Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic visceral pain is common. Abdominal pain is among the main reasons for physician visits, with more than 12 million consultations each year in the United States. Patients with visceral pain present unique challenges as the pain is often poorly localized, associated with strong autonomic reactions and changes in visceral function. Pain management, in turn, may further alter visceral function, with opioid effects on the gastrointestinal tract providing a good example. These unintended treatment effects on visceral function can exacerbate pain or lead to additional discomfort, thus showing that rational and effective pain management needs to be based on an understanding of the anatomic and physiologic basis of visceral function and pain. Lastly, visceral pain may elicit a stronger emotional response in patients than somatic pain, which may lead to increased pain-related disability and affect the transition to chronicity.
Most viscera arise from midline structures and thus receive bilateral innervation. As a result, visceral stimuli activate both hemispheres of the brain, with a predominance of the left side in most right-handed individuals. , In addition, organs in the chest cavity and most viscera within the abdomen receive dual afferent innervation with vagal and spinal nerves conveying sensory input to the central nervous system ( Fig. 41.1 ). While vagal fibers do not reach the pelvic organs, the distal colon, bladder, prostate, and uterus also have a complex sensory innervation with afferents projecting through the thoracolumbar (hypogastric) and lumbosacral (pelvic) nerves to the spinal cord.
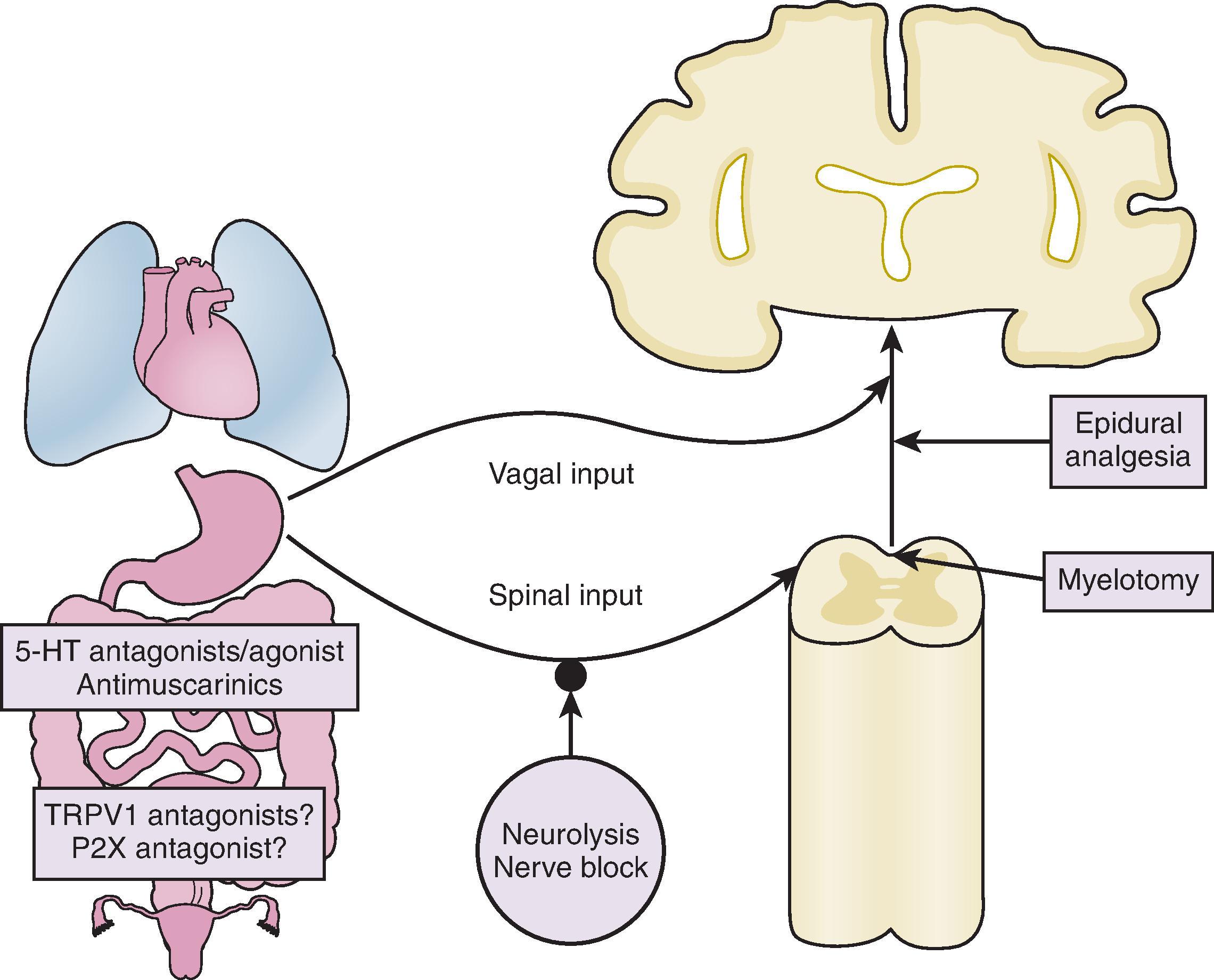
The vagus nerve predominantly comprises afferent fibers (≥80%), which project via the nodose and jugular ganglia to the nucleus of the solitary tract in the brainstem. Spinal afferents pass through the prevertebral (sympathetic) ganglia to the dorsal root ganglia and send their endings to the dorsal horn and central gray of the spinal cord. Information about noxious stimuli is relayed rostrally through the spinothalamic tract. In addition, post-synaptic dorsal horn neurons within the central gray send their central processes through the medial aspect of the dorsal columns, a pathway that has been recognized as uniquely important in visceral pain.
Most physiologic studies characterizing the properties of visceral sensory pathways rely on responses to defined mechanical stimuli. Vagal afferents form a relatively homogeneous group that is activated by low-intensity mechanical stimuli and encodes stimulus intensity over a wide range. The low activation threshold is consistent with the presumed role of these sensory pathways in regulating physiologic processes. In contrast, two classes of mechanosensitive spinal afferents can be distinguished based on their response characteristics: low threshold fibers are similarly activated by low-intensity stimuli and continue to encode stimulus intensity over a wide range, whereas high-threshold fibers