Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chapter 3 , pp. 35–46 : Skull—suspected NAI.
Chapter 6 , pp. 92–93 : Shoulder.
Chapter 7 , pp. 95–114 : Elbow.
Chapter 13 , pp. 214–215, 224–226 : Pelvis.
Chapter 17 , pp. 298, 304–305 : Foot.
Chapter 21 , pp. 350–351, 358–359 : Swallowed foreign bodies.
“A child is not a small adult …” This truism is particularly important in relation to paediatric bone injuries
There are three major differences between a child's and an adult's skeleton .
Children have growth plates that:
have the consistency of hard rubber and act, in part, as shock absorbers
protect the joint surface from sustaining a comminuted fracture
are weaker than the ligaments. Consequently the epiphysis will separate before a dislocation (ie ligamentous disruption) occurs.
Children have a thick periosteum that:
is not only thick but very, very, strong
acts as a hinge, which inhibits displacement when a fracture occurs.
Children's bones have an inherently different structure to adults' bones, being:
less brittle
flexible, elastic, and plastic, allowing an injured bone to bend or to buckle.
You need to be familiar with the normal radiographic appearance of the ends of the long bones in children. This will help you to detect the important injuries and will also protect you from labelling a normal developmental appearance as being abnormal.
A child's long bone grows in length initially by forming layers of cartilage and gradually converting that cartilage into bone. This layering process takes place at the end of the bone at the site of the physis (also called the epiphyseal plate or the growth plate). The physis is made of cartilage and lies between the epiphysis and the diaphysis. Cartilage is lucent on a radiograph. The cartilaginous physis remains as a radiographic lucency until the child reaches skeletal maturity and stops growing. At that time the lucent physis fuses to the metaphysis (and also to the epiphysis). When fusion occurs the linear lucency that was the physis disappears.
An epiphysis is a secondary centre of ossification at the end of a long bone. Each epiphysis is initially composed solely of cartilage. As a consequence it looks as though nothing is there (take a look at a new born baby's elbow region). Of course each of the epiphyses is present, but present as a radiolucent blob of cartilage. These invisible blobs enlarge slowly with age. Eventually they begin to ossify at their centres and become visible. Finally, these blobs of bone will fuse to the physis at maturity.
“The key to accurate diagnosis is a precisely accurate assessment of the radiographs.”
The growth plate (the physis) is a very vulnerable structure. The joint capsule, the surrounding ligaments and the muscle tendons are all much stronger than the cartilaginous physis.
A shearing or avulsion force applied to a joint is most likely to result in an injury at the weakest point, ie a fracture through the growth plate.
Most growth plate injuries will heal well without any resultant deformity. However, in a few patients, failure to recognise a growth plate injury may result in suboptimal treatment with a risk of premature fusion resulting in limb shortening. If only a part of the growth plate is injured, unequal growth may lead to deformity and disability.
This classification links the radiographic appearance of the fracture to the clinical importance of the fracture. A Salter–Harris type 1 injury has a good prognosis whereas a Salter–Harris type 5 injury has a poor prognosis.
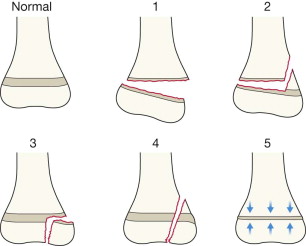
Type 1 is a fracture restricted to the growth plate.
Types 2–4 represent various patterns of fracture involving the growth plate and the adjacent metaphysis and/or epiphysis.
Type 5 is an impaction fracture of the entire growth plate.
| Type | Relative frequency | Prognosis for normal growth | |
|---|---|---|---|
| Upper limb | Lower limb | ||
| 1 | 8% | Satisfactory | The likelihood of a growth complication is higher for all types of Salter–Harris injury as compared with the upper limb. |
| 2 | 73% | Satisfactory | |
| 3 | 6% | Satisfactory | |
| 4 | 12% | Guarded | |
| 5 | 1% | Poor | |
| SH 1 | = S | is Separated (a widened physis) |
| SH 2 | = A | is Above the growth plate |
| SH 3 | = L | is beLow the growth plate |
| SH 4 | = T | is Through the growth plate |
| = E | is for nothing! | |
| SH 5 | = R | has a Rammed together growth plate |

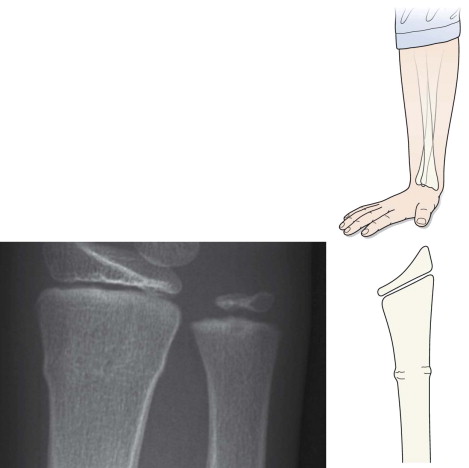
Fracture restricted to the growth plate. In this patient the epiphysis is displaced posteriorly.
Note: Many type 1 fractures do not show displacement of the epiphysis, making it impossible to detect the injury to the growth plate from the radiographs. Prognosis in these cases is invariably very good.
Impaction fracture of the entire growth plate. There is little or no malalignment and it is usually impossible to make the diagnosis on the initial radiographs. This is the most significant of the Salter–Harris injuries. The plate may fuse prematurely with consequent limb shortening. The diagnosis, and consequently optimal management, depends on a high degree of suspicion following clinical examination.
When a child's long bone is subjected to a longitudinal compression force (such as a fall on an outstretched hand), this can result in two common but different types of injury in the region of the metaphysis and proximal diaphysis.
Torus fracture
Greenstick fracture
Results from a longitudinal compression force with little or no angulation. The axial loading is distributed evenly across the metaphysis (right). There are microfractures of the trabeculae at the injured site.
The commonest sites for a torus fracture are the distal radius and/or ulna.
The fracture is often subtle and appears as a ripple, a wave, an indent or a slight bump/bulge in the cortex. The bulge may be seen at both cortices or at one cortex only.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here