Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The evaluation and management of cervical spine deformity remains one of the most challenging issues within spinal surgery. Although multiple etiologies exist, iatrogenic malalignment represents a significant portion of cases. This chapter focuses on the evaluation of patients with postoperative cervical deformity, reviews preventive measures, and details our surgical approach. A series of case examples demonstrates our current techniques while emphasizing surgical principles.
The importance of global spinal alignment has been increasingly recognized. In deformity surgery, the cervical spine should not be viewed in isolation, but within the greater context of the cervicothoracic junction and overall spinal balance. More recent clinical and radiographic tools have been developed to aid in quantifying the nebulous complexities and building a surgical plan.
The clinical evaluation of a patient with postoperative cervical deformity should begin by understanding the nature of the disability. The impact of the deformity on the patient's activities of daily living is a critical component and should guide both nonsurgical and surgical management. A detailed surgical history is critical to preoperative planning. Previous surgical approach, instrumentation, and decompression areas should help guide surgical planning. Patients with previous anterior surgery should be considered for evaluation of vocal cord dysfunction to determine the innervation of the recurrent laryngeal nerve (RLN). Our preference is to approach the anterior spine opposite a previous surgery, unless RLN dysfunction is identified, as bilateral RLN palsies will result in loss of phonation.
The majority of patients have kyphotic deformities, but scoliosis is also common. The malalignment may be severe, and patients report inability to maintain horizontal gaze, difficulty eating, high fatigability, and pain. With loss of stability and normal alignment, pain can be severe and results from degeneration of the intervertebral discs and facet joints, increased stress on the posterior soft tissue complexes, and an often-dysfunctional posterior muscle complex. In addition to progressive pain and deformity, postoperative malalignment is often associated with neurologic dysfunction such as myelopathy and/or radiculopathy.
The physical exam should begin with a careful neurologic assessment. Progressive malalignment is commonly associated with myelopathy and radiculopathy. Bony and ligament overgrowth in response to instability hasten central and foraminal stenosis development. Furthermore, the draping and flattening of the spinal cord over the kyphotic vertebral bodies may also contribute to myelopathy and present as hand and gait disturbance. Evaluation of the patient's global and regional alignment allows for quantification of deformity severity. Measures such as the chin-brow vertical angle assess the lack of horizontal gaze.
Standard evaluation in all spine patients should include static and dynamic radiographs of the cervical spine, including the cervicothoracic junction, as well as standing scoliosis films of the entire spine. We use the low-dose digital EOS Imaging system to obtain full-length standing films. Advanced imaging, including computed tomography (CT) and magnetic resonance imaging (MRI) of the operative region should also be obtained and allow for careful evaluation of the vertebral artery anatomy, areas of central and foraminal stenosis, the existing fusion mass, areas with previous laminectomies, and the presence of pseudarthrosis.
Radiographic measurements allow the surgeon to quantify the degree of deformity and set goals for operative correction. A variety of regional and global alignment parameters have been described and validated. On the upright lateral radiograph, the C2–C7 sagittal vertical axis is the distance the center of C2 falls from the posterior-superior aspect of the C7 vertebral body. Cervical lordosis between C2 and C7 can be measured using a variety of techniques. More recently other measurements to quantify deformity at the cervicothoracic junction and the global spine have been described but are beyond the scope of this discussion. Overall, a thorough radiographic exam is critical to optimizing a safe and effective preoperative plan.
The best treatment of postoperative cervical deformity is prevention. Iatrogenic malalignment can be produced during every step of a cervical spine operation. Errors in patient positioning, distractor placement, extent of decompression, instrumentation, selection or placement of bone graft, and even use of postoperative immobilization may all result in postoperative cervical deformity. Malalignment may occur after single-level or multiple-level operations, anterior or posterior operations, and decompression procedures with or without stabilization. The surgeon must pay meticulous attention to detail at every step of the procedure to prevent iatrogenic malalignment. This chapter reviews some of the common causes of iatrogenic malalignment of the cervical spine, outlines some techniques to avoid postoperative deformity, and discusses the treatment of postoperative cervical malalignment.