are activated by intense, potentially noxious intensities of mechanical stimuli. Thus spinal high-threshold fibers resemble specialized nociceptors that have been described and characterized best in the skin, suggesting that they play a primary role in visceral nociception. , However, recent studies call such a “specificity” of nociceptive pathways into question as low-and high-threshold fibers project to similar regions in the spinal cord with more intense stimuli recruiting more afferents, a conceptual shift from specificity to intensity coding.
Most studies of visceral afferent pathways rely on mechanical stimulation to identify fibers or neurons projecting to various inner organs. Recent investigations suggest that such a biased search strategy may miss approximately 25% of the primary afferent fibers. While these afferents are referred to as “silent” based on their lack of mechanosensitivity, they likely respond to other stimulus modalities and can be recruited by exposure to inflammatory mediators or chemical signals in the bladder and gut. , Finally, most visceral sensory neurons are polymodal, meaning they respond to multiple stimulus modalities, including endogenous and exogenous chemicals contained in luminal contents, temperatures (heat or cold), and stretch.
In the airways, gastrointestinal tract, and urinary bladder, nerve fibers are found close to epithelial cells, which often exhibit specializations with secretory vesicles on the basal surface. Structural organization and functional studies suggest that visceral epithelial cells function as an interface between chemical or mechanical stimuli and the nervous system. The best example is serotonin release from enteroendocrine cells in the gastrointestinal tract. The gut is the major source of this signaling molecule and contains 95% of the serotonin in the body. Most of this serotonin is stored in specialized enteroendocrine (enterochromaffin) cells and can be released by chemical or mechanical stimuli, activating intrinsic and extrinsic neurons. Within the urinary tract, epithelial cells release adenosine triphosphate (ATP), which acts on purinergic receptors (P2X receptors) and is involved in normal micturition as well as bladder pain. Bladder epithelial cells also express the capsaicin receptor TRPV1, an ion channel that is activated by acid, temperature, endogenous lipid mediators, and the pungent substance (capsaicin) contained in hot pepper. Animals with a targeted deletion of this channel display altered micturition behavior, again lending to the importance of epithelial cells in visceral sensation. A variety of luminal contents present in the gut can interact with epithelial cells or nerve terminals through the activation of protease-activated-receptors (PAR). For example, PAR-2 receptors are present in the submucosal neurons and extrinsic afferent neurons. Luminal proteases, such as trypsin, protease-released inflammatory cells, or the resident microbiome can cleave the tethered ligand and activate this pathway, thereby contributing to sensitization.
