Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
During normal pregnancy, the maternal cardiovascular system undergoes significant hemodynamic changes to ensure an uncomplicated pregnancy and a healthy fetus. Evaluation of these changes needs precise and safe diagnostic modalities. Echocardiography is the modality of choice to evaluate cardiac structure and function in pregnant women. Transthoracic echocardiography (TTE) is noninvasive and safe; does not involve radiation; is easily available, affordable, and portable; and can provide accurate assessment of cardiac morphology and function. Transesophageal echocardiography is seldom performed during pregnancy; however, when necessary, it can be performed safely, although careful monitoring of maternal oxygen saturation is necessary if midazolam is used for sedation. However, the risk of vomiting and aspiration as well as sudden increases in intraabdominal pressure should be considered and fetal monitoring performed. Physiological exercise testing is an integral part of follow-up of patients with adult congenital heart disease and valve disease and may be combined with stress echocardiography for additional information.
Many healthy pregnant women experience shortness of breath, syncope, dizziness, and fatigue, and at later stages of pregnancy bilateral pedal edema, that mimic the presence of significant heart disease. On cardiac examination, the heart rate increases, particularly in the second trimester of pregnancy. Slight elevation of jugular venous pressure may be detected in the middle of the second trimester. Prominent first and second heart sounds may be detected that may suggest an atrial septal defect or an increase pulmonary artery pressure. Up to 3/6 ejection systolic flow murmur from increased flow through the left and right ventricular (RV) outflow tracts can be heard along with a bounding arterial pulse, a prominent apical impulse that may be shifted laterally because of the gravid uterus, and an RV impulse caused by volume overload; a third heart sound may also be present. Continuous murmurs, either a cervical venous hum best heard over the right supraclavicular area, or a mammary murmur (continuous or systolic) caused by increased flow in the mammary arteries, may also be heard over the breast late in pregnancy or during lactation period. When disproportionate or unexplained dyspnea or new cardiovascular signs or symptoms occur during pregnancy or when a new pathological murmur or diastolic murmur is heard, echocardiography is indicated.
Pregnancy has prominent effects on the cardiovascular system. These include increase in blood volume, red cell mass, heart rate, and cardiac output related to changes in afterload, preload, and peripheral vascular resistance, and these effects are sustained into the postpartum period. Pregnancy in women with cardiovascular disease is associated with impaired physiological adaptation and hence results in adverse material and fetal outcomes. Blood volume increases by 10% to 15% by 7 weeks of gestation and rises until around 32 weeks to a 30% to 50% increase in total plasma volume. About 75% of this increase has occurred by the end of the first trimester. The red cell mass also increases until the end of pregnancy to about 20%, resulting in anemia of pregnancy. Overall, cardiac output increases 30% to 50% during normal pregnancy, beginning during the first trimester and peaking at around 25 to 35 weeks of gestation.
The increase in stroke volume accounts for much of the increase in cardiac output in the first two trimesters. An elevation in heart rate becomes a more important factor in the third trimester of pregnancy. Blood pressure (BP) decreases at 7 weeks’ gestation and continues to fall until it reaches nadir by midpregnancy, reaching about 5 to 10 mm Hg (∼10%) below baseline. The decrease in the BP is related to the decrease in systemic vascular resistance (SVR), which is noted as early as 5 weeks of gestation, falling to around 35% to 40% at 20 weeks, when it plateaus. Afterward, BP gradually increases and returns to its prepregnancy level at term. , Increased level of estrogen, progesterone, and relaxin with some vasodilatory properties and increased production of vascular nitric oxide are probable contributors to reduced SVR during pregnancy. Uteroplacental shunting and decrease in vascular responsiveness to the pressor effect of angiotensin II and norepinephrine are other contributors. ,
The physiological adaptations to pregnancy influence the evaluation and interpretation of cardiac function and clinical status. Maternal cardiac dysfunction is related to impaired uteroplacental flow and suboptimal fetal outcome. , Increase in blood volume is offset by a reduction in SVR, causing no change in pulmonary artery pressures. These cardiovascular changes resolve after delivery, with hemodynamics largely returning to baseline level by 24 weeks postpartum. ,
In response to the hemodynamic changes in pregnancy, the heart undergoes major Morphologic and functional adaptations that can be detected by TTE ( Table 161.1 ).
