Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anesthesiologists commonly encounter bleeding during and after surgery, which can impact perioperative outcomes, even increasing morbidity and mortality. The most common approach to managing a bleeding patient is by transfusing blood products. Nevertheless, there are instances when there is refractory bleeding despite appropriate blood product administration, necessitating the use of other drugs that can reduce bleeding. In specific patient populations such as those with right-sided heart failure, rapid transfusion of blood products may not be tolerated. Some patients may refuse blood transfusions for religious (Jehovah’s witness) or personal reasons. In specific situations such as on the battlefield or in a pandemic, blood donation and banking may limit the supply and availability of blood products.
Blood transfusion is associated with infectious and noninfectious complications, which have resulted in an increased emphasis over the years on hemovigilance strategies and implementation of best practices guidelines. Transfusion-related adverse events include transfusion-related lung injury (TRALI), transfusion-associated circulatory overload (TACO), transfusion-associated hypothermia, allergic reactions, and acute hemolytic transfusion reaction. With advances in donor screening, transmission of viruses, such as human immunodeficiency virus (HIV), hepatitis B, and hepatitis C, has been reduced considerably; however, it has not yet been eliminated. Transmission of prion-based diseases is possible but rare. Bacterial contamination of platelets, which must be stored at room temperature, is always a concern ( Table 57.1 ). Immunomodulation is another important risk of transfusion, which may be mitigated, in part, by leukoreduction of red blood cells.
| Infectious | Noninfectious | ||
|---|---|---|---|
| Human immunodeficiency virus | Hemolytic | ||
| Hepatitis B virus | Transfusion-related acute lung injury | ||
| Hepatitis C virus | Transfusion-associated circulatory overload | ||
| Human T-cell lymphotropic virus | Allergic reactions | ||
| West Nile virus | Febrile reactions | ||
| Cytomegalovirus | Graft-versus-host disease | ||
