Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The optimal aesthetic reconstruction using a local cutaneous flap is dependent on the size of the cutaneous defect and the orientation of the flap in relationship to relaxed skin tension lines (RSTLs). The effects on surrounding facial structures from primary and secondary tissue movement also influence the final outcome. Primary tissue movement is the movement of a cutaneous flap necessary to close a defect. Secondary tissue movement is the movement of skin and facial structures adjacent to a defect during the process of wound repair using a local flap. Large cutaneous defects of the face are often difficult to completely close with local flaps without significant distortion of surrounding anatomy caused by secondary tissue movement. When reconstructing large facial skin defects, facial structures that are frequently distorted from secondary tissue movement include the eyelid, eyebrow, nostril margin, anterior hairline, and vermilion border. Of particular concern is ectropion of the lower eyelid in elderly patients with significant laxity of the canthal tendons. Retraction or ectropion of the lower eyelid is common among these patients when skin defects in the vicinity of the lower eyelid are repaired with local flaps. To prevent distortions associated with primary and secondary tissue movements after the transfer of local flaps, full-thickness skin grafts can be used in conjunction with the flaps to minimize distortion of facial structures and achieve optimal reconstruction.
Cutaneous defects of the medial cheek frequently extend to the nose, crossing the aesthetic borders of the alar facial or nasal facial (cheek-nasal sidewall junction) sulcus. For defects involving more than one aesthetic facial region, reconstruction with a single cutaneous flap may result in blunting or obliteration of the boundary lines that topographically separate the regions. This may lead to a suboptimal outcome. This is especially true of concave boundary lines between the nose, cheek, and lip. The concomitant use of a full-thickness skin graft and a local flap to repair these types of defects will separate the reconstruction into two distinct regions of healing and may prevent blunting of aesthetic boundaries. The skin graft is usually used to resurface the nasal component of the defect and an advancement flap is used to repair the cheek component of the defect.
A full-thickness skin graft can also be combined with a local flap in other ways. For instance, a flap of subcutaneous tissue or muscle can be transferred to fill a soft tissue void. A skin graft is then placed over the flap to provide an epithelial cover for the repair. This technique is used to repair small but deep defects of the lateral alae. , Another situation where a local flap may be combined with a skin graft is for reconstruction of large facial cutaneous defects that cannot be repaired with a local flap alone or where excessive wound closure tension will occur if a local flap is used by itself. Skin grafts may also be used to cover the secondary defect resulting from transfer of a local flap. One example of this involves using a graft to repair the donor site of an intranasal bipedicled vestibular skin advancement flap or scalp flap. Using skin grafts to close secondary defects rather than allowing the wound to granulate reduces wound contraction.
There are four types of pivotal flaps: rotation, transposition, interpolated, and island. All pivotal flaps are moved toward the defect by pivoting the flap around a fixed point at the base of the pedicle. Except for island flaps skeletonized to the level of their nutrient vessels, the greater the arc of pivot, the shorter the effective length of the flap (see discussion in Chapter 6 ). Thus pivotal flaps must be carefully designed to accommodate for this reduction in length. As the flap turns in an arc around its relatively fixed pivotal point, redundant tissue, known as a standing cutaneous deformity (SCD; dog ear), develops at the base. Similar to the effective length of the flap, there is a positive correlation between the degree of pivoting of the flap and the size of the SCD that forms. The greater the pivot, the larger the deformity. Thus increasing the flap’s pivot will change the flap’s shape, shorten its effective length, and deform the flap’s base with the development of an SCD. To limit these restricting factors, a flap’s arc of pivot should not exceed 90° whenever possible. In addition to larger SCDs developing as a pivotal flap turns on its base, the larger the size of the flap, the larger in surface area is the deformity for a given pivotal arc. For large pivotal flaps, this deformity can be of sufficient size to allow its excision and use as a full-thickness skin graft to assist with the resurfacing of a portion of a cutaneous defect.
