can be used to detect pathology at a single glance. The use of MIP images can speed up image evaluation and may perhaps increase sensitivity, because they rapidly pinpoint potential lesions that can then be further inspected on 2D source images and other sequences. Reversing the black and white contrast of a DWIBS data set yields an image that resembles the standard (FDG-)PET view (i.e., lesions appear black and background appears white), which may be visually convenient to those readers who are accustomed to the standard (FDG-)PET view. Nevertheless, reversing the black and white contrast is only a matter of habituation and personal taste and is unlikely to affect diagnostic performance.

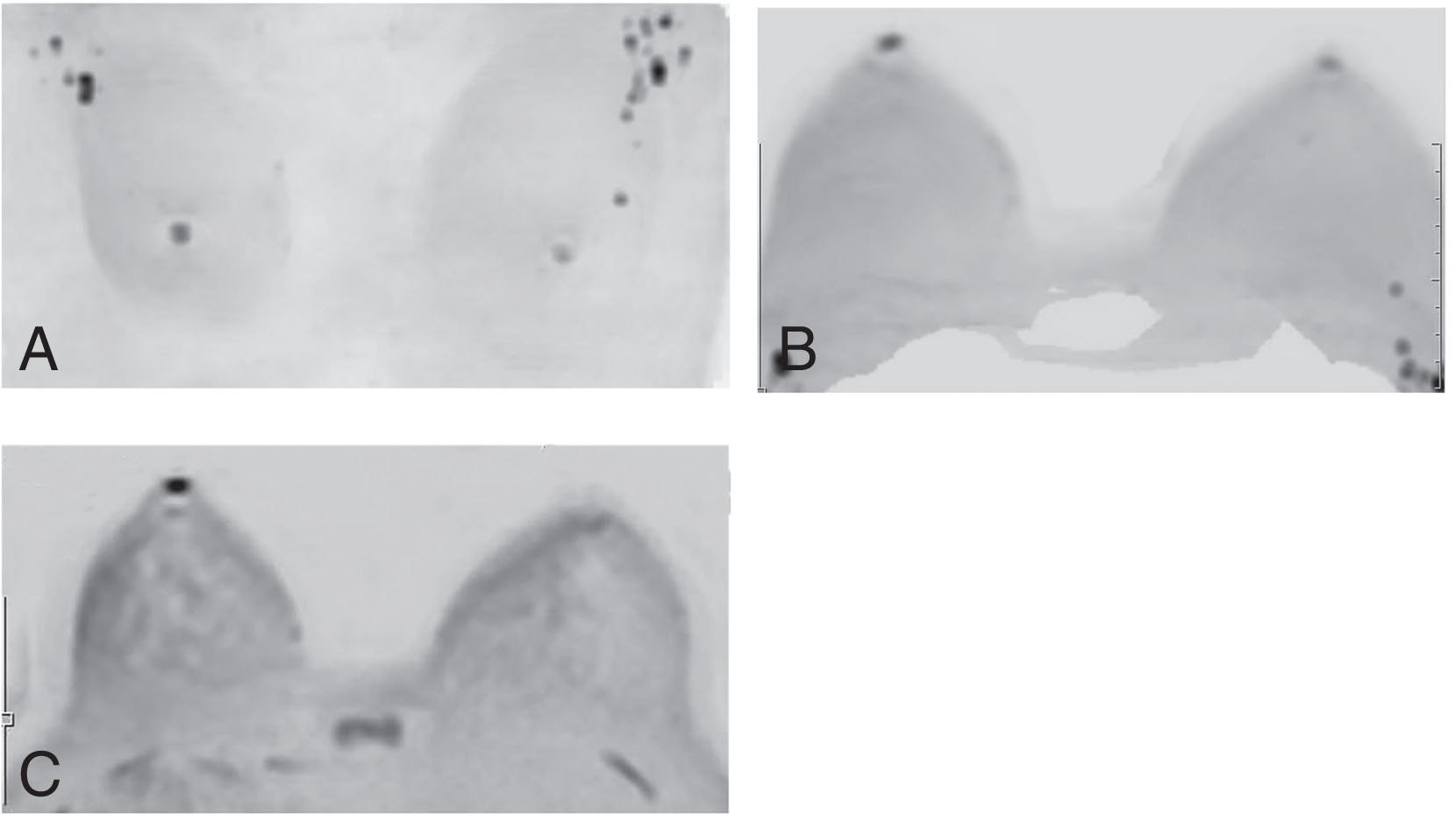
The DWIBS method has proven versatile and easy to implement. It has been incorporated into clinical protocols and used to identify cancerous lesions, evaluate treatment strategies for bone metastases of prostate cancer, and is part of some imaging evaluation methods such as ONCO-RADS. It is generally less expensive than (FDG-)PET and Positron emission tomography–computed tomography (PET-CT). It does not involve radiation exposure, making it a suitable method for a follow-up study of cancer treatment. Because breast cancer is a disease with a high incidence of bone metastases, DWIBS is often used for screening across the whole body. Recently, ADC color maps have been added to DWIBS to aid in lesion characterization and treatment selection ( Fig. 11.2 ).