| Echocardiographic Variable | Change During Pregnancy |
|---|---|
| LVD and volume | Increases |
| LV wall thickness and LV mass | Increases |
| LVEF | Unchanged |
| LV fractional shortening | Unchanged |
| LV radial and longitudinal strain rate | Increases |
| Aortic root diameter | Mildly increases |
| RV dimension and volume | Increases |
| RVEF | Unchanged |
| Left atrial size and volume | Increases |
| Stroke volume as measured using LVOT VTI | Increases |
| Mitral E-wave velocity | Increases and then decreases |
| Mitral A-wave velocity | Increases |
| Peak pulmonary artery systolic pressure estimated using TR jet | Unchanged |
The increase in circulating volume during pregnancy is thought to lead to an increase in left ventricular (LV) mass and a proportional increase in LV wall thickness. The ratio between ventricular end-diastolic radius and wall thickness, represented by the relative wall thickness (RWT), remains stable during normal pregnancy and is referred to as eccentric remodeling. This is in contrast to concentric remodeling, which occurs in hypertensive pregnancy when RWT increases more than LV end-diastolic radius. ,
To accommodate the increased preload, there is a 5% to 10% increase in LV end-diastolic dimension , ( Fig 161.1 ). Along with an increase in LV dimensions, there is a corresponding increase in LV wall thickness and LV mass, reaching a maximum increase of 23.6% in the third trimester followed by a sharp drop in LV mass late in the third trimester. Increase in LV mass is significantly higher in preeclamptic and pregnancies complicated by pregnancy-induced hypertension compared with normotensive pregnancies ( P < .0001).
This physiologic hypertrophy is thought to normalize the elevated level of systolic wall stress. During normotensive pregnancies, interventricular septal thickness does not change up to the early third trimester compared with reference, but thickness statistically significantly increases between 29 and 35 weeks of gestation by 0.09 cm.
Similar to the left ventricle, the right ventricle increases in size over the course of pregnancy because of the increased preload ( Fig 161.1 ). This increase in size can be detected in the apical four-chamber view at the basal or mid-RV level ( Fig. 161.2 and ![]() ).
).
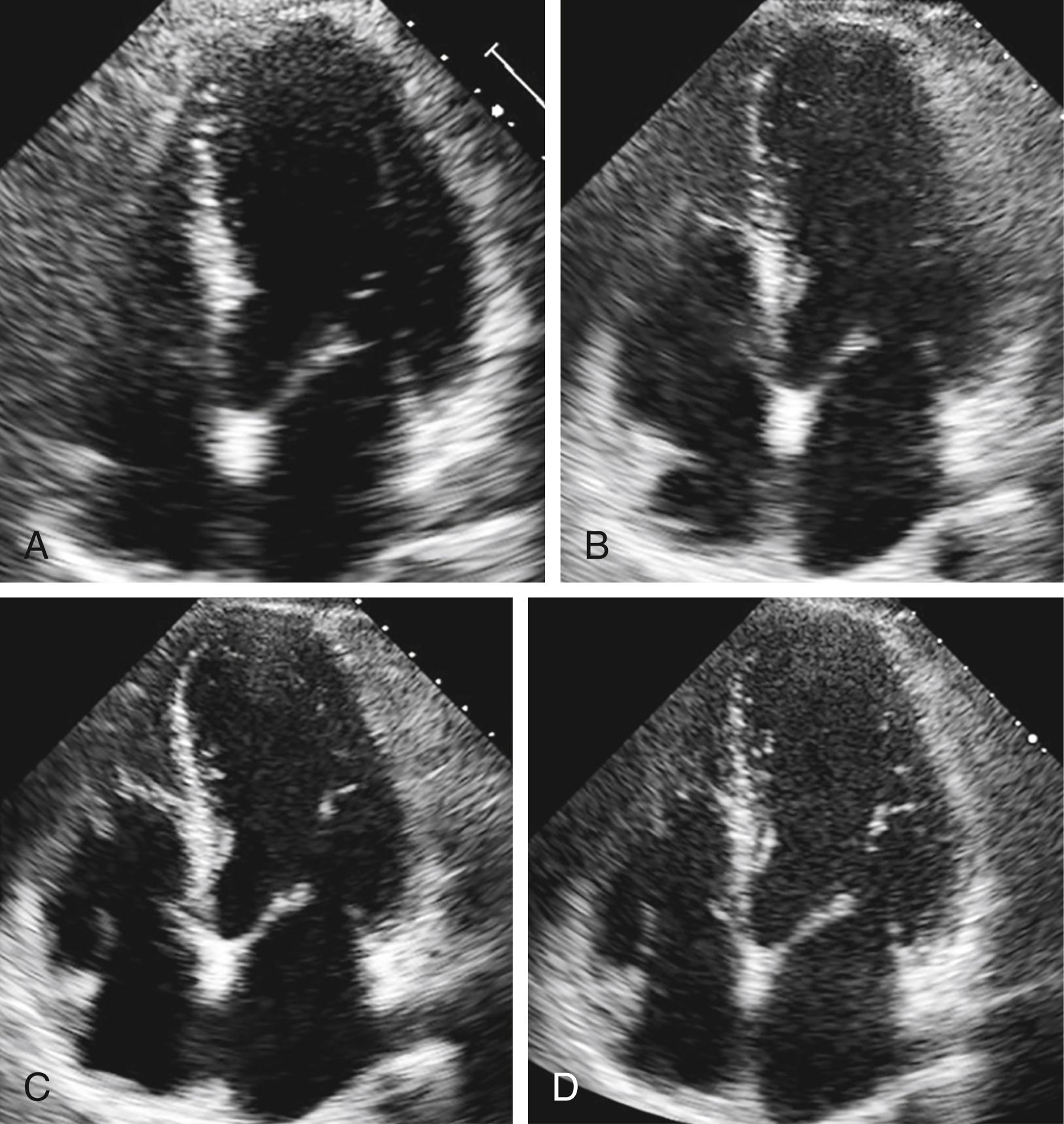
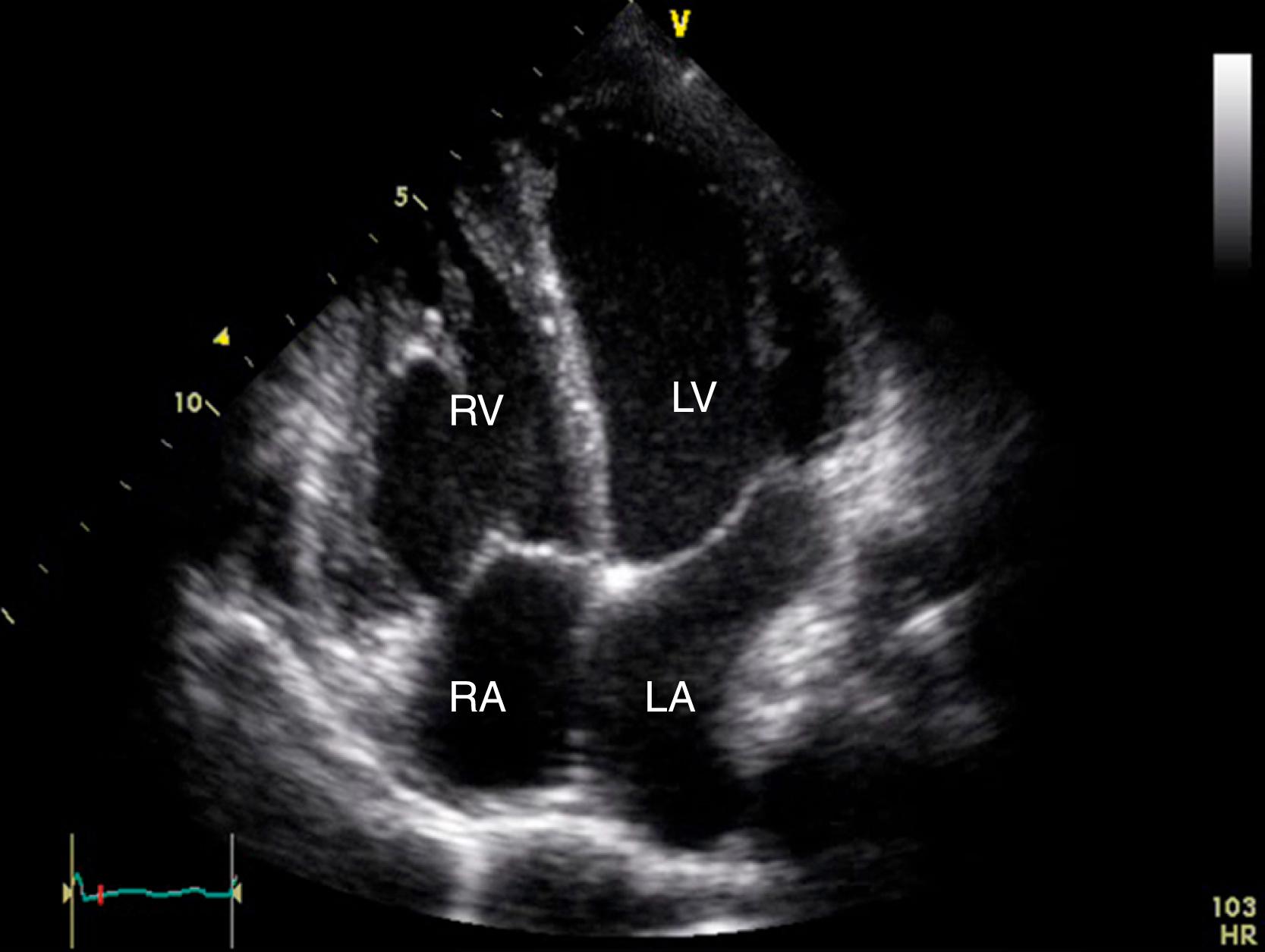
Video 161.2. Apical four-chamber view during the third trimester in a normal pregnancy shows increased cardiac chamber dimensions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here