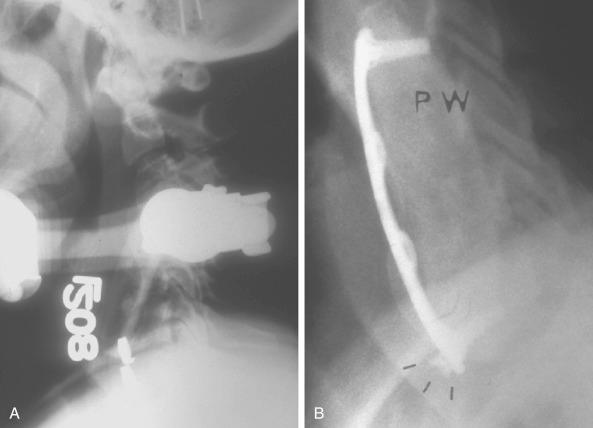
The most common error of patient positioning for anterior surgery is to put the patient's neck into hyperlordosis. A rolled towel is often placed underneath the patient across the shoulders to extend the neck. Whereas moderate cervical lordosis is desirable, hyperlordosis such that the spinous processes are touching is, in general, excessive. If the patient is fused in this position he or she will often have severe interscapular and posterior cervical pain, especially if an extensive foraminotomy is not performed at the time of the procedure. Extension of the neck narrows the posterior neural foramen and may result in root compression. To avoid this complication, we routinely inspect the position with the patient supine to ensure that the neck is in a relatively neutral or slightly lordotic position. In addition, we examine the localizing radiograph to verify that the neck is in an acceptable amount of lordosis. If the patient's neck is hyperlordotic on this radiograph, we place Caspar distractor pins with the tips converging. When the distractor is placed over the pins, the amount of lordosis will be reduced ( Fig. 105.1 ). At the end of the procedure, the goal is to have the neck in a normal lordotic configuration.
Coronal malalignment of the cervical spine may also occur. One potential cause of iatrogenic coronal deformity is taping one shoulder lower than the other during the initial patient positioning. Before prepping and draping, we routinely inspect the patient's head and shoulder positions to confirm that the cervical spine is aligned properly and that the shoulders are level. If a coronal deformity is introduced into the cervical spine at a single level, the adjacent levels will generally compensate for the malalignment with little effect on the overall balance. An instrumented fusion over multiple levels performed with the patient improperly aligned, however, may result in a postoperative deformity with clinical imbalance.
Finally, the surgeon must confirm that the patient is positioned in neutral axial rotation. Axial malalignment may occur as a result of slight rotation of the head. During the dissection and retraction, it is common for the surgeon to inadvertently push the head away from the side of the approach. Some surgeons do this routinely to assist the exposure. If the surgeon is not aware that the head is rotated toward the contralateral side and puts a plate on, the segment will be fused in rotation. The rotational malalignment is obviously compounded when multiple segments are fused with instrumentation.
The surgeon can avoid creating a rotational deformity by using one of two techniques. The first is to ask the anesthesiologist to confirm that the nose is pointed straight up before placing any grafts and beginning the instrumentation. This, however, requires that the surgeon remember to ask the anesthesiologist. We prefer to use a more foolproof technique of routinely placing a tape across the forehead to prevent inadvertent rotation of the head during the operation. Another variation on this technique is to use commercially available head holders with an elastic chinstrap to stabilize the head. When performing high cervical approaches to C2–C3 or C3–C4, it is sometimes advantageous to rotate the neck to the contralateral side to gain better access to the spine. Under those circumstances, it is a good idea to write a reminder on the sterile drape to turn the head back into neutral alignment before grafting and plating are done.
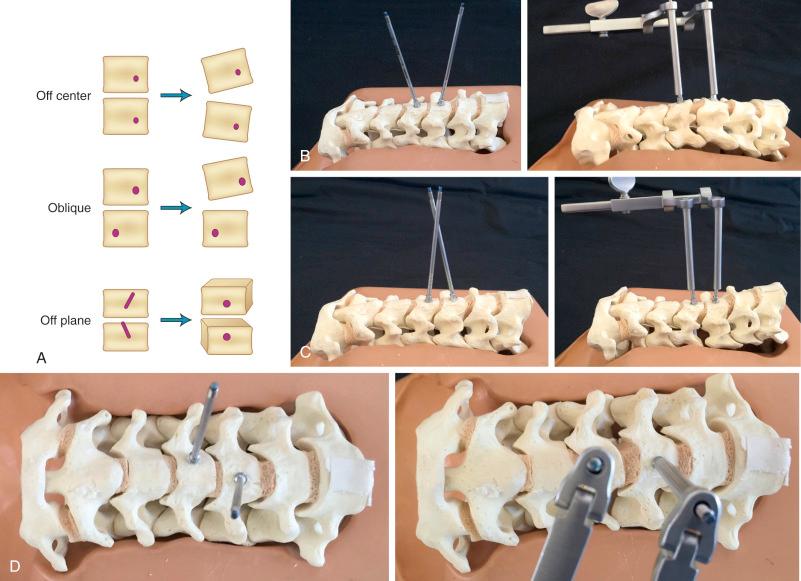
We routinely use Caspar distractor pins to open the disc space during anterior cervical surgery. Although the distractor is quite useful in exposing the disc space, the surgeon must be careful in placing the pins. If both pins are placed off center to one side, the disc space will open asymmetrically, causing segmental coronal angulation. If the pins are placed in an oblique position, the disc space will open asymmetrically and relative lateral translation of the vertebral bodies will occur. Finally, if the pins are placed in different planes, a rotational malalignment of the vertebra can occur ( Fig. 105.2 ).