V isceral afferents can sensitize in response to inflammation or injury. The release of mediators, such as prostaglandins or bradykinin, rapidly alters the properties of ion channels, leading to an increase in neuronal excitability. In addition, cytokines and growth factors may trigger transcriptional changes, affecting the properties of sensory neurons through alterations in gene expression. As described above, luminal contents may directly affect the functioning of afferent neurons or indirectly influence neuron excitability by activating epithelial or immune cells. Increased peripheral input ( peripheral sensitization ) may secondarily alter sensory processing in the central nervous system ( central sensitization ), with both of these sensitization states contributing to the development and maintenance of visceral pain syndromes. One easily recognized consequence of sensitization of visceral afferent pathways is increased tenderness to palpation over a larger area than what would be expected based on the underlying pathology. Both peripheral and central mechanisms contribute to the increased sensitivity and expanded areas of referred pain, which are common in irritable bowel syndrome (IBS), functional dyspepsia, and patients with painful bladder syndrome (formerly known as interstitial cystitis), or similar disorders.
Vagal afferents project to the nucleus of the solitary tract and from there via the parabrachial nucleus and ventromedial thalamus to the insular cortex. They form many connections with the hypothalamus, supraoptic nucleus, anterior cingulate cortex, and amygdala, which are essential for autonomic and emotional responses to visceral stimulation. , Spinal afferents also project to the thalamus. However, they are preferentially found in the posterolateral nucleus, which is connected to cortical areas, including the insula. The lateral components primarily serve discriminative functions associated with pain perception (e.g. location and intensity). At the same time, the medial thalamic nuclei, the main target of vagal input, are more closely linked to emotional and autonomic responses triggered by pain and other visceral inputs. Consistent with the bilateral innervation of organs originating from midline structures, most visceral stimuli activate both cerebral hemispheres, albeit with a preferential activation of one, mostly the left side. , , Studies using functional brain imaging have not demonstrated striking differences in the supraspinal processing of visceral and non-visceral pain. However, visceral pain activates the perigenual portion of the anterior cingulate cortex, whereas non-visceral pain is primarily represented in the mid-cingulate cortex. The physical proximity or even overlap between the processing of visceral pain and emotion in the perigenual portion of the anterior cingulate cortex may well explain the stronger emotional response to painful visceral than non-visceral stimuli.
Increased afferent input alters the response properties of second-and higher-order neurons, potentially leading to lasting functional and even structural changes. In addition, factors independent of specific peripheral input, such as anxiety with associated hypervigilance, affect descending modulating mechanisms, which can also facilitate synaptic transmission along afferent pathways and affect the perception and impact of pain. More recently, the potential contribution of glial cells has generated new insights into the role of non-neuronal cells in synaptic plasticity, thereby opening another potential venue for targeted pain management strategies. While experimental approaches typically focus on selecting mechanisms contributing to sensitization, clinicians face the combined impact of synaptic plasticity of afferent pathways driven by different processes, such as inflammation or cancers, compounded by central states or traits, such as anxiety or arousal with anticipation or altered sensory processing and the associated changes in descending modulation. Thus agents affecting a single step or process will have more limited efficacy in clinical practice than in more controlled experimental settings. The mechanisms of central sensitization and potential treatment strategies are not unique to visceral pain and are discussed in more detail in Chapters 8 and 9.
Visceral events that can produce a conscious sensation or acute pain in humans include traction of the mesentery, distension of hollow organs, strong contractions of muscle layers surrounding such hollow organs, ischemia, and chemical irritants. , As routine endoscopic interventions have been established, cutting or burning—two clearly noxious stimuli when applied to the skin—are not perceived when applied to the viscera, thus setting visceral apart from non-visceral sensation. Because of its sensitizing influences on sensory pathways, visceral inflammation can trigger pain and/or increase the excitability of visceral afferent pathways (e.g. enhancing low threshold input into a noxious range), which can become chronic (e.g. chronic pancreatitis). Finally, while not studied in as much detail, malignancies can trigger chronic pain because of direct effects of the tumor on afferent nerves (e.g. nerve compression, release of mediators, and growth factors) or because of indirect effects, such as distension of a hollow organ. ,
Current evidence suggests that spinal afferents primarily serve the discriminatory function of nociception, which encodes the location and intensity of visceral pain. Thus treatment strategies, such as regional block or surgical dissection generally target spinal afferent pathways.
