Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An atrial septal defect (ASD) is a defect in the atrial septum that allows communication between the right atrium (RA) and left atrium (LA). Isolated ASDs account for 6% to 10% of all congenital heart disease.
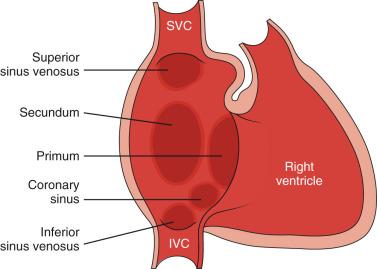
Two primary types of ASDs occur and are classified by their relationship to the fossa ovalis ( Fig. 72.1 ). Secundum-type defects (80%–90% of all ASDs) occur in the region of the fossa ovalis. Although a patent foramen ovale is similar in location, it usually is not considered a true defect as it is a persistence of the normal interatrial communication from fetal life and is present in 27% to 34% of the general population ( Fig. 72.2 ). Ostium primum defects occur anterior to the fossa ovalis at the base of the atrial septum, are usually larger defects, and are almost always associated with other structural heart defects. Additionally, two defects—sinus venosus defects and unroofed coronary sinus—do not involve the atrial septum but are physiologically equivalent to an ASD as they allow blood to shunt from the LA to RA. Sinus venosus defects are typically located posterior and superior to the fossa ovalis but may sometimes be posterior and inferior. These occur as a result of abnormal resorption of the right horn of the sinus venosus during embryologic development leading to a defect in the wall that separates the right pulmonary veins from the superior vena cava and the RA, typically resulting in anomalous drainage of the right upper, middle, or lower pulmonary veins to either the RA or superior vena cava (see Chapter 71 ). An unroofed coronary sinus is rare and occurs as a result of a partial or complete absence of the wall between the inferior LA and the roof of the coronary sinus. An unroofed coronary sinus generally is associated with drainage of a left superior vena cava to the coronary sinus or LA.
Small secundum ASDs may close spontaneously ; however, primum ASDs, sinus venosus defects, and coronary sinus defects generally do not decrease in size. Shunt volume is related to the size of the defect, right and left heart compliance, and pulmonary vascular resistance. Larger shunt volumes lead to right atrial, right ventricular, and pulmonary artery enlargement. Over time, pulmonary hypertension may develop.
Most infants and young children with ASDs are asymptomatic. ASDs usually are detected at about 6 months of age, often during evaluation for a murmur or as an incidental finding on a chest radiograph. Older children with moderate to large ASDs may have symptoms of fatigue and dyspnea. In addition to pulmonary hypertension, older children and adults with ASDs may have atrial tachyarrhythmias or paradoxical strokes, a risk that increases with age.
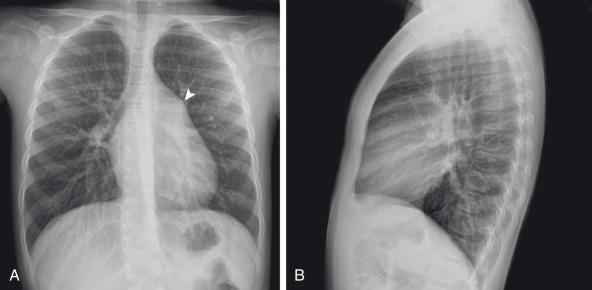
Chest radiography in the neonate usually shows that the heart is normal in size and pulmonary flow is normal. Findings in infancy and childhood include mild cardiomegaly related to right atrial and ventricular enlargement ( Fig. 72.3 ). The LA is not enlarged, which distinguishes an ASD from other left-to-right shunt lesions. Usually main pulmonary artery enlargement and increased pulmonary vascularity is found if the pulmonary to systemic flow ratio is greater than two to one. If the patient has significant pulmonary hypertension, enlarged central pulmonary arteries and peripheral pulmonary arterial vessel tapering may be seen ( e-Fig. 72.4 ).

