Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
To efficiently perform an echocardiographic study on an adult with congenital heart disease (CHD), it is extremely important to understand the following: (1) the role of history and natural history, (2) location of the surgical scar(s) and probable surgical repair, (3) knowledge of segmental analysis, (4) special pediatric views and their significance, and (5) the role of transesophageal echocardiography (TEE), particularly with certain CHDs and those with poor acoustic windows.
Lack of awareness of their CHD and the anatomic diagnosis is common among adult patients for whom diagnosis and possible intervention occurred early in life. Information about procedures was provided to the parents, not to the current adult patient, whose understanding will be modified by time and the second telling. If the patient knows the diagnosis, this provides important information to the sonographer that can be beneficial while performing an echocardiogram. Patients without the particulars of diagnosis might use statements such as, “My arteries were backwards,” which might mean transposition of great arteries, or “I was born with half a heart,” which might mean a single ventricle of some sort. The statement “I had a hole in my heart” can have many meanings ranging from simple to complex problems. Patients may refer to their defect as a “heart murmur,” with no understanding of the implications.
If medical records are available, it is worth spending time reviewing this information before initiating an echocardiographic study. If records are not available, clinicians should make every attempt to procure them from the treatment facility (an important historical question), which is often known. Specific knowledge of surgical procedures is vital to understanding the patient and interpreting the echocardiogram. Subtle, but important, details such as an absent pulmonary artery or a right-sided aortic arch will make the echocardiographic examination much smoother and less time consuming.
The natural history of CHD varies tremendously depending on the defect. Not all CHD is lethal. CHD occurs in about 0.8% of live births. In the current era of significantly improved survival, , adults with complex CHDs have outnumbered children. , The total number of adults with CHD is estimated to be more than 1 million. Patients who claim to have CHD will be more likely to have a defect that is more prevalent. The actual prevalence of various forms of CHD varies depending on the study cited or methodology used for diagnosis. Bicuspid aortic valve is likely the most common “defect” but is often left out of many lists of CHD as a normal variation. Ventricular septal defect is the next most common CHD, comprising 18% to 28% of the total. A list of the rough incidence percentages of CHD is shown in Table 140.1 . , When performing an echocardiogram on an uninformed adult with CHD, knowledge of commonly found CHD and its natural history is helpful.
| Cardiac Malformation a | CHD (%) | Male-to-Female Ratio |
|---|---|---|
| Ventricular septal defect | 18–28 | 1:1 |
| Patent ductus arteriosus | 10–18 | 1:2–3 |
| Tetralogy of Fallot | 10–13 | 1:1 |
| Atrial septal defect | 7–8 | 1:2–4 |
| Pulmonary stenosis | 7–8 | 1:1 |
| Transposition of the great arteries | 4–8 | 2–4:1 |
| Coarctation of the aorta | 5–7 | 2–5:1 |
| Atrioventricular canal defect | 2–7 | 1:1 |
| Aortic stenosis | 2–5 | 4:1 |
| Truncus arteriosus | 1–2 | 1:1 |
| Tricuspid atresia | 1–2 | 1:1 |
| Total anomalous pulmonary venous connection | 1–2 | 1:1 |
Details such as the year of surgery and the total number of surgeries a patient has gone through may help to define the type of surgical repair the patient might have had. A detailed listing of timeline for various surgical procedures is provided in another chapter. Gathering all of this information may take some detective work on the part of the sonographer or cardiologist. A good example is the case of d-transposition of great arteries, which was repaired by performing an atrial switch operation (also referred to as Mustard/Senning procedure) for the first time in 1954. With advancement in surgical techniques, the approach of switching the atria was changed to performing the arterial switch operation (also referred to as Jatene procedure) for the first time in 1976. However, acceptance of this newer procedure was not immediate everywhere, implying that patients born before 1976 most likely had atrial switch operations, and those born after early 1980s very likely had arterial switch operations. It is also important to know if the patient had any form of catheter-based intervention such as a device or a stent, which were not common before the mid-1990s. Many patients may also confuse a catheter-based intervention or even a diagnostic catheterization with a “surgery.”
