Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
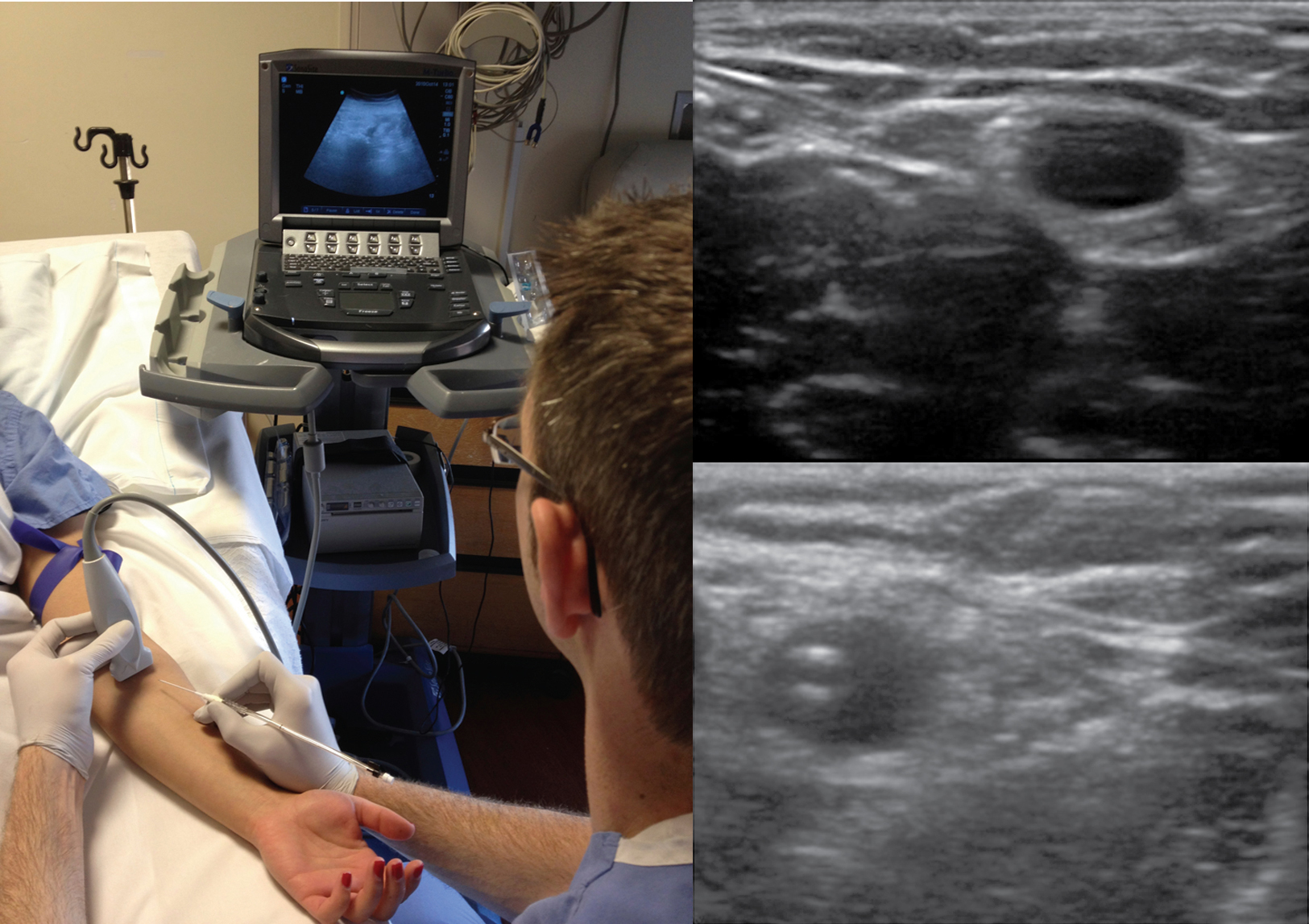
Ultrasound guidance to obtain vascular access has become increasingly more popular over the past decade. Advances in ultrasound technology have enhanced its ability to detect and interrogate smaller vascular structures for cannulation purposes. Given the potential complications that can develop when accessing central veins, practitioners have turned to ultrasound-guided peripheral access. Although no invasive procedure is without risks, the relative array of complications potentially produced by peripheral, non–centrally extending venous lines tend to be significantly less severe than those from central venous access. This chapter outlines the indications, risks, and benefits of ultrasound-guided, noncentral peripheral intravenous (IV) access.