The contrast principle of the DWIBS method is described in the previous section. To obtain a wide coverage of the torso, it is necessary to achieve good fat suppression in any part of the body. In general, in 2D images (e.g., axial images), insufficient fat suppression at the edges of the field of view is rarely a diagnostic problem. However, poorly suppressed superficially located fat can seriously deteriorate the MIP image and obscure lesions.
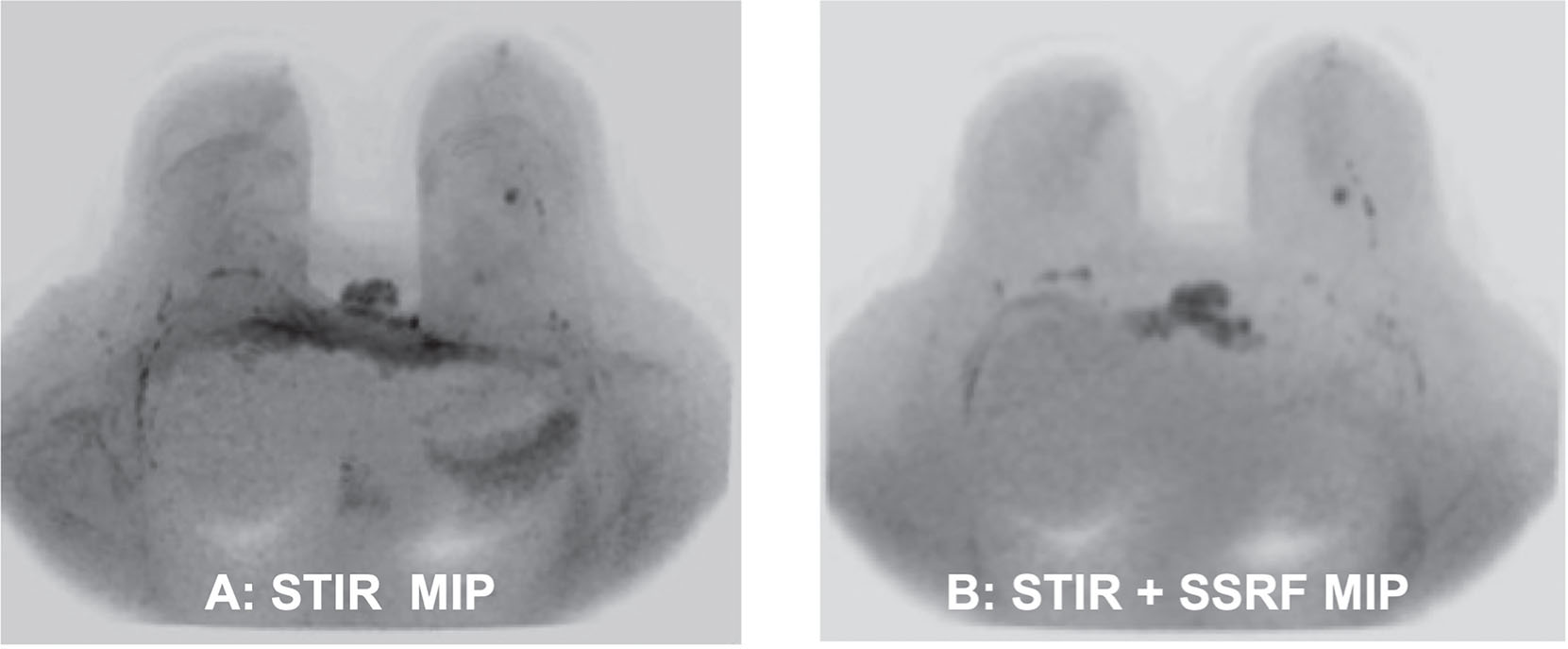
Among fat-suppression techniques (see Chapter 12 ), such as STIR, chemical shift selective (CHESS) or spectral attenuated inversion recovery (SPAIR), the use of STIR has shown to be effective for homogeneous fat suppression ( Fig. 11.3 ), although both STIR and SPAIR techniques showed similar diagnostic performances for ADC-based differentiation of malignant from benign breast tumors, and SPAIR is recommended in breast DWI by the latest consensus statement of the European Society of Breast Imaging (EUSOBI).
