Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Surgical hip dislocation (SHD) combined with a sliding osteotomy of the greater trochanter provides a 360-degree overview for correction of structural hip problems and is a safe approach with a low complication rate.
SHD can be used for correction of intraarticular and extraarticular femoroacetabular impingement (FAI; Video 54.1 ), for residual Perthes deformities (Legg-Calvé-Perthes disease [LCPD]), for severe slipped capital femoral epiphysis (SCFE) using the modified Dunn procedure, for avascular necrosis (AVN) of the femoral head, and for open reduction and internal fixation (ORIF) of acetabular fractures.
Surgical hip dislocation provides a direct view of the retinacular vessels for safe resection of cam deformities and enables intraoperative range-of-motion (ROM) testing to ensure complete surgical correction.
Preoperative imaging should include supine and axial radiographs and dedicated magnetic resonance imaging (MRI) of the hip, which includes radial images for definite diagnosis of cam FAI and the distal femoral condyles for measurement of femoral torsion. MRI with intraarticular contrast (direct MR arthrography) enables detection of degenerative changes, which predict long-term failure of FAI surgery and can be further combined with axial leg traction for improved visualization of cartilage lesions. For complex pathomorphologies, 3-dimensional computed tomography (3D CT)–based impingement simulation considerably facilitates surgical planning.
The technique of surgical hip dislocation has been slightly modified since its first description in 2001; currently, a stepped osteotomy of the greater trochanter is performed. A retinacular soft tissue flap is used for the modified Dunn procedure.
Long-term results after correction of FAI, residual Perthes deformity, SCFE, and ORIF of acetabular fractures are favorable, with survivorships ranging from 80% (anterior FAI) up to 93% (SCFE).
Surgical dislocation for femoroacetabular impingement.
Surgical hip dislocation (SHD) was first described by Ganz et al. in 2001, after a thorough analysis of the blood supply to the femoral head, as a technique for safe surgical dislocation of the hip. Open SHD offers the possibility of circumferential corrections and can be combined with additional procedures to relieve intraarticular and extraarticular impingement and associated collateral damage.
The approach can be used for surgical correction of prearthritic conditions such as femoroacetabular impingement (FAI), residual Perthes deformity (Legg-Calvé-Perthes disease [LCPD]), slipped capital femoral epiphysis (SCFE), avascular necrosis (AVN) of the femoral head, synovial disease with formation of loose bodies, and for open reduction and internal fixation (ORIF) of acetabular fractures. In this chapter, we provide a comprehensive overview of indications for SHD, preoperative planning, the surgical technique, long-term results, and complications.
The technique of SHD combined with an osteotomy of the greater trochanter was first described for correction of FAI. FAI represents an early and painful abutment between the proximal femur and the acetabular rim triggered by osseous pathomorphologies that impair range of motion (ROM; Fig. 54.1 ). Two main mechanisms of impingement have been described: (1) Inclusion type FAI (cam type) in which the aspherical femoral head protrudes into the acetabulum and induces shear forces that lead to the typical carpet-like delamination of cartilage and detachment of the labrum; and (2) impaction type FAI (pincer type) in which the femoral head abuts against an excessively prominent acetabulum, leading to cartilage thinning and degenerative labrum tears.
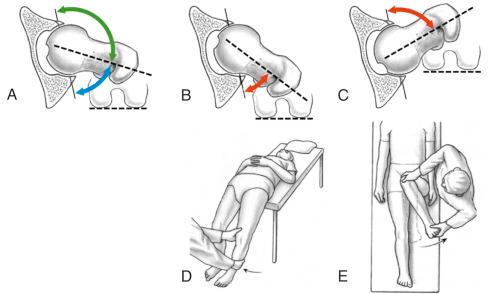
Recently, extraarticular hip impingement has been recognized as an additional but less frequent cause of impingement. Extraarticular impingement can occur anteriorly or posteriorly. Anterior extraarticular impingement occurs secondary to a caudal extension of the anterior inferior iliac spine (AIIS). The so-called subspine impingement occurs between the AIIS and the intertrochanteric region of the proximal femur and is caused by a too prominent caudal extension of the AIIS and/or secondary to low femoral torsion ( Fig. 54.2 ). Posterior extraarticular impingement (ischiofemoral) occurs between the ischial tuberosity and the lesser trochanter and is caused by high femoral torsion and valgus hips ( Fig. 54.3 ).