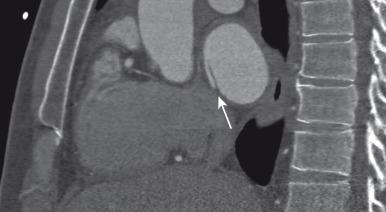
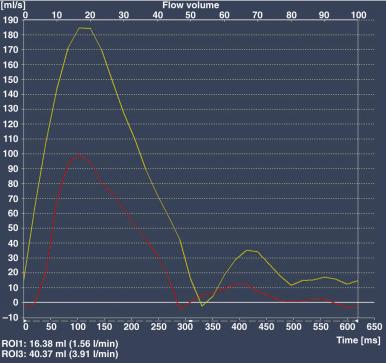
Echocardiography is the imaging modality of choice to evaluate the location, size, direction of flow across the defect, atrial and ventricular chamber size, ventricular function, right ventricular systolic pressure, and to assess for associated cardiovascular abnormalities. Magnetic resonance imaging (MRI) or computed tomography (CT) may also be used for evaluation of the atrial septum in cases of poor acoustic windows or to evaluate the pulmonary veins in patients with suspected sinus venosus defects ( to ). Left and right ventricular size and quantitative systolic function can be assessed. Right ventricular volume overload is detected as diastolic septal flattening or diastolic bowing of the septum from right to left with severe volume overload. Comparison of right and left ventricular stroke volumes can be used to calculate the ratio of pulmonary to systemic arterial flow (Qp:Qs). Right ventricular pressure is assessed by evaluating the degree of tricuspid regurgitation and septal systolic position. Systolic septal flattening is indicative of elevated right ventricular pressure. Phase contrast MRI can be used to estimate the size of the ASD and to determine the direction and amount of atrial shunting by calculation of Qp:Qs ( e-Fig. 72.5 ).
Closure should be performed in childhood to avoid complications of arrhythmia, right ventricular dysfunction, pulmonary hypertension, and paradoxical embolus. ASD closure can be performed surgically or via transcatheter closure; the latter procedure has become the primary therapy for anatomically favorable secundum defects. After closure, children with ASDs have an excellent prognosis.
Atrioventricular septal defects (AVSDs) account for 4% of all cases of congenital heart disease. Most patients with complete AVSD have Down syndrome. AVSD is also associated with visceral heterotaxy syndromes.
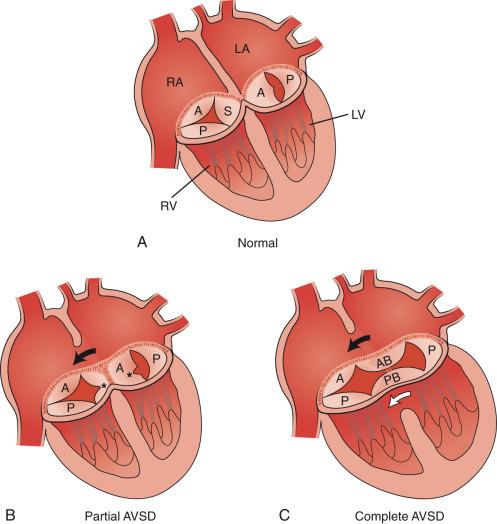
AVSD results from abnormal development of the embryologic endocardial cushions and produces a spectrum of disease ( Fig. 72.6 ). In its mild form, partial AVSD, a crescent-shaped primum ASD is found in the inferior portion of the atrial septum immediately adjacent to the atrioventricular (AV) valves, along with an associated “cleft” mitral valve with separate mitral and tricuspid valve orifices. Persons with the complete form have an ostium primum defect, an inlet ventricular septal defect (VSD) beneath the plane of the AV valves, and a single or common AV valve, with variable leaflet size, location, and morphology. Most importantly, the common valve has two components that “bridge” the ventricular septum and may form attachments to the septal surface and/or both the right and left sides of the heart. In most cases, the common AV valve is shared equally between the right and left ventricles, but the valve orifice may be unequally shared favoring either the right or left ventricle. Components of common AV valves are referred to as left- or right-sided valves rather than mitral or tricuspid as there is a single valve annulus.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here