| Creutzfeldt-Jakob disease | Iron overload | ||
| Bacterial (platelets) | Immunomodulation |
Since the introduction of patient blood management strategies in the perioperative setting, there has been an increased emphasis on minimizing transfusion by employing the following strategies: (1) Managing preoperative anemia by treating with erythropoietin, iron, and vitamins; (2) minimizing blood loss by improving surgical hemostasis and the use of topical hemostatic agents, autologous blood salvage techniques, and antifibrinolytics such as tranexamic acid; and (3) optimizing allogenic transfusions to improve patient outcomes.
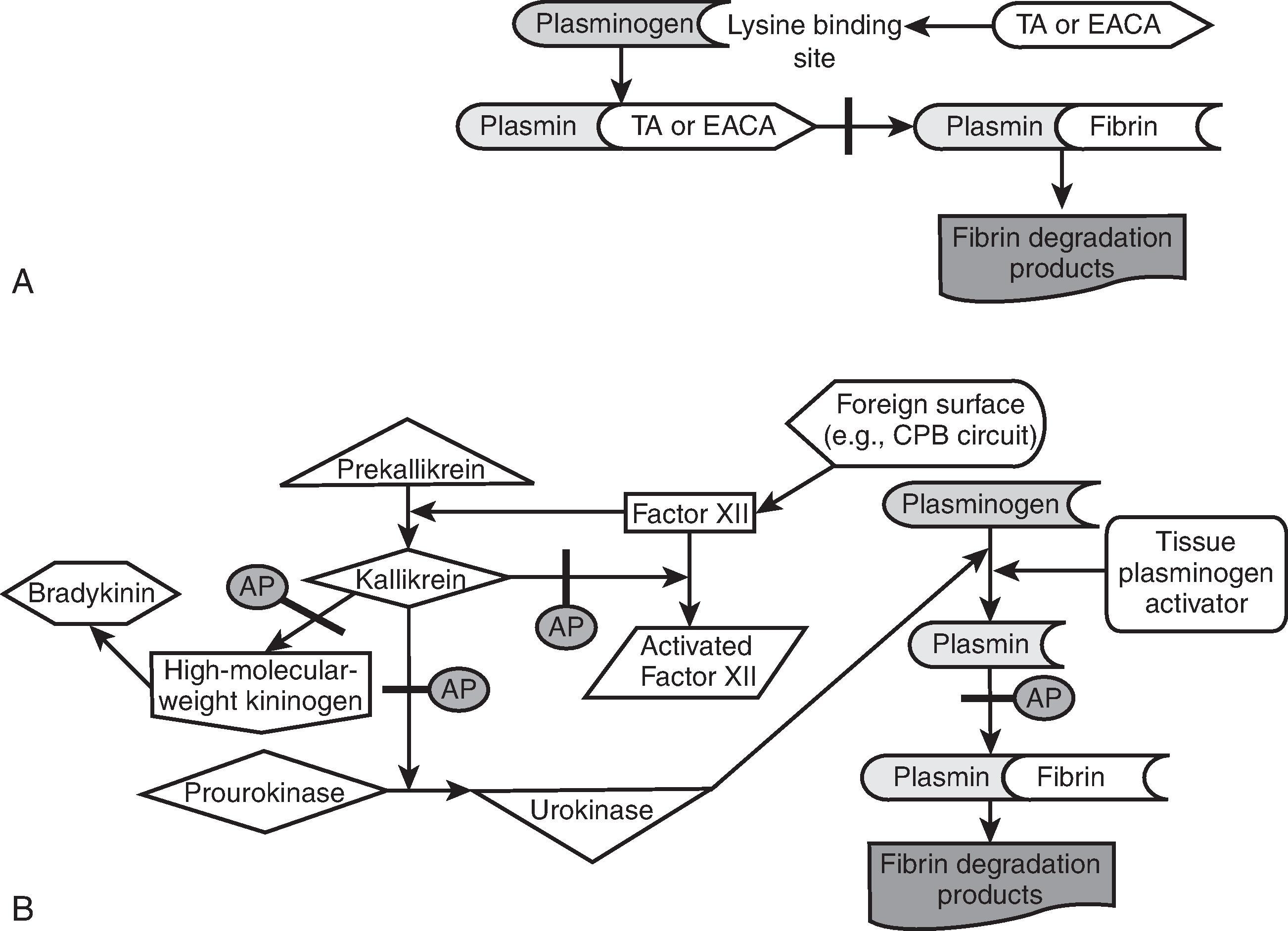
Antifibrinolytic drugs have been used extensively in cardiac surgery, trauma surgery, and orthopedic surgery. The two main drugs in clinical use in the United States are tranexamic acid (TXA) and ε-aminocaproic acid (EACA). They are both synthetic lysine analogs that bind reversibly to the lysine-binding site of plasminogen, which, in turn, displaces plasminogen from fibrin and prevents fibrinolysis. Both drugs are excreted renally and require dose adjustment for patients with renal insufficiency. TXA has more sustained tissue antifibrinolytic activity and is 7 to 10 times as potent as EACA.
Aprotinin is a nonspecific serine protease inhibitor derived from bovine lung. It acts at several proteases, including plasmin, kallikrein, trypsin, and factor XII ( Fig. 57.1 ). Compared with the lysine analogs, aprotinin not only inhibits fibrinolysis but also complements activation and contact activation of both coagulation and inflammation. In addition, aprotinin also preserves platelet function after cardiopulmonary bypass. There is a small risk for anaphylaxis, especially with repeated exposure. It should be noted that aprotinin artificially prolongs celite-based activated clotting time (ACT) measurements; therefore a kaolin ACT test should be used. Dosing is based on kallikrein-inhibiting units (KIU). Aprotinin was withdrawn from the US market in 2008 after Blood Conservation Using Antifibrinolytics in a Randomized Trial (BART) showed an increase in the mortality rate compared with the lysine analogs (see Fig. 57.1 ).
