Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tomosynthesis will alter the clinical practice of diagnostic mammography. The standard diagnostic work-up of noncalcification lesions can be markedly abbreviated because fewer diagnostic views are required for lesion confirmation, characterization, and localization. Many patients, particularly those with masses, can proceed directly from routine tomosynthesis views to ultrasound, avoiding additional diagnostic mammographic views altogether. Although the value of tomosynthesis in the work-up of calcifications has not been well established, early clinical experience has shown tomosynthesis to be helpful in evaluating some types of calcifications. This is especially true for benign calcifications, such as early vascular, dermal, and dystrophic calcifications, in which tomosynthesis can reveal pathognomonic benign features that may be difficult to perceive on conventional two-dimensional (2 D ) mammographic views.
As in screening mammography, the improved visualization of lesion characteristics aids in achieving both greater sensitivity and specificity in the diagnostic setting. Both benign and malignant lesions can be assessed more accurately and with greater diagnostic confidence. For example, the subtle pseudocapsule of a hamartoma, which may be obscured by overlying dense breast tissue on 2D mammography, can be unveiled on tomosynthesis slices. Similarly, the spiculated margin or associated architectural distortion of a mass surrounded by dense breast tissue is often dramatically displayed on tomosynthesis, confirming a high probability of malignancy in a lesion that may otherwise be perceived as indeterminate. The exquisite sensitivity of tomosynthesis for fine detail can also reveal features within and surrounding breast cancers that could not be appreciated with conventional 2D mammography alone. For example, some breast cancers are shown to contain intralesional fat, which should not be misinterpreted as a sign of benignity.
In the conventional 2D diagnostic mammography environment, spot compression views are an essential diagnostic tool. By dispersing fibroglandular tissue within an area of interest, spot compression views are particularly useful in differentiating a mammographic density created by tissue overlap from a true lesion. Spot compression views help to characterize a true lesion by improving visualization of features, including mass margins. By reducing the masking effect of overlying breast tissue, tomosynthesis imaging precludes the need for many of the additional diagnostic views traditionally used in diagnostic mammography. Lesion features can often be assessed without obtaining spot compression or rolled, tangential, and other views ( Fig. 6.1 ).

After implementing tomosynthesis, the number of diagnostic views required to reach a final assessment in screening recalls should be significantly reduced. Patients recalled from tomosynthesis screening typically require fewer additional views and more commonly proceed directly to ultrasound for an ultrasound-only work-up. This is particularly true for patients recalled for masses, in which standard craniocaudal (CC) and mediolateral oblique (MLO) tomosynthesis views often clearly reveal mass margins without the need for additional views. Despite the abbreviated diagnostic work-up, specificity can be maintained or even increased.
Among patients imaged in the diagnostic environment for reasons other than a screening recall, such as a clinical symptom or a Breast Imaging Reporting and Data System (BI-RADS) 3 follow-up, the number of additional views performed should also decrease. Diagnostic studies beginning with routine tomosynthesis MLO and CC views require fewer additional views, with the number of both spot compression views and even magnification views substantially reduced ( Table 6.1 ).
| 2D Mammography | 2D Mammography Plus Tomosynthesis |
|---|---|
| Spot compression Magnification True lateral Exaggerated craniocaudal Rolled craniocaudal Step oblique Tangential |
Spot compression Magnification (for calcifications) |
The improved visualization of lesion features, such as mass shape and margins, facilitates a more accurate diagnostic assessment of the probability of malignancy. Cancers appearing mostly circumscribed or obscured on 2D images may be shown to have spiculated margins on tomosynthesis slices. Even small focal asymmetries may be revealed to represent suspicious masses on tomosynthesis ( Fig. 6.2 ). The fine detail visible with tomosynthesis reduces the likelihood that a cancer would be missed or misinterpreted as a probably benign or benign finding.