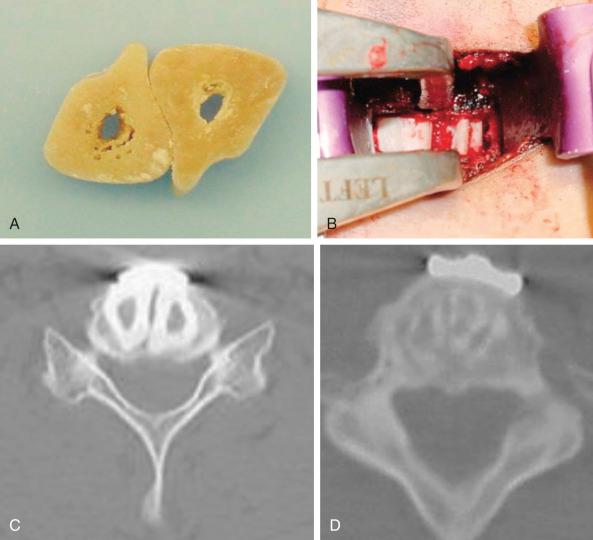
Failure to expose the entire disc space may increase the likelihood of performing an asymmetrical discectomy or corpectomy. Placing a graft asymmetrically on one side may result in a coronal plane deformity ( Fig. 105.3 ). This can be avoided by exposing the intervertebral disc to the uncovertebral joints bilaterally before starting the decompression. These lateral structures provide a fixed reference to the surgeon and assist in performing a symmetrical decompression and reconstruction.

The type of decompression performed also matters. Long corpectomies reconstructed with an allograft long bone can only be placed into a neutral or kyphotic position; because the graft is straight, it is impossible to produce lordosis. Kyphosis typically develops as the graft subsides into the endplates. To avoid this, we routinely use segmental decompression combining corpectomies at the levels that have retrovertebral compression with discectomies at levels that only have retrodiscal neural compromise ( Fig. 105.4 ). For patients who have retrovertebral compression at more than one level, we perform a procedure that we call corpectomy-corpectomy: performing corpectomy at one level and skipping the next level, followed by a corpectomy at the third level ( Fig. 105.5 ). This type of segmental decompression and fixation using several small grafts rather than one long strut graft allows for better preservation of cervical lordosis.


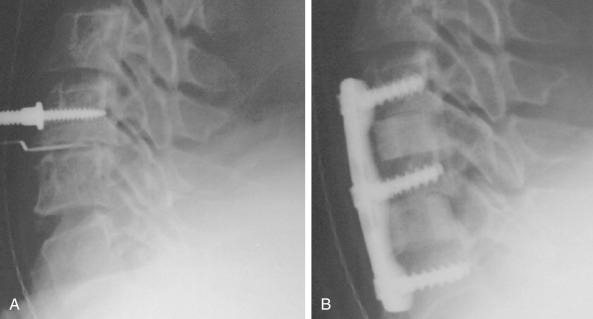
A multilevel noninstrumented arthrodesis of the cervical spine can result in kyphosis as the grafts collapse or resorb ( Fig. 105.6 ). Whereas the use of a plate does not absolutely guarantee the avoidance of kyphosis, most surgeons would agree that anterior cervical plates decrease the likelihood of postoperative kyphosis.

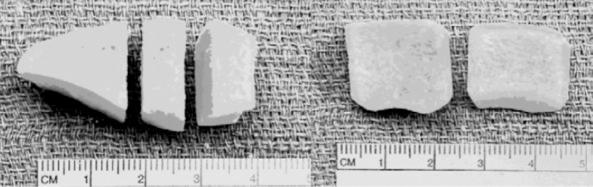
The type of graft material used can also influence the likelihood of postoperative kyphosis. In general, fresh-frozen allografts are less likely to collapse than freeze-dried bone, and freeze-dried bone is less likely to collapse than irradiated freeze-dried bone. If a surgeon finds a piece of allograft to be fragile, it is advisable to use another specimen rather than implanting an inferior allograft. We most commonly use cortical allografts harvested from the fibula, ulna, radius, humerus, and occasionally the tibia. We also use dense cancellous allograft from the patella ( Fig. 105.7 ).