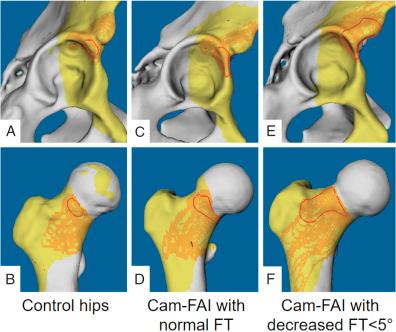
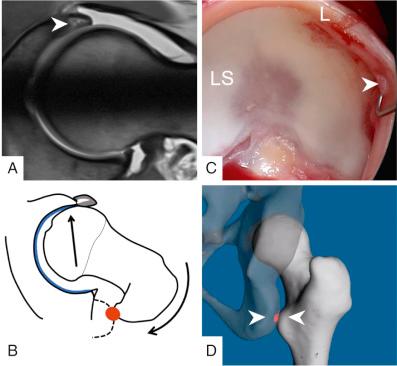
Asphericity of the femoral head-neck junction results from distinct osseous variants. Idiopathic cam-type deformity is the most frequent cam-type deformity (occurring in over 80%) and typically arises from an excessively lateral extension of the epiphysis. Slip-like morphology resembling sequelae of SCFE or postslip morphologies leading to inclusion FAI are less frequently observed. The cam deformity is typically located anterosuperior. The eccentric part of the femoral head-neck junction can slide into the anterosuperior acetabulum during flexion and internal rotation and adduction. Shear stress is induced in the chondrolabral transition zone, which is the first structure that fails. Chondrolabral separation reflects the precursor lesion, which progresses to in-toto delamination of the acetabular cartilage and detachment of the labral base. Damage secondary to inclusion FAI is typically focal but pronounced.
Intraoperatively, the location and extent of the aspherical portion of the femoral head-neck junction is identified using hemispherical plastic templates. The femoral head-neck offset is restored using chisels and a high-speed burr. The torn labrum is trimmed to stable substance, reattached, or can be reconstructed using autologous fascia lata or ligamentum teres grafts. Labrum preservation or reconstruction of the labrum should be achieved whenever possible to achieve a good clinical outcome.
In hips with pincer morphology, acetabular overcoverage restricts the impingement-free ROM. Acetabular cartilage damage is usually restricted to a narrow and circumferential strip, with labral damage usually colocated and typically presents as ossification and degenerative tearing within the labrum. The overcoverage can be localized as an anterior osseous acetabular prominence (e.g., with anterosuperior acetabular retroversion) or generalized to the entire acetabulum (e.g., protrusio acetabuli representing the most severe form of pincer impingement). Rim trimming is performed until impingement-free ROM is achieved, followed by reattachment of the labrum.
Extraarticular FAI occurs either anterior or posterior. Posterior, ischiofemoral impingement is typically located between the ischial tuberosity and the lesser trochanter (see Fig. 54.3 ). Excessive high femoral torsion combined (> 35 degrees) with a valgus deformity (neck-shaft angle > 139 degrees) predisposes to this conflict in extension with or without external rotation in the hip joint. The posterior osseous abutment supposedly leads to a levering mechanism and decentration or hip instability. Clinical diagnosis is established with a positive posterior impingement test or the Flexion, Abduction and External Rotation (FABER) test. Especially in the presence of a cam deformity and acetabular overcoverage, it can be challenging to diagnose ischiofemoral impingement. Computed tomography (CT)–based 3-dimensional (3D) reconstructions of the pelvis and femur followed by a dynamic simulation of hip impingement considerably facilitate surgical decision making in patients with suspected posterior extraarticular FAI ( Fig. 54.4 ).