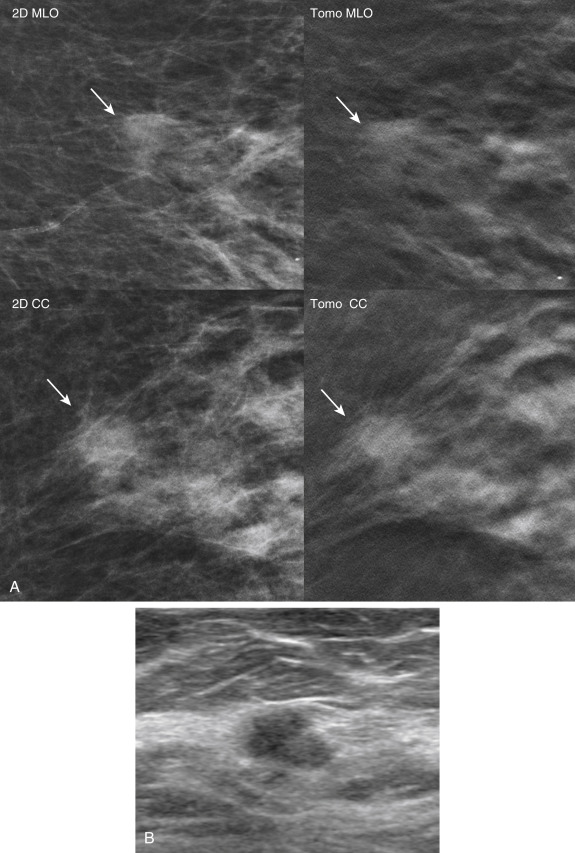
Breast cancers are often more conspicuous on routine tomosynthesis CC and MLO views compared with 2D spot compression views, and some cancers are seen only on tomosynthesis. Indeed, in some cases, a 2D spot compression view may result in a false negative final interpretation. A cancer initially seen on tomosynthesis can appear to disperse on 2D spot compression, suggesting that the questioned lesion represented tissue overlap. In these cases, tomosynthesis shows the suspicious lesion more reliably than additional 2D views do and appropriately leads the work-up toward further evaluation and biopsy ( Fig. 6.3 ).

Multiple authors have shown that diagnostic evaluation with routine tomosynthesis views could achieve equivalent or superior sensitivity and specificity compared with conventional 2D supplemental views. When combined with tomosynthesis, routine MLO and CC views may be sufficient in the diagnostic evaluation of the majority of abnormal findings, thereby replacing the conventional diagnostic work-up. Zuley et al. demonstrated that tomosynthesis CC and MLO views could not only replace supplemental diagnostic views but could actually improve diagnostic accuracy compared with a conventional diagnostic work-up of noncalcified abnormal lesions recalled from screening mammography. In this study there was a significant reduction of false-positive cases placed in the BI-RADS 4 and 5 categories, and a greater number of cancers placed in the BI-RADS 5 category when using tomosynthesis.
With more benign lesions placed in the BI-RADS 1 and 2 categories and more cancers placed in the BI-RADS 4 and 5 categories, a steady decline in BI-RADS 3 assessments, as well as an increase in the positive predictive value for biopsies (PPV3), may be seen with tomosynthesis. This improved accuracy in the assessment of benign and malignant lesions reflects both a higher sensitivity and specificity. For cases still assessed as BI-RADS 3 using tomosynthesis, the mammographic work-up at a 6-month follow-up may be abbreviated because fewer views are likely to suffice.
A mass, architectural distortion, or asymmetry may be obvious on both the 2D mammogram and tomosynthesis, may be subtle on the 2D mammogram but seen well on tomosynthesis, or may be difficult to perceive and characterize even on tomosynthesis. When the lesion is obvious, the diagnostic work-up can usually begin with targeted ultrasound. In such cases the routine views with tomosynthesis provide sufficient information regarding lesion location and features such that spot compression and 90-degree true lateral views are unnecessary ( Fig. 6.4 ). When skipping the true lateral view and going straight to targeted ultrasound, it is important to remember that lesions located far medially or laterally will be located more superiorly or inferiorly, respectively, than depicted on the MLO view. When an ultrasound correlate is seen, the lesion can be determined to be benign, probably benign, or suspicious and is managed accordingly.

