Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physiological changes associated with pregnancy have a profound effect on how medications are handled in pregnant women.
Most medications taken by pregnant women reach the fetus to varying degrees. The fetus is in part protected by placental efflux transporters and placental drug-metabolising enzymes. The fetus can also metabolise some drugs but to a minor degree.
Drugs reaching the fetus can be teratogenic or toxic, but the vast majority of pharmacologic agents are neither teratogenic nor toxic. Most drugs are inadequately studied in pregnancy, limiting the usefulness of the US Food and Drug Administration classification of medications.
Medication use in pregnancy is on the rise. A majority of pregnant women in the United States use at least one over-the-counter or prescription medication during pregnancy; the average number of medications taken by pregnant women in a survey in 2006 to 2008 was four. Over the past decade, women have become older and heavier at the time of conception. Consequently, the number of women entering pregnancy already receiving treatment for chronic hypertension, diabetes, asthma and other chronic conditions has also increased. Pregnant women may also receive medications for a gestation-related condition such as preeclampsia, gestational diabetes or preterm labour. Substance use disorder also leads to additional drug exposure in certain pregnant women.
Medication use in pregnancy is innately complicated because the medication may affect not only the mother but may also affect fetal organogenesis, fetal organ function and maturation. Thus fetal risk and benefit must also be considered when prescribing medications for a pregnant woman. This is particularly important during the first trimester, during fetal organogenesis. During this sensitive period, about 50% of women are exposed to at least one medication. Prescription medications commonly used in the first trimester include progestins; antibiotics; and medications for hypertension, asthma, diabetes, nausea and vomiting of pregnancy (i.e., promethazine, ondansetron) and thyroid disorders, among others. Medications taken during pregnancy after the period of organogenesis may also impact fetal organ function or maturation. Common medications include labetalol for hypertensive disorders, oral hypoglycaemic agents such as glyburide and metformin for gestational diabetes, magnesium sulphate, betamethasone and nifedipine and indomethacin for preterm labour.
Most medications used by pregnant women are used ‘off label’, meaning that the medication is Food and Drug Administration (FDA) approved but not specifically for pregnant women. In fact, very few drugs commonly used in pregnancy are FDA approved for use in this population. Pharmacokinetic and safety information is required for all drugs before FDA approval, but this information is virtually nonexistent for medications used in pregnancy. Of the 172 newly approved drugs from 2000 to 2010, there were insufficient data to assess teratogenicity in 97.7% of the drugs, and 73.3% of the newly approved drugs provided no data regarding the medication use in pregnancy. Despite this dearth of data, pregnant women are being prescribed medications not approved by the FDA for use in pregnancy. In fact, from 1996 to 2000, only 2.4% of women received a prescription medication that was rated Category A (i.e., Controlled studies in women fail to demonstrate a risk to the fetus in the first trimester. Risk of fetal harm appears remote.); nearly 50% were rated Category C-X. Extending from this problem, clinicians have little to no pharmacokinetic and pharmacodynamic data by which to adapt dosing regimens specific to pregnancy. It is common practice to apply pharmacokinetic data obtained from men and nonpregnant women to determine dosing during pregnancy despite the dramatic physiologic changes that occur during pregnancy that might affect dosing.
In June 2015, the FDA released new labelling requirements to be used in pregnancy. These new requirements are titled: the Prescription & Lactation Labeling Rule (PLLR). This labelling replaces the standard Category Rankings A, B, C, D and X. The prior categories were deemed oversimplistic and were often inappropriately interpreted as a grading system. The newly implemented PLLR is composed of three sections: (8.1) Pregnancy, (8.2) Lactation, (8.3) Females and Males of Reproductive Potential. The new ‘Females and Males of Reproductive Potential’ section provides information relating to contraception, pregnancy testing and infertility.
The ‘Pregnancy’ and ‘Lactation’ sections each contain a Risk Summary, Clinical Considerations and Data. Taken together, this information is provided to assist clinicians in making an informed decision about medication use in pregnancy and provides more information on both the risks and benefits than previous labelling. The new rule also mandates that if a pregnancy exposure registry exists, it must be listed in the ‘Pregnancy’ section. Such registries facilitate epidemiologic studies of medication use in this vulnerable population.
Several factors contribute to the paucity of pharmacokinetic and pharmacodynamic data in pregnancy. A major barrier is the enormous liability concerns that discourage pharmaceutical companies from studying pregnant women. When studying medications in pregnancy, the risk posed to both the mother and the fetus must be considered. This additional liability is often enough to dissuade pharmaceutical companies from performing such studies. The relatively small market for many pregnancy medications is another factor discouraging involvement of the pharmaceutical industry. Pregnant women account for only 4% of the female US population, according to the Centers for Disease Control and Prevention (CDC), and pregnancy lasts only 40 weeks. Therefore the potential revenue to be gained by these companies for studying medications in this population is relatively small. Big pharma is also aware that women with chronic conditions frequently continue their medication regimens throughout pregnancy regardless of the lack of pregnancy-specific pharmacological data. There is little incentive for pharmaceutical companies to study drugs during pregnancy and assume potential litigation risk because the pregnant woman’s care provider often continues to provide the medication if the clinical circumstances demand that the medication be used despite a lack of precise pharmacologic information.