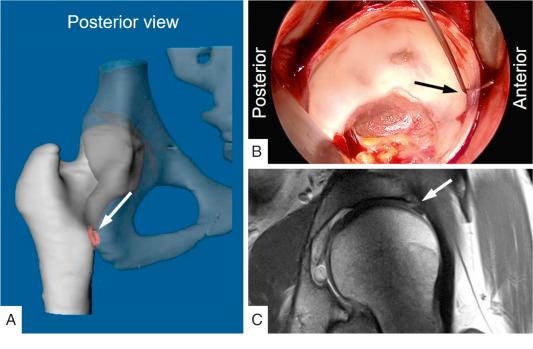
The causal treatment for this condition is a proximal femoral derotational osteotomy ( Fig. 54.5 ). In our institution, this procedure typically is combined with an SHD for an anterior cam resection and for intraoperative dynamic evaluation of hip ROM. A derotational osteotomy will increase the range of external rotation while impairing the range of internal rotation. Thus, a concomitant anterior cam resection is performed on a nearly regular basis in these hips.
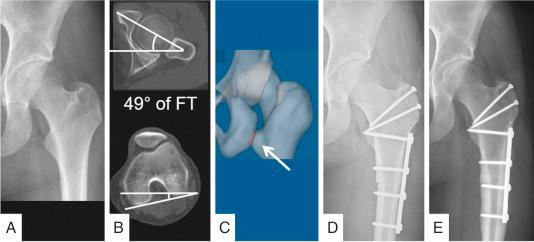
Anterior subspine impingement is typically located between the AIIS and the intertrochanteric region of the proximal femur (see Fig. 54.2 ). This condition can be caused by low femoral torsion, severe acetabular retroversion, or after avulsion fractures of the AIIS. This has been described using CT-based 3D reconstructions of the pelvis and femur and is probably underestimated (see Fig. 54.2 ). The use of intraarticular corticosteroid injections can help to differentiate between anterior intraarticular and extraarticular hip impingement. We also use CT-based 3D reconstructions of the pelvis and femur and dynamic simulation of hip impingement for diagnosis and preoperative planning in these cases (see Fig. 54.2 ) because the clinical diagnosis is difficult. Surgical treatment for these hips is performed using an SHD for cam resection and resection of the intertrochanteric region and/or resection of the AIIS. We use intraoperative dynamic evaluation of hip ROM for testing of impingement-free motion. In the case of persisting anterior FAI after the aforementioned resection, a rotational femoral osteotomy to increase femoral torsion should be considered.
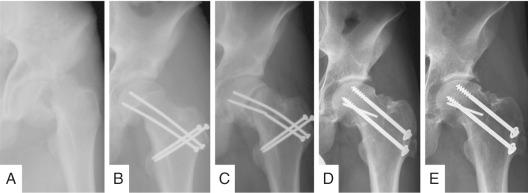
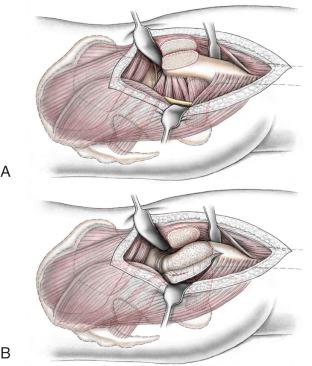
Severe or unstable SCFE is another indication for open surgical treatment. A surgical hip dislocation is performed and the so-called retinacular soft tissue flap is developed in order to perform a modified Dunn procedure for subcapital realignment and fixation ( Fig. 54.6 ). Via a stepwise resection of the most posterior portion of the greater trochanter, a flap that contains the deep branch of the medial femoral circumflex artery (MFCA), periosteum, piriformis muscle, and short external rotators is developed ( Fig. 54.7 ). Callus resection with a short chisel will allow the surgeon to separate the femoral epiphysis from the metaphysis while leaving the epiphysis attached to the posteroinferior retinacular soft tissue flap. After complete resection of callus formation at the posterior aspect of the neck, the physeal scar within the head is removed with a burr. Then, the epiphysis is manually reduced onto the metaphyseal stump. Threaded wires (2 mm) are used for retrograde and antegrade fixation of the epiphysis. There is an ongoing controversy about the indication for this procedure. Historically, in situ pinning had the lowest risk for AVN and became the treatment of choice in many institutions. The downside of in situ fixation is that even large deformations are left uncorrected in these adolescent hips, leaving a high probability of early hip dysfunction. Thus, we recommend treatment of SCFE with a slip angle of more than 30 degrees (moderate to severe slip) and unstable slips with a modified Dunn procedure (see Fig. 54.6 ). Others use this procedure only for severe and unstable SCFE.
