Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This work was supported by the NIH-NINDS (R01NS049516), NCRR (M01RR000080 and UL1RR024989) and NCATS (UL1TR000439). This investigation was approved by the Institutional Review Board of MetroHealth Medical Center (IRB98-00091).
Conflict of Interest Notification
Dr. DiMarco holds two United States Patents for technology related to the content of this paper: Method and Apparatus for Electrical Activation of the Expiratory Muscles to Restore Cough (5,999,855); Bipolar Spinal Cord Stimulation to Activate the Expiratory Muscles to Restore Cough (8,751,004).
Electrical stimulation techniques have been used successfully to restore skeletal muscle function in a wide variety of motor systems. Regarding respiratory muscle function, Glenn and associates demonstrated restoration of inspiratory muscle function in patients with ventilator dependent spinal cord injury (SCI), more than four decades ago ( ; ). Via electrical stimulation of the phrenic nerves bilaterally, diaphragm pacing (DP) has been successful in liberating thousands of patients from mechanical ventilation. DP has provided these patients with more comfortable and natural breathing, elimination of the risk of disconnection from the mechanical ventilator, elimination of the stigma of being attached to a life support machine, improved speech, greater mobility, and overall improvements in life quality. Since the initial introduction of DP, refinements in technique have provided methods to implant electrodes using minimally invasive methods i.e., placing electrodes directly into the diaphragm near the phrenic nerve motor points via laparoscopic techniques ( ; ; ). This method has lessened the risk of the phrenic nerve injury, reduced length of hospital stays, and reduced overall costs while providing similar benefits to direct phrenic nerve stimulation. While restoration of inspiratory muscle function has provided significant benefits to SCI patients, perhaps even more important is the restoration of expiratory muscle function, which is necessary to generate an effective cough ( ).
In this chapter, current techniques of secretion management in patients with SCI will be reviewed, followed by the exciting development of new methods, which have the capacity to activate the expiratory muscles and restore an effective cough mechanism. The major focus of this chapter, however, will be a detailed presentation of spinal cord stimulation (SCS) to restore cough. This technique has been evaluated most extensively, and shows promise to be a useful clinical adjunct, with the potential to reduce morbidity and mortality, in subjects with SCI.
There are several modalities in current clinical practice, which are employed to manage airway secretions or to deal with foreign body aspiration. These include gravity, active suctioning with a catheter connected to a suction machine, manually assisted coughing whereby external force is applied to the abdominal wall and, use of a mechanical insufflation-exsufflation device. This latter device is used to apply a large positive pressure followed by a large negative pressure to the airway. This method has demonstrated efficacy and is frequently used in clinical practice ( ; ). While each of these techniques has demonstrated some benefit, they are also associated with significant limitations that restrict their overall effectiveness. For example, these methods are usually uncomfortable, typically labor intensive, require specialized equipment and provider-patient coordination, and lack uniform distribution of pressure within the intrathoracic cavity. Moreover, based upon the need for trained personnel alone, the annualized costs of application of these methods is also quite large. Perhaps, most importantly, despite use of these methods, the incidence of respiratory tract infections and the mortality from respiratory complications in the SCI population remains high ( ).
The act of coughing is characterized by an explosive expiration that provides a normal protective mechanism for clearing the airway of secretions and foreign material. While the development of a cough in patients with normal expiratory muscle function is generally considered a nuisance, the absence of an effective cough can result in significant discomfort to patients who find themselves unable to clear secretions, dislodge foreign bodies, and who live with the recurrent fear of aspiration when eating or drinking. Patients with upper thoracic and cervical SCI suffer from paralysis of a major portion of their expiratory muscles and therefore cannot generate an effective cough mechanism. As a result, most of these patients are not able to adequately clear airway secretions and are dependent upon caregiver support for secretion management. Perhaps more importantly, the lack of an effective cough increases their risk of atelectasis and respiratory tract infections such as bronchitis and pneumonia ( ). In fact, one of the major causes of death in the SCI population is respiratory tract infection. The potential benefits of restoration of an effective cough are enumerated in Table 113.1 .
|
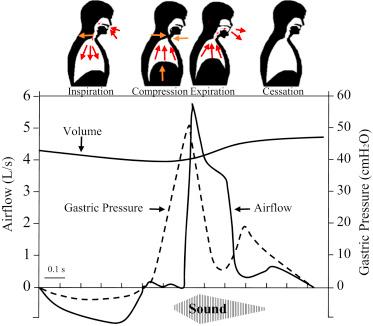
As shown in Fig. 113.1 , the normal cough reflex is comprised of several phases. The initial phase involves a variable-sized inspiration. Inspiration causes a lengthening of the expiratory muscles resulting in greater capacity to generate force. The larger the degree of inspiration, the greater potential force development by the expiratory muscles, the greater expiratory airflow and dynamic airway compression and, in turn, the greater magnitude of the cough effort. This phase is followed by glottic closure and then expiratory muscle contraction against a closed airway resulting in the development of very large intrathoracic pressures, which is represented by gastric pressure in Fig. 113.1 . In the final phase, the vocal cords and epiglottitis open widely. The large pressure differential between the airways and atmosphere coupled with the tracheal narrowing result in rapid airflow rates through the trachea and the characteristic sound associated with coughing. The resulting shearing forces cause expectoration of any foreign bodies or secretions from the airway.