Unilateral nerve blocks are often ineffective, which is least partly because of complex afferent innervation with sensory fibers projecting centrally on both sides in two distinct pathways.
Visceral pain is a complex experience associated with strong emotional and autonomic reactions, which correlates with the areas activated by visceral pain and emotional processing in the anterior cingulate cortex.
Impaired function of the viscera, such as decreased transit of material in the gut, may cause or contribute to pain because of the composition of luminal contents, increased distension, or the resulting contractions of visceral muscles. Thus effective pain management needs to consider analgesic therapies and treatment strategies targeting specific visceral functions.
Surgical and non-operative approaches have been developed to perform transient nerve blocks or permanently destroy the sensory pathways involved in visceral pain. Given concerns about the irreversible nature of nerve ablation or neurolysis, most studies targeting visceral sensory pathways have involved patients with inoperable cancers and relatively short life expectancies. As these patients typically present in advanced stages of their disease with poor performance status, surgical denervation plays only a minor role in the treatment. Chemical neurolysis, generally using high concentrations of alcohol or phenol, can achieve comparable results without subjecting patients to the risk of an operation. Since the first description by Kappis nearly 100 years ago, several techniques have been developed to optimize the targeted delivery of neurolytic agents and minimize the likelihood of adverse effects. These approaches utilize imaging methods to guide and confirm appropriate needle placement, such as fluoroscopy, ultrasound, or computerized tomography. However, despite this wealth of literature, few systematic studies have addressed the efficacy, outcomes, or adverse effects of these interventions. Problems assessing the effects of visceral pain management with peripheral blocks are further confounded by differences in type, concentration, and amount of the neurolytic agent, primarily alcohol, in both definition and measurement endpoints and in follow up time.
Spinal afferents innervating organs in the upper abdomen traverse the celiac plexus with two distinct ganglia located caudal to the origin of the celiac artery. The afferents travel centrally behind the crura of the diaphragm in the splanchnic nerves. The traditional dorsal approach uses the 12th rib and spinal process of the first lumbar vertebra as landmarks. , With the patient in the prone position, a needle is advanced about 7 cm lateral to the midline at a 30–45 degree angle and tilted slightly cranially to reach the lateral wall of the body of the first lumbar vertebra. The needle was then moved anteriorly by approximately 2 cm. If aspiration does not yield blood return, water-soluble contrast (3–5 mL) often mixed with a local anesthetic is injected under fluoroscopic guidance. To better directly target the celiac plexus, the needle can be placed approximately 2 cm more anterior, which requires piercing the diaphragmatic crura and positioning the needle close to the anterolateral aspect of the aorta. Severely ill patients with respiratory compromise, patients with significant ascites, or recent abdominal surgery often poorly tolerate being in the prone position for the time required to complete this procedure. Therefore an anterior approach has been developed with the advancement of the needle from the epigastric area toward the body of the first lumbar vertebra. If the appropriate position is confirmed, a neurolytic agent, generally phenol or alcohol, is given. Current approaches mostly rely on the tissue destructive properties of alcohol, which is used in concentrations between 50%–99% and volumes between 20 and 50 mL per injection. Injections are generally performed bilaterally to destroy the afferent pathways effectively. More recent reports suggest that radiofrequency ablation may provide an alternative and perhaps better approach than chemical neurolysis. , However, larger studies are needed to more conclusively show a clinically relevant difference between these approaches.
Various imaging techniques have been used to improve the efficacy of neurolysis and to decrease the potential for adverse effects. The celiac ganglia are too small to allow direct visualization with computed tomography (CT) scanning or transabdominal ultrasound. Using endoscopic ultrasonography, the scanner can be brought into close proximity to the plexus. However, the ganglia do not differ in echogenicity from surrounding structures; thus they do not allow direct imaging and identification of the target structure. Therefore all approaches rely on identifying the celiac artery as the main landmark. CT allows guidance of the needle to the target area and a three-dimensional reconstruction of the area affected by the neurolytic agent, based on the spread of radio-opaque contrast. While ultrasound allows real-time guidance without radiation exposure, air in the overlying structures often interferes with sound penetration and imaging, thus limiting its utility for patients undergoing celiac plexus block. Endoscopic ultrasound with the use of an endoscopically advanced needle has been successfully used. Close inspection may identify tumor infiltration as a negative prognostic criterion and thus help in appropriate patient selection. In addition, alcohol injection alters the echogenicity of the affected tissue, thus allowing direct visualization of the spread of the neurolytic agent. Only one trial directly compared endoscopic and conventional percutaneous approaches in celiac plexus block, suggesting the superiority of the endoscopic approach for efficacy outcomes.