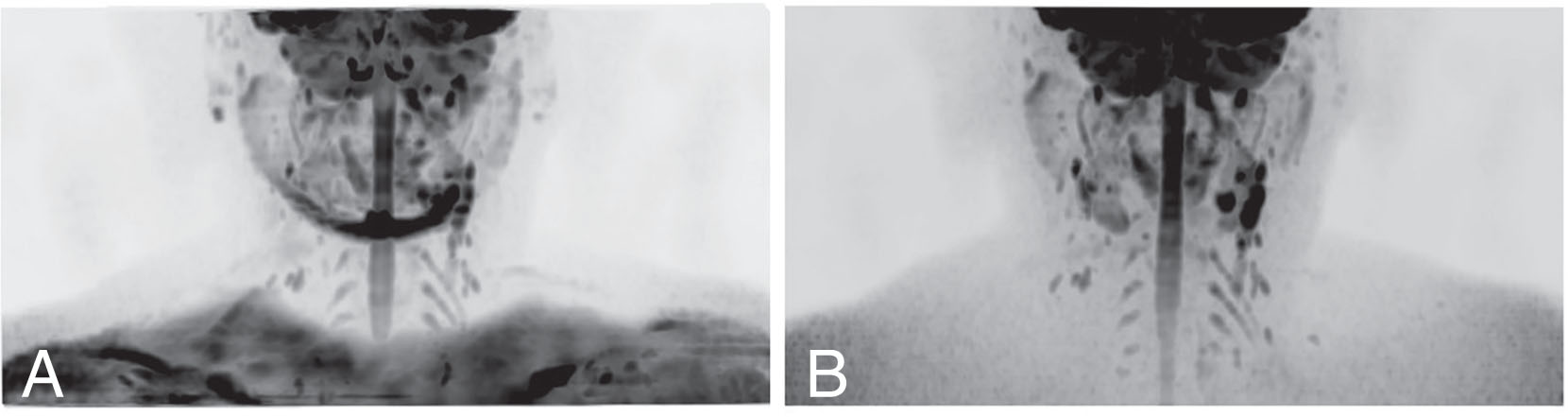
The breast has a spatially complex shape, and the breast cleavage and nipple area are prone to local magnetic field heterogeneities. The STIR method, which relies on T1 differences between fat and tissues, is more robust than CHESS, which is based on the fat/water frequency difference, particularly for the superficial regions of the breast. Fig. 11.4 shows a DWI of a breast performed with the commonly used fat-suppression method (CHESS). The MIP image looks clear at a first glance (pseudotransparent effect), but it is important to note that the signal intensity of the surface fat is dominant, and the interior is not visible.
Even with STIR, the fat-suppression effect may not be perfect. There are two potential options to enhance fat suppression in STIR: spatial-spectral radiofrequency (SSRF; Fig. 11.5 ) or slice selective gradient reversal (SSGR). Although SSGR has the advantage of no trade-offs, it is susceptible to magnetic field inhomogeneity, and it is generally more prone to failure when used for the breast region, so its use requires extreme caution.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here