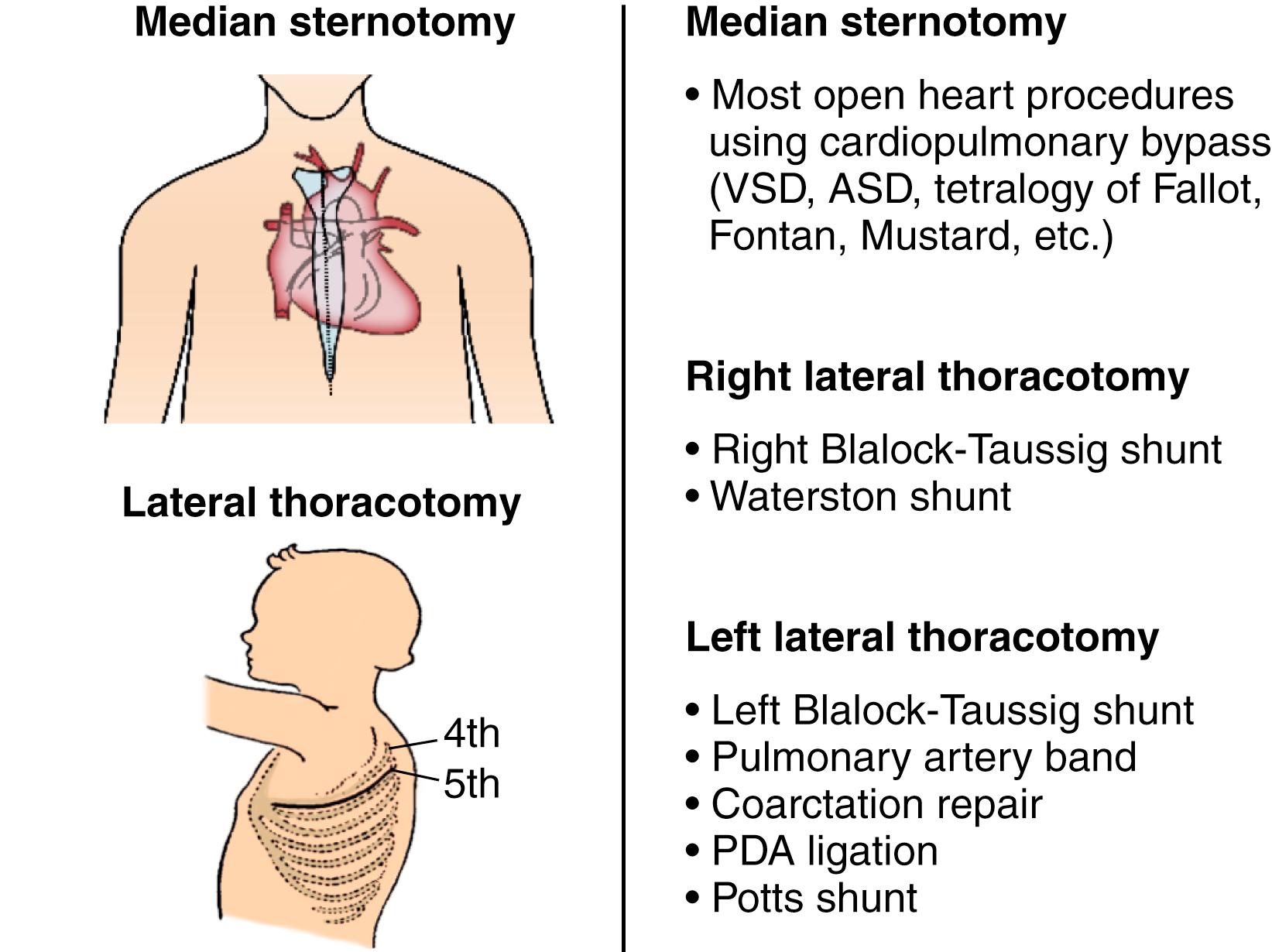
Optimal timing for repairing a particular CHD has evolved with time and advancement in surgical technique. We are now increasingly performing complete repairs for several CHDs in the neonatal period and fewer palliative operations ( Table 140.2 ). Primary open-heart repair using cardiopulmonary bypass is most frequently performed through a median sternotomy and a midline chest incision. By contrast, in earlier years, palliative operations were frequently performed using lateral or posterolateral thoracotomies. A midline sternotomy scar versus a right or left lateral thoracotomy scar can help discern the probable surgical repair and, in some cases, the possible diagnosis. Some of the operations that could be performed without opening the heart were performed via a lateral thoracotomy ( Fig. 140.1 ).
| Closed Heart Operations | Open Heart Operations |
|---|---|
| Ligation of patent ductus arteriosus | Closure of atrial septal defect |
| Repair of coarctation of the aorta | Closure of ventricular septal defect |
| Pulmonary artery banding | Repair of tetralogy of Fallot |
| Division of vascular ring or double aortic arch | Arterial or atrial switch operation (for d-TGA) |
| Blalock-Taussig shunt | Fontan procedure |
| Transventricular aortic or pulmonary valvotomy | Repair of complete atrioventricular canal defect |
a Operations done via a “closed” heart technique implies no use of cardiopulmonary bypass. “Open” heart surgery generally is done using bypass and generally through a median sternotomy.
An echocardiographic strategy, which encompasses identification of the blood flow in and out of the heart and the connection of the various segments of the heart, is called segmental analysis . This includes systematic determination of the position of the cardiac apex, situs of the atrium, the atrioventricular (AV) relationship, and the ventriculoarterial relationship. In CHD, the pathway that the blood takes and the connections between the cardiac segments are the focus, particularly in those with complex CHD. Standard American Society of Echocardiography (ASE) imaging protocols , allow the examiner to identify these points of anatomic interest and recognize the deviation from normal. It is the thinking, not just the protocol, that needs emphasis in terms of segmental analysis. Segmental thinking includes:
Cardiac position and position of the visceral organs (visceral situs)
Position of the heart in the chest and the visceral organs in the abdomen
Relative position of the atria, identified morphologically
Relative position of the ventricles, identified morphologically
Blood flow into the heart
Identification of systemic veins and its drainage
Identification of pulmonary veins and its drainage
Identification of additional venous anomalies
Blood flow through the heart
Atrioventricular connections, identified morphologically
Ventriculoarterial connections, identified morphologically
Shunts
Obstructions
Blood flow out of the heart
Aortic arch patency and branching pattern
Pulmonary artery patency, bifurcation, and size
Presence and size of the ductus arteriosus
Coronary artery anatomy
Abnormalities of cardiac position and visceral situs may be associated with complex CHDs. Imaging difficulties or confusion about complex anatomy can be made clearer after defining these points. An unusual or confusing appearance of the heart from standard left parasternal imaging planes may imply abnormal cardiac position such as dextrocardia or mesocardia.
Cardiac position and identification of visceral situs are best performed in a transverse plane from the subcostal or subxiphoid location. The transducer positioned with the notch at 3 o’clock position will demonstrate the relative position of the abdominal viscera such as liver and stomach.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here