One randomized controlled trial and several small case series have used surgical approaches to ablate the celiac ganglia or splanchnic nerves. Direct visualization during surgical exploration allows targeted injection of neurolytic agents into the celiac plexus if curative resection cannot be performed. Because of advances in preoperative imaging, fewer patients currently undergo exploratory laparotomies, thus limiting the number of patients who might undergo an intraoperative celiac plexus block or ablation. Thoracoscopic resection of splanchnic nerves has been reported with the advent of minimally invasive surgery. As is true for less invasive procedures, approaches have not been standardized with unilateral and bilateral resection with or without vagotomy being performed to achieve pain control in these patients.
Despite a wealth of published data, questions about the benefits, the best approach, and potential unintended consequences remain regarding the efficacy of neural blocks and ablation, which are likely because of differences in patient selection, interventional techniques, and outcome measures. A meta-analysis published in 1995 concluded that nearly 90% of patients with various malignancies experienced good pain relief for approximately three months after the procedure. Two small randomized controlled trials demonstrated similar pain control but lower adverse effects because of decreased opioid consumption in patients treated with neurolytic block. , Subsequent studies point to a slight advantage of ablative treatment over pharmacotherapy. Intraoperative celiac plexus block with 50% alcohol led to stable pain subjective pain severity scores in patients with inoperable pancreatic cancer, while patients receiving saline injection as a control experienced a significant increase in pain scores during follow up. This improvement in pain control was associated with a significantly lower use of opioids. In a posthoc analysis, patients with significant pain had improved survival if they underwent celiac plexus block, compared to controls. However, there was no overall survival benefit when the comparison was made using the original entire study cohort. Three subsequent trials comparing neurolytic celiac plexus block to analgesic therapy confirmed better pain relief after ablative therapy. In two studies, the improvement was transient with progressive recurrence of pain after about one to two months. , Most patients still required opioids, albeit at lower dosages compared to the control in the two smaller studies. , A more recent study by Wong et al. did not confirm this decrease in opioid consumption. Consistent with prior studies, their results also demonstrated that appropriate dosing of opioids achieves good pain control and quality of life that did not differ between treatment groups. However, none of these investigations demonstrated a significant effect of neurolytic plexus block on patient survival. This lack of survival difference was called into question by a large study that pointed to a possible detrimental effect of celiac plexus block in pancreatic cancer patients. The retrospective design did not allow a clear answer as to why the intervention was associated with shortened survival. However, baseline characteristics suggest a selection bias with a more advanced illness stage in the group undergoing neurolysis as a potential explanation. As cancer progression may affect the efficacy of ablative procedures by lowering apparent response rates, one small study randomly enrolled patients to perform early and late neurolytic blocks. While both groups reported better pain control than medically treated controls, there were no significant differences between the groups, arguing against disease progression as a relevant confounder. Despite some remaining questions, these data and meta-analyses indicate that pain relief after neurolytic block in pancreatic cancer is at least comparable to conventional analgesic therapy and may be associated with lower opioid consumption and thus fewer treatment-related side effects.