Pivotal flaps are highly versatile and can be used to repair many types of facial cutaneous defects. Although a pure pivot flap turns in an arc at its base and is not stretched, most pivotal flaps have some component of advancement. Provided the flap is the same size as the defect, it is the advancement that can cause an increase in wound closure tension and distortion of surrounding facial structures. It is in these situations that the addition of a skin graft can be quite beneficial. The combined use of pivotal flaps and full-thickness skin grafts is usually reserved for repair of very large defects in instances where the use of a skin graft is necessary to prevent excessive wound closure tension. The other instance where this combination is used is when there is insufficient skin at the flap donor site to close the secondary defect.
A 52-year-old man presented for excision of atypical junctional melanocytic hyperplasia of the cheek and lower eyelid. This skin abnormality is considered to be at high risk for transitioning to an invasive melanoma. Margins free of disease around the lesion were obtained using the “square” technique (see discussion of the square technique in Chapter 8 , Case 3). This resulted in an area requiring resection that measured 4 × 4 cm ( Fig. 16.1 ). The patient’s facial skin was taut and the area of skin excision large relative to the total surface area of the cheek. A rhombic flap was designed for repair of the cheek defect after resection of the lesion. Although the rhombic flap was designed correctly, when the flap was transposed to the recipient site after excision of the skin lesion, excessive wound closure tension was noted. The tension caused a downward pull on the lower eyelid skin causing concerns for retraction or even ectropion of the eyelid. For this reason, a full-thickness skin graft was used to assist with repair. The graft was harvested from the SCD resulting from pivoting the flap. The skin graft was positioned between the distal border of the flap and the lower eyelid. This completely relieved wound closure tension and the wound healed without distorting the eyelid. The proximity of the donor and recipient site of the skin graft ensured the best possible skin color and textural match with adjacent facial skin.

A patient with the same disease as the patient described in Case 1 is shown in Fig. 16.2 . It was necessary to resect a large area of cheek skin in addition to skin of the lower eyelid. In this case a superiorly based transposition flap was selected for repair to facilitate recruitment of skin for construction of the flap from the jowl area. The jowl region has the greatest skin redundancy of the face. The defect was too large to completely cover with a transposition flap without causing excessive wound closure tension. In this case such tension was likely to cause lower eyelid retraction or ectropion. To prevent distortion of the lower eyelid, a full-thickness skin graft was used to cover the eyelid component of the defect after resection of the skin lesion. The skin from the SCD resulting from transferring the flap (vertical lines of flap marked in Fig. 16.2, A ) was excised and used as the source for the skin graft. The skin graft served the purpose of reducing overall wound closure tension. It also enabled the use of separate and different skin to reconstruct a defect involving two aesthetic regions of the face, the cheek and eyelid. This in turn facilitated a more distinct topographic separation of the eyelid from the cheek. The skin of the SCD was not hair bearing. This skin was also thinner than the skin of the lower face. Both of these qualities made the SCD of the transposition flap the ideal donor site for the full-thickness skin graft. In this case the skin graft did not survive completely. As a result the patient developed a minor ectropion of the lower eyelid. The possible partial or complete failure of the skin graft is one of the disadvantages of combining skin grafts with local flaps to repair facial defects. The other major disadvantage of the combined approach is the possible discrepancy of skin color and texture between flap and graft. This is uncommon, however, when the source of the graft is from the SCD formed by the local flap. When skin grafts are harvested from a more distant site, skin color and texture discrepancies are more likely to be observed.

The note flap is a transposition flap originally described by Walike and Larrabee , that allows the closure of a circular defect with a triangular-shaped flap. The design of this flap consists of drawing a line tangent to a border of a circular cutaneous defect and parallel to RSTLs for a distance of 1.5 times the defect diameter. A second line the same length as the diameter of the defect is drawn at 50° to 60° to the first line to create a triangular-shaped flap. The final flap design combined with the defect resembles a musical eighth note when drawn. The surface area of the flap is typically 75% of the surface area of the defect. Although ideally the flap is used to repair skin defects less than 2 cm, larger defects can be closed using this design. The major disadvantage with larger note flaps, as with large transposition flaps, is that the SCD is also larger and requires removal. In addition, the major tension vector is perpendicular to the tangential border of the triangular flap, and it is this force that is magnified with larger flaps (see discussion of note flaps in Chapter 8 ).