Most subjects with SCI can breathe spontaneously and have normal upper airway control and glottic function. They have limited ability to cough due to minimal or absent expiratory muscle function. In theory, therefore, restoration of expiratory muscle function should provide subjects with the missing component of the cough reflex. Importantly, as with other skeletal muscles below the level of SCI, the neuromuscular apparatus is generally intact and amenable to electrical stimulation techniques to restore function.
Working under the premise that optimal generation of an effective cough is best achieved with the restoration of expiratory muscle function, several methods have been evaluated to activate the expiratory muscles. These include magnetic stimulation (MS) ( ), surface stimulation (SS) of the abdominal muscles ( ; ; ), and SCS ( ). Both MS and SS have the advantage of being noninvasive, whereas the SCS system requires surgical placement. The goal of each method is to activate the major portion of the expiratory muscles, which are typically engaged in the development of an effective cough. These include the abdominal muscle (obliques, rectus, and transversus abdominis muscles) and internal intercostal muscles of the lower rib cage.
MS involves the placement of a large coil over the back in the midline to activate the spinal roots innervating the expiratory muscles. While this technique has been shown to generate significant airway pressures in normal subjects, this could not be reproduced in tetraplegic subjects. It is likely that muscle atrophy contributed, at least in part, to low pressure development and that this would improve with muscle reconditioning ( ). However, it should also be noted that this method has significant limitations in that it is a large, bulky device requiring a 220 V power supply and therefore is not portable. Moreover, substantial heat can be generated at the stimulating coil creating the risk of thermal injury. Lastly, the presence of significant adipose tissue may interfere with successful stimulation due to the greater distance between the stimulating coil and neural activation points. It is possible with further refinement of this device, it may be a useful adjunct to secretion management in selected individuals.
SS of the abdominal muscles has been shown to produce large airway pressures with the application of electrodes with very large surface areas and large stimulation currents. McBain et al. demonstrated that SS, in patients with SCI, results in a plateau in expiratory cough flow in association with increasing expiratory pressures ( ). This finding is indicative of dynamic airway compression, characteristic of an effective cough. Despite very high stimulus intensities, which were as high as 480 mA, current density was low due to the large electrode surface area. While promising, this method has the disadvantages of tedious placement, and removal, of these large electrodes and risk of skin irritation and injury. As with MS, the presence of significant adipose tissue may interfere with its successful application in obese patients due the high electrical resistance of fat tissue. Moreover, long-term clinical efficacy of this method has yet to be demonstrated.
The SCS system results in very large airway pressure generation ( ) and peak airflow rates approximating that achieved by normal individuals. This is accomplished by applying electrical stimulation to disc electrodes, implanted on the dorsal epidural surface of the lower thoracic spinal cord. In contrast to MS and SS, this system is portable, does not require trained caregivers and is likely to be effective in virtually all SCI individuals, even those with significant adipose tissue. While this technique does require an invasive procedure, the surgical technique for placement of electrodes is a routine one that has been in clinical use for over 40 years for the management of chronic pain and spasticity. The incidence of operative complications such as infection and bleeding is also quite low. Consequently, the remainder of this chapter is devoted to this latter technique.
Prior to clinical application, extensive studies were performed in animals (dogs) to determine optimal electrode placement and evaluate the mechanism of SCS to activate the expiratory muscles ( ). These investigations demonstrated that SCS with disc electrodes placed over the T9–L1 spinal levels within the dorsal epidural surface resulted in significant activation of the expiratory muscles. Concerning the mechanism of expiratory muscle activation, SCS was shown to involve direct activation of motor roots near the electrode (∼2 segments cephalad and ∼2 segments caudal). Stimulation at the T9 level alone results in the development of large positive airway pressures due to activation of local motor roots but also more caudal motor roots via activation of spinal cord pathways ( ). However, stimulation at the T9 level does not result in complete expiratory muscle activation since stimulation with a second electrode at the L1 spinal level resulted in much greater changes in airway pressure. Use of more than two electrodes does not result in further increases in airway pressure generation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here