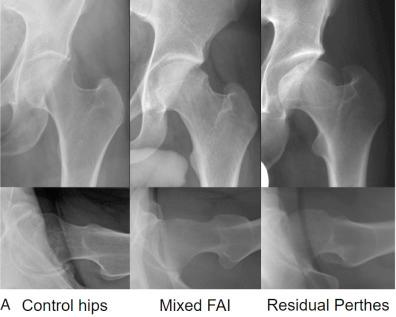
LCPD results typically in an aspherical, mushroom-shaped femoral head as a result of an abnormal development of the growth plate ( Fig. 54.8 ). In flexion and internal rotation, the aspherical portion of the head-neck junction may protrude into the acetabulum and create in shear forces perpendicular to the acetabular cartilage, resulting in cartilage avulsion from the labrum and/or abrasions on the acetabular cartilage. Resection of the aspherical portion of the head to restore ROM is the surgical treatment of choice ; therefore, a large osteochondroplasty of the head-neck junction has to be performed. Another typical deformity in LCPD is a high-riding trochanter, which impairs abductor strength and causes an extraarticular impingement between the greater trochanter and the supraacetabular region (see Fig. 54.8 ). Advancement or distalization of the greater trochanter to perform a relative femoral neck lengthening is necessary to improve the lever arm and restore abductor function. Some authors even suggest a femoral neck lengthening osteotomy (Morscher osteotomy) to restore anatomy and biomechanics. If the deformed and enlarged femoral head is not contained by the acetabulum, intraarticular impingement between the femoral head and the acetabulum results. This has been referred to as hinged abduction or levering out in abduction. A semicircumferential femoral osteochondroplasty can be safely performed via a surgical hip dislocation. By contrast, these large and extensive deformities are difficult to correct via an arthroscopic approach. If containment of the femoral head cannot be achieved by femoral osteochondroplasty alone, a further femoral head reduction can be considered in selected cases. To avoid AVN, a retinacular soft tissue flap is developed for a safe femoral head reduction osteotomy. In our institution, we performed femoral head reduction osteotomies in 11 patients (11 hips) with severe head asphericities resulting from LCPD (10 hips) or disturbance of epiphyseal perfusion after conservative treatment of developmental dysplasia (1 hip) over a 10-year period. Concomitant to severe femoral head deformities, as a result of a premature fusion of the triradiate cartilage the acetabulum becomes dysplastic, with an increased radius, a decreased depth, and a more vertically oriented acetabular roof. This can be the source of joint instability, leading to acetabular rim overload and concurrent chondrolabral lesions. Structural instability is defined as radiographic evidence of acetabular dysplasia with intraoperative confirmation of instability demonstrating subluxation by dynamic examination. Obtaining sufficient acetabular coverage management of acetabular dysplasia in LCPD may require a periacetabular osteotomy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here