Desmopressin (1-deamino-8-D-arginine vasopressin, DDAVP) is a synthetic analog of the hormone arginine vasopressin, also known as antidiuretic hormone (ADH). It is Food and Drug Administration (FDA) approved for the treatment of hemophilia A (when factor VIII activity is greater than 5%), von Willebrand disease type 1, and diabetes insipidus. It has also been used off-label to treat other forms of platelet dysfunction (e.g., uremia-induced or post cardiopulmonary bypass) because of its ability to release endogenous stores of factor VIII, von Willebrand factor (vWF), and plasminogen activator, which, in turn, enhance platelet function. The recommended dose is 0.3 mcg/kg and effects are seen within 30 minutes of intravenous (IV) administration. Contraindications include moderate to severe renal insufficiency and hyponatremia. In the perioperative setting, transient hypotension caused by decreased systemic vascular resistance is the most common side effect, although this is mitigated by slow infusion. ,
Protamine is a strongly basic polypeptide used in the reversal of unfractionated heparin. It binds to the highly acidic heparin molecules to form a stable salt that lacks anticoagulant properties. Protamine by itself, however, is a weak anticoagulant, with effects on factor V, platelets, and fibrinolysis. Inadequate or excess doses can result in bleeding. It is not effective for reversal of low-molecular-weight heparin. Reactions may include histamine release and anaphylactic, anaphylactoid, and pulmonary vasoconstriction. Slow administration can help prevent some of these reactions. Treatment of a protamine reaction is supportive.
Warfarin works by inhibiting the vitamin K-dependent gamma-carboxylation of factors II, VII, IX, and X, as well as proteins C and S. As such, warfarin can be reversed by the administration of vitamin K, and effects are seen in 4 to 6 hours if given intravenously. Oral administration requires up to 24 hours for full effect. , If more urgent reversal is necessary, fresh-frozen plasma (FFP) or prothrombin complex concentrates (PCCs) should be used, supplemented by vitamin K because of the short half-life of exogenous factors. The American College of Chest Physicians recommends the addition of 5 to 10 mg IV vitamin K to be given in addition to plasma transfusion for rapid reversal. Concerns over anaphylaxis have led many to avoid IV use of vitamin K, but these reactions are quite rare, and IV administration should not be avoided if urgent reversal is needed.
PCCs are the recommended means of rapidly reversing warfarin anticoagulation in the setting of life-threatening bleeding or the need for an emergent/urgent procedure. They are isolated from pooled human plasma and contain varying amounts of the vitamin K-dependent clotting factors. These clotting factor concentrates are available as the following formulations: three-factor (3F; Factors II, IX, X) and four-factor (4F; Factors II, VII, IX, X, also with Proteins C, S, and some heparin to prevent VIIa and then Xa formation). In the United States, a 4F-PCC formulation is approved by the FDA for the reversal of warfarin-associated bleeding and reversal of warfarin anticoagulation in the settings previously described (Kcentra, CSL Behring, Marburg, Germany).
Compared with FFP, the theoretical advantages of PCCs include immediate availability without thawing, small volume of administration, rapid administration, and viral inactivation. Disadvantages include the potential for thromboembolic events and cost. In addition, FFP contains more than just the specific factors found in PCCs (e.g., fibrinogen).
Recombinant activated factor VII (rFVIIa) is FDA approved for the treatment of bleeding in congenital factor VII deficiency and in hemophilia patients with inhibitors to factor VIII or IX. It has been used off-label in a variety of scenarios, including trauma, intracranial hemorrhage, surgery, and reversal of anticoagulation. , The mechanism of action is related to its ability to complex with tissue factor, allowing it to activate factors X and IX, which, in turn, complex with other factors to convert prothrombin to thrombin. It should be noted that rFVIIa is a relatively expensive drug, costing approximately $10,000 for a typical adult dose ( Table 57.2 ).
| Agent | Loading Dose | Infusion | ||
|---|---|---|---|---|
| Epsilon aminocaproic acid | 100 mg/kg (5–10 g) | 30 mg/kg (1 g/h for 4–6 hours) | ||
| Tranexamic acid | Low dose: 10 mg/kg bolus, 1–2 mg/kg CPB High dose: 30 mg/kg bolus, 2 mg/kg CPB |
Low dose: 1 mg/kg High dose: 16 mg/kg for 6 hours |
||
| Desmopressin | 0.3 µg/kg over 30 min | |||
| Protamine | 1.0–1.3 mg per 100 units circulating heparin | |||
| Vitamin K | 5–10 mg IV | |||
| Prothrombin complex concentrate | 10–15 IU/kg, repeat x1 | |||
| Recombinant factor VIIa | 9–120 µg/kg (Adult dose 1 mg) |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here