Further complicating research in this population is the need for long-term follow-up for childhood outcomes. To fully quantify risk for outcomes such as attention deficit hyperactive disorder, follow-up must be adequate. In addition to long lengths of follow-up, large sample sizes are required to document associations with rare birth defects. For example, congenital heart defects (the most common birth defect diagnosed in the United States) occur at a rate of about 1% with an estimated 40,000 affected births each year in the United States, according to the CDC. To demonstrate an increased risk resulting from medication exposure, investigators may need thousands of exposed pregnant women.
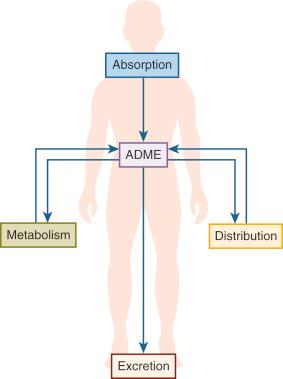
Pharmacokinetics is the study of what the body does to a drug; this includes absorption, distribution, metabolism and elimination (ADME). Each aspect of pharmacokinetics can influence the exposure of the patient to the drug. In practice, the area under the plasma concentration × time curve (AUC) or the trough concentrations are commonly used as surrogate markers to measure drug exposure ( Fig. 48.1 ).
Throughout pregnancy, extraordinary anatomic and physiologic changes occur in the mother. These adaptations impact most maternal organ systems and collectively produce an environment that optimises fetal growth and development. These changes dramatically affect both the pharmacokinetics and pharmacodynamics of a drug. The physiologic adaptations occurring during pregnancy are generally gradual but may change from trimester to trimester. For example, blood pressure decreases early in gestation (lowest point at 20–24 weeks) but typically returns to normal levels by delivery. Others changes persist throughout pregnancy, such as the decrease in plasma proteins.
We will now describe each component of pharmacokinetics (ADME) and discuss how pregnancy can alter each of these processes. This list is not complete but aims to give readers a perspective on how influential these physiologic changes can be on drug exposure to mother and the fetus.
Absorption is defined as the movement of drug into the systemic circulation from the site of administration. Bioavailability is the per cent of the administered drug that reaches the systemic circulation in intact form. When a drug is administered intravenously, it is 100% bioavailable. This is also true for most drugs that are administered intramuscularly, subcutaneously and by inhalation. However, when a drug is administered orally, intraperitoneally, dermally or rectally, the drug is often not fully absorbed or bioavailable. Orally administered medications have the greatest variability in absorption and bioavailability because they are affected by multiple factors such as gastric acidity, gastric transit time, permeability from the gastrointestinal tract, involvement of uptake and efflux transporters, metabolism by intestinal enzymes and hepatic enzymes after entering the portal circulation. Whereas metabolism occurs primarily in the liver, enzymes in extrahepatic tissues such as in the gastrointestinal tract, lungs, the gut wall and gut flora can also contribute to metabolism of certain drugs. Metabolism is influenced by the motility of the gut, enzymatic activity in the gut and the impact of transporters.
This ‘first-pass’ effect dramatically reduces the amount of drug that reaches the systemic circulation. Therefore the term ‘bioavailability’ is commonly used to describe the extent to which a drug is systemically available. Drugs with low bioavailability require a higher oral dose to reach plasma concentrations equivalent to that observed after intravenous administration. Variations in oral bioavailability of drugs have direct clinical consequences. Drugs with low bioavailability typically will have large intersubject variation in drug exposure that may translate into variable clinical effects and potentially side effects.
Numerous maternal changes in pregnancy impact absorption of oral medications. In a nonpregnant woman, gastric acidity is between a pH of 1 and 3. Gastric acidity is reduced in pregnancy, resulting from both decreased production of gastric acid along with increased mucous secretion. Gastric acidity influences ionisation of drugs and thereby absorption. Both weak acids (e.g., aspirin) and weak bases (e.g., caffeine) diffuse more easily in unionized form; the pKa of a drug is the pH at which a drug will be 50% ionized and 50% unionized. Weak acids are more likely to be unionized when the pH of the stomach is lower than pKa of the drug; conversely for weak bases the pH must be higher (i.e., more basic) to remain in unionized form. When the pH is increased in pregnancy, weak acids such as aspirin will have decreased absorption. Conversely, these changes in acidity can increase the absorption of weak bases such as caffeine because they are more likely to be unionized in this environment and more readily cross the membrane.
Pregnant women also commonly experience nausea and vomiting in pregnancy, particularly in the first trimester. More than 80% of pregnant women develop this condition. Nausea and vomiting impact drug absorption through many ways. First, nausea and vomiting can limit a woman’s ability to ingest oral medications. In severe cases, known as hyperemesis gravidarum, women may require intravenous treatment. In addition, a drug’s absorption may vary according to whether it is administered during the fed or fasted state. Nausea and vomiting can impact the woman’s diet, which ultimately affects drug absorption. Medications typically used to treat these conditions, such as antacids, act by decreasing gastric acidity, again ultimately affecting a drug’s absorption. Beyond that, antacids are also known to adsorb some drugs and impact their absorption.
In regards to first-pass metabolism, pregnancy can either increase or decrease the activity of drug-metabolising enzymes located in the gut. Contact of the drug with these enzymes is also increased because progesterone, a smooth muscle relaxant, decreases gut transit time by an estimated 30% to 50% in pregnancy. This increased time for interaction allows for more gut metabolism to occur. Finally, portal venous flow is increased during pregnancy, which may facilitate absorption and increase drug delivery to the liver.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here