The standard limitations described with landmark-based IV catheter placement can be overcome given the advances in visualization brought to the bedside with ultrasound. With regard to operators, emergency physicians, anesthesiologists, nursing staff, intensivists, and their respective trainees have reported peripheral IV cannulation success rates of higher than 85%. With regard to risk for infection, Maki et al reported that peripheral IV catheters in general maintain lower infection rates than do any other forms of IV access. Additionally, when complications did occur, they tended to not be as morbid as those associated with central venous catheters.
Despite such a successful track record of placement and safety, limited data exist on the role of ultrasound-guided peripheral IV access in patients in the intensive care unit (ICU). One of the reasons for this is that many medications should not be administered through peripheral access given their potentially damaging effects on veins (e.g., certain vasopressors, total parenteral nutrition [TPN]). In another report, medications such as vancomycin or phenytoin were suggested to be associated with increased rates of thrombophlebitis. Aside from these relative contraindications, a question remains: in patients who do not need central venous access, are ultrasound-guided peripheral IV techniques reliable enough to allow increased avoidance or removal of central lines in the critically ill? Gregg et al were able to achieve ultrasound-guided peripheral venous access in 99% of patients who failed standard landmark attempts at placement. Among the diverse group of trauma, postsurgical, and cardiac intensive care patients, 34 central lines were avoided and 40 were removed as a result of adequate peripheral access. In a small randomized controlled trial, Kerforne et al also demonstrated increased success rates of ultrasound-guided peripheral IV access over the landmark technique in critical care patients who were deemed to have difficult access. Despite reports of relatively low complication rates with ultrasound-guided peripheral IV access in the ICU, no trials have directly compared rates of infection or thrombophlebitis with the use of ultrasound-guided versus landmark techniques.
Different techniques for placing peripheral IV catheters have been described. One-person operation of the ultrasound transducer while placing the IV line has the benefit of allowing the entire procedure to be performed by a single party. However, applying appropriate skin tension when limited to a single hand to perform the insertion has the potential to be awkward. This has led to reports of a two-person technique that involves an ultrasound operator and an IV operator working together throughout the placement procedure. Chinnock et al showed that the number of operators placing the IV line was not predictive of successful placement, and a variety of other studies describing either a one- or two-person technique have shown successful placement more than 85% of the time. Another variation in equipment described includes the use of guidewire assistance. Guidewire-assisted vascular access devices have traditionally been used when attempting arterial access; however, given their ease of use, successful single-operator cannulation rates higher than 95% can be achieved. The limitation of catheters with wires that are preloaded onto the device is that the IV lines tend to come in limited diameters. To overcome this shortcoming, Sandhu and Sidhu described a technique that allows upsizing an access catheter to a larger-bore one by means of exchanging the device over a free wire. It is this author’s preference to use wire-assisted devices for single-operator placement of peripheral IV lines when larger-bore access is not necessary.
In summary, ultrasound-guided peripheral IV lines are an attractive access option since they have been shown to have low procedure-related morbidity while avoiding the possible complications associated with central venous catheters. Future challenges for this approach to IV access include the widespread availability of ultrasound and standardized education of all levels of practitioner.
A 40-year-old man underwent total pancreatectomy for chronic pancreatitis. His postoperative complications included hemorrhagic shock, multisystem organ failure, and an enterocutaneous fistula. The patient eventually recovered, successfully completed rehabilitation, and was being maintained on outpatient TPN. He was seen multiple times with recurrent bacteremia as a result of peripherally inserted central venous catheter infections. The intravenous nurse was unable to gain access through landmark techniques, and a new central line was suggested. Given the patient’s ongoing fevers and chills and evidence of persistent bacteremia, ultrasound was used to assess the patency of other peripheral veins. Multiple veins were visualized with tourniquet placement, and two peripheral IV lines were placed for administration of antibiotic. The central line was removed and the patient’s bacteremia cleared. When readmitted to the hospital after some time for line infections, additional IV lines were placed without complication. The patient’s enterocutaneous fistula was eventually repaired surgically 1.5 years following his first operation, and TPN was stopped.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here