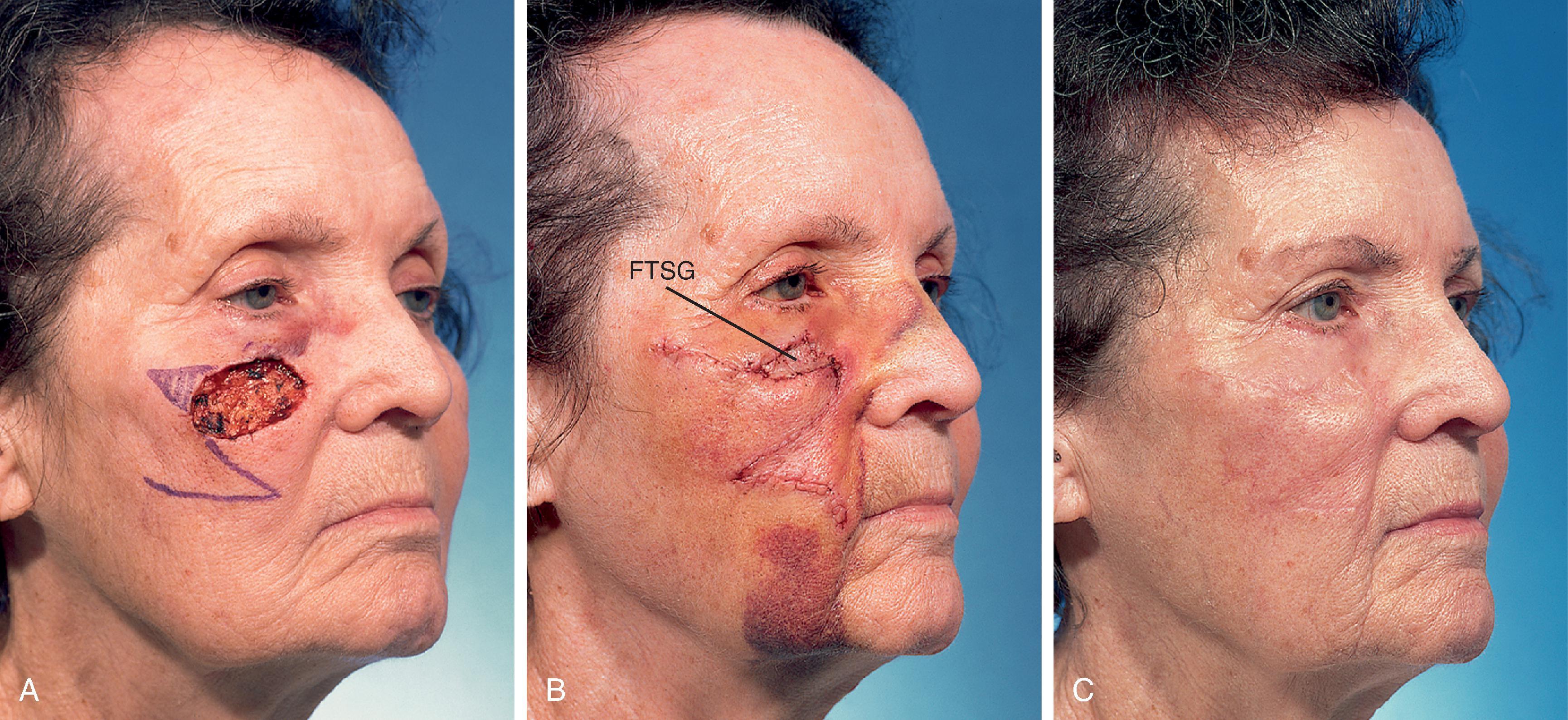
A 74-year-old woman with a basal cell carcinoma of the right cheek underwent micrographic surgical excision. The resulting skin defect measured 4 cm × 2.5 cm. A 5 cm × 1.8 cm laterally based note flap was designed for repair ( Fig. 16.3 ). In retrospect, the flap was not designed large enough to close the wound without excessive wound closure tension. This was particularly problematic because of the proximity of the defect to the lower eyelid in an elderly patient with lower eyelid laxity. When the flap was transposed, tension caused the lower eyelid to retract from secondary tissue movement. Thus, in addition to the flap, it was elected to use a 2.5 cm × 1.0 cm full-thickness skin graft, which was placed between the flap and the inferior border of the eyelid. The skin graft was obtained from the SCD marked in Fig. 16.3A . Fig. 16.3B shows the patient 5 days after reconstruction and immediately after the removal of a skin graft bolster dressing and sutures. The skin graft healed completely and perfectly matched the skin color and texture of the flap and adjacent facial skin. Most important, however, was the maintenance of a normal lower eyelid position and contour. This case represents an example of selecting an inappropriate local flap to repair a cutaneous defect. It was fortunate that a major complication (ectropion or eyelid retraction) was avoided. Avoiding the likely complication of eyelid retraction was made possible by using a full-thickness skin graft to assist the local flap in reconstruction of the defect.