The size of the graft also influences the propensity to develop postoperative kyphosis ( Fig. 105.8 ). The grafts should be large enough to allow for 1 or 2 mm of subsidence without creating kyphosis. In addition, the more graft used per level, the less likely it is to collapse. For this reason, we routinely fill the disc space with as much graft as possible, which often means placing two allografts side by side ( Fig. 105.9 ). More recently, we have moved to using iliac crest allograft. The width and depth of the disc spaces are measured preoperatively, and an allograft is hand selected and initially cut immediately before the skin incision. We prefer to fill the entire disc space, from uncinate to uncinate, with graft and we often insert a vertical “wedge” into a trough cut into the very lateral edge superior and inferior vertebral bodies. We have experienced higher union rates with this technique.

Although judicious and careful use of anterior cervical plates can help avoid postoperative kyphosis, poor attention to detail can result in plate-induced malalignment. If a screw inadvertently perforates an adjacent disc space, it can result in rapid degeneration and collapse of that disc space. Even if the screw does not perforate the next disc space, placement of a plate within 5 mm of an adjacent level increases the likelihood of adjacent-level ossification development ( Fig. 105.10 ). The adjacent-level ossification can become quite profound, causing rapid deterioration of that adjacent disc space and resulting in kyphosis. The surgeon must be careful not to use a plate that is too long, especially when using dynamic or subsidence plates, because these will migrate toward the adjacent disc spaces as the grafts subside.

When performing anterior cervical fusions on a patient with preoperative cervical scoliosis, the surgeon must pay close attention to the overall alignment of the head, neck, and torso. Often, even in a patient with severe scoliosis, the spine rebalances itself such that the patient can hold the head in a neutral position. If the surgeon corrects the cervical scoliosis in a patient with severe thoracic curve, the head will be tilted to one side. This is analogous to correcting only the thoracic curve in a patient with a balanced and oppositely directed thoracolumbar curve, thereby causing shoulder asymmetry.
Patients who have long corpectomies are prone to graft extrusion. The reported incidence is as high as 9%. Unfortunately, plates do not help prevent such complications ( Fig. 105.11 ). With static plates, extension of the neck loads the graft as the plate acts as an anterior tension band. In flexion the graft is unloaded because the anterior cervical plate acts as the center of rotation. In extension the inferior screws can pull out, and in flexion they can be driven into the next disc space, resulting in graft collapse or extrusion. To avoid these complications, we routinely perform circumferential stabilization in patients who undergo corpectomies at two or more levels. We also prefer a circumferential approach in patients with poor-quality bone who undergo single-level corpectomies.
Positioning for posterior cervical procedures is just as critical as for anterior operations. We routinely use the Jackson frame (Mizuho OSI) to position our patients for posterior operations. We tape the shoulders down as for the anterior procedures. We also make sure that one shoulder is not pulled asymmetrically to prevent an iatrogenic coronal plane deformity. We place bolsters just underneath the clavicle and use Gardner-Wells (GW) tongs with bivector traction to allow us to position the neck in either flexion or extension. We check the position preoperatively to ensure that we can place the neck into an adequate amount of flexion and extension. Foraminotomies are best accomplished with the neck in maximal flexion, which unshingles the facets and exposes the underlying superior articular facet. If the neck is not adequately flexed during a foraminotomy, a large amount of the overhanging inferior articular facet must be resected to expose the underlying superior facet. This may weaken the structure and lead to a fracture. More commonly, it makes it difficult to place a lateral mass screw in patients who require fusion and decompression. Before fusion, we change the weight from the lower, or flexion, rope to the upper, or extension, rope. The advantage of using bivector tong traction is that the surgeon can easily alter the position of the neck intraoperatively. With fixed head holders such as Mayfield tongs, an assistant has to crawl under the table to reposition the head holder.
Although it is important to position the neck properly for fixation of the subaxial spine, it becomes even more critical when one is performing an occipitocervical or an occiput-to-thoracic fusion. If the neck is improperly positioned and instrumented, the resulting malalignment can be quite debilitating. Phillips and colleagues measured the occipitocervical angle on 30 normal cervical spine radiographs of patients in flexion, extension, and neutral alignment. The occipitocervical angle was defined as the angle between the McRae line (the line connecting the basion and opisthion, which demarcates the foramen magnum on a lateral radiograph) and a line parallel to the rostral endplate of C3. The mean occipitocervical angle on the neutral radiographs was 44 degrees. Phillips and colleagues recommend that when performing an occipitocervical fixation and fusion, the surgeon should try to fix the occiput and upper cervical spine in as close to this value as possible to provide the patient with a functional head position ( Fig. 105.12 ). We concur with this for patients with occipitocervical fusions. However, when performing occiput-to-thoracic fusions, we prefer to fix the patient with 5 to 10 degrees of flexion compared with normal. This is because these patients are unable to bend their necks at all, and if they undergo fusion looking straight ahead they cannot look down to see their own bodies.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here