If a lesion is subtle on both 2D and tomosynthesis, a diagnostic work-up is helpful prior to targeted ultrasound. Unlike a conventional diagnostic work-up in which spot compression is often performed in two views, a single tomosynthesis spot compression view usually suffices to distinguish between tissue overlap versus a true lesion and, when a true lesion is present, to provide adequate margin detail. Occasionally a very subtle lesion will require tomosynthesis spot compression in two views. For such subtle lesions a small spot compression paddle may be helpful to optimize visualization.
If there is uncertainty that a sonographic finding definitively correlates with the mammographic finding, a metallic marker (BB) can be placed on the skin overlying the lesion during the ultrasound examination, and tomosynthesis spot compression views can be obtained. If the sonographic and mammographic findings are the same, the BB should be in the vicinity of the mammographic finding. Because the BB is placed on the skin and not directly on the lesion and the patient is positioned differently during mammography and ultrasound, the BB may not be directly overlying the mammographic finding. Caution must be exercised to ensure that the two lesions match not only in terms of location but also in terms of size, appearance, and level of suspicion. For suspicious ultrasound lesions that proceed to biopsy, placement of a biopsy clip and post-biopsy mammography with tomosynthesis are paramount to confirm correspondence of the biopsied ultrasound lesion with the original tomosynthesis finding.
When performing spot compression views with tomosynthesis, the question often arises whether to acquire only tomosynthesis or a combination of 2D imaging and tomosynthesis. When a lesion is best seen on tomosynthesis, a tomosynthesis-only spot compression view may suffice. However, a combination spot compression view using both 2D imaging and tomosynthesis is often beneficial because the 2D component allows better identification of nearby landmarks, ensuring that the appropriate region of the breast is included in the spot compression window. This may be particularly helpful in patients with large breasts. To reduce patient radiation exposure, synthesized 2D spot compression allows similar assessment of nearby landmarks and can replace the traditional 2D component of the combination spot compression. Importantly, a cancer may be visible only on tomosynthesis, and 2D spot compression views alone without tomosynthesis can be misleading. A suspicious finding seen on tomosynthesis should not be dismissed as benign if not reproduced on 2D spot compression views alone ( Fig. 6.5 ).
If a subtle suspicious finding is seen on tomosynthesis and requires further evaluation, spot compression views with tomosynthesis are advised because some malignancies will not be reproduced on 2D spot compression alone.

On 2D mammography, findings requiring additional evaluation may occasionally be seen in only one view. In these cases a number of additional diagnostic views are helpful in the diagnostic work-up. For example, when a possible lesion is initially seen only in the CC view, rolled CC views can be obtained to determine whether the lesion is located in the superior or inferior breast, thereby localizing it to a specific quadrant. Similarly, to triangulate a lesion initially seen only in the MLO view, true lateral or step oblique views can be performed to localize the lesion in the three-dimensional (3D) space. Precise lesion localization is important to exclude the possibility of summation artifact and to accurately direct targeted ultrasound. With the ability to localize a lesion within single, thin sections of breast tissue, tomosynthesis can eliminate the need for additional diagnostic work-up of lesions initially seen in only one view.
In the case of a lesion seen only in the CC view, scrolling through the breast from superior to inferior will identify the tomosynthesis slice(s) containing the lesion and pinpoint its location within the superoinferior dimension ( Fig. 6.6 ). By knowing the location of the slice in the CC plane, the reader can determine the location of the lesion. Likewise, in the case of a lesion seen only in the MLO view, scrolling through the thickness of the breast from lateral to medial will identify the slice(s) where the lesion is best visualized. Thus even lesions seen in only one of the routine views can typically be localized in 3D space and accurately targeted by ultrasound without the need for additional views.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here