Rotation flaps are pivotal flaps with a curvilinear configuration. They are designed immediately adjacent to the defect and are best used to close triangular defects. In such instances, the triangular-shaped defect is covered by a portion of the SCD, thus facilitating the pivotal movement of the flap and lessening the need to excise the deformity. The greatest wound closure tension of rotation flaps is at the advancing border of the flap. A back cut at the base of the flap shifts the position of the pivotal point, and thus changes the wound closure tension vector as well as the location of the SCD. There are several advantages of rotation flaps. The flap has only two sides; thus it lends itself to placing one side in a border between aesthetic regions of the face. The flap is broad based, and therefore its vascularity tends to be reliable. There is great flexibility in the design and positioning of the flap. When possible, the flap should be designed so that it is inferiorly based, which promotes lymphatic drainage and minimizes flap edema. Rotation flaps are discussed in detail in Chapter 7 .
The patient shown in Fig. 16.4 developed a melanoma in situ of the right cheek. Tumor-free margins were obtained around the skin lesion using the square technique. The resulting area requiring excision measured 5 cm × 3.5 cm. A 7 cm × 3.5 cm V-to-Y subcutaneous tissue pedicled advancement flap was designed to reconstruct the cheek after resection of the skin lesion ( Fig. 16.4, A ). The advancement flap proved to be of insufficient size for covering the defect because of the limited superior mobility of the flap. A 3 cm × 2.5 cm full-thickness skin graft was obtained from the supraclavicular fossa and used to cover the most superior portion of the defect ( Fig. 16.4, C ). Fig. 16.4D shows the results of the reconstruction 6 months postoperative. The skin graft was moderately unsightly and there was a depressed scar along the lateral border of the transferred flap. For these reasons, a second operation was performed in which incisions were made along the superior and lateral borders of the healed flap. The skin of the flap was widely undermined to develop a cutaneous pedicled advancement flap. The mobilized skin was advanced superomedially. Advancement was such that most of the full-thickness skin graft was removed and the resulting skin defect was covered with the advancement flap ( Fig. 16.4, E ). Figs. 16.4F–I show the patient before resection of her melanoma and 7 months after the second stage surgical procedure.

Similar to the last case, this case represents an example of poor clinical judgment in designing a local flap. The defect was large, the facial skin was taut, and the flap did not provide sufficient skin to reach the most superior aspect of the defect. A better method for reconstructing the patient would have been to use a large cervical facial rotation advancement flap. Such a flap may have prevented the need for using a full-thickness skin graft. Nevertheless, when repairing very large cutaneous cheek defects with a cervical facial rotation advancement flap, it is not uncommon that the flap must be combined with a skin graft to achieve wound closure.
This case demonstrates the advantage of staging reconstruction of large facial cutaneous defects. Using two surgical stages enabled the covering of the cheek defect resulting from resection of the skin lesion with adjacent cheek skin, which provided the best possible skin color and texture match with the resected skin.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here