Rather than targeting the celiac plexus, one can also block or cut the splanchnic nerve, which has been compared in one trial with celiac plexus block. The reported improved pain control was not consistent across key primary endpoints and was only significant for a secondary outcome measure, which was a decrease in pain intensity from baseline. Thus confirmatory studies are needed to establish whether splanchnic nerve destruction is indeed superior to the neurolysis of the celiac plexus. Similarly, the results of surgical interventions with neurolytic or neuro-ablative therapy of the splanchnic nerve remain inconclusive. While the only randomized controlled trial demonstrated good pain relief and a decrease in opioid consumption, a case series evaluating different palliative operations for pancreatic cancer did not confirm a decrease in opioid use after surgery plus celiac plexus block. Smaller case series reported improved pain control in about 60%–80% of patients after thoracoscopic splanchnicectomy, performed unilaterally or bilaterally with or without a vagotomy. , Poor definition of endpoints, limited assessment of analgesic effects, the lack of appropriate control groups, and the fact that comparable results were obtained using a variety of different approaches demonstrate the need for further research with rigorous methodologic design. Splanchnicectomy reduces opioid requirements compared to systemic pharmacotherapy but not compared to celiac plexus block. , Overall, the current data suggest acceptable pain relief with an at least transient decrease in opioid requirements, but do not support the superiority of one ablative approach over another. Thus the discussion of available treatment choices for patients and physicians should primarily focus on the risk/benefit ratio of the procedure, the available expertise, and whether a specific institution or provider favors one technique over others because of appropriate training and expertise in specific techniques.
Pain relief after a neurolytic block is often transient, thus decreasing the enthusiasm to use such approaches in patients with non-cancer chronic visceral pain disorders and longer life expectancies. Given this, less information is available regarding the efficacy of nerve blocks in these patient cohorts. Several case series have been published investigating the efficacy of nerve blocks in more than 500 patients with chronic pancreatitis, making this the largest patient group with benign visceral pain disease. The initial response rates to this intervention in this population varied between 30% and 90%, with limited follow up in most cases. , , , , Because of concerns about the use of neurolytic agents, the largest series combined bupivacaine with triamcinolone. While about half of the patients reported an initial benefit, sustained analgesic responses after 24 weeks were seen in only 10% of cases. The commonly practiced addition of corticosteroids has been addressed in a randomized controlled trial, which showed no additional benefit of triamcinolone with response rates of approximately 15% one month after celiac plexus block with bupivacaine plus placebo or the steroid. Moore et al. reported results of stellate ganglion and paravertebral blocks with bupivacaine in 59 patients with refractory angina because of coronary artery disease. About 60% of the patients reported pain relief for more than two weeks. However, the benefit was transient, and most patients required multiple interventions to maintain some benefits. Interestingly, limited experience with differential neuraxial blocks suggests that primarily visceral pain was present only in about one-fifth of patients with chronic pancreatitis, with the majority experiencing “central pain,” defined by persistent pain despite surgical anesthesia through epidural administration of lidocaine. Overall, the data highlight the complex etiology of chronic pain syndromes in patients with benign visceral pain disorders and do not support the use of ablative therapies in these patients.
Several surgical and non-operative approaches target ganglia or nerve structures projecting to the pelvic structures. The most extensive experience with appropriately designed clinical trials addresses the management of dysmenorrhea and pelvic pain in endometriosis, largely relying on presacral neurectomy or laparoscopic uterosacral nerve ablation (LUNA). Three randomized controlled trials did not show a true benefit when the nerve ablation was added to the surgical treatment of endometriosis. Less is known about the impact of presacral neurectomy, which reportedly leads to lasting pain relief in more than 50% of patients described in a large case series. , Two randomized trials showed inconsistent results with one group reporting complete resolution of pain in 85% vs. 57% of women treated with and without neurectomy, respectively, while an earlier trial concluded that only menstrual pain, but not other forms of the more chronic pelvic pain, improved after surgical nerve ablation. A meta-analysis of published data did not find sufficient evidence supporting the benefit of ablative therapies in dysmenorrhea or chronic pelvic pain.
Various non-operative approaches have been developed to block or ablate afferent pathways that contribute to pelvic pain. As described earlier, the pelvic viscera conveys sensory input through two distinct spinal afferent pathways, which project to the thoracolumbar and lumbosacral segments of the spinal cord. The thoracolumbar afferents give rise to the splanchnic and hypogastric nerves, while the lumbosacral afferents form the pelvic nerve. Several distinct ganglionic structures form and are potential targets for interventions. They include the inferior mesenteric and major pelvic ganglion, as well as the presacral ganglion impar. In addition, the pudendal nerve functions as the primary sensorimotor nerve for the pelvic floor muscles, sphincters, perineum, and genitals. As is true for interventions targeting the celiac plexus, options include interventions guided by cross-sectional imaging, mostly with CT, and fluoroscopic guidance relying on bony structures as landmarks. The indication and performance of the aforementioned nerve blocks depend on the affected nerves, location of the pain, technical expertise, and availability of the equipment. Current data do not show effects on success rates.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here