Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The advancement of magnetic resonance imaging (MRI) has made high-quality visualization of the normal and pathologic spine, as well as associated neural tissue, readily available. Relative to plain radiography and computed tomography (CT), MRI boasts excellent visualization of soft tissues without exposing the patient to harmful radiation. Within the cervical spine specifically, MRI is routinely used for evaluation of neck pain and radicular symptoms. Several pathologies including spinal stenosis, degenerative disc disease, and tumors can be identified on MRI. However, as with any imaging modality, MRI also has the potential to highlight clinically insignificant pathologies, thus correlation with clinical exam findings is critically important to confirm a diagnosis. Regardless, high-quality visualization of anatomic structures and their associated soft tissues makes MRI a highly valuable clinical and diagnostic tool.
When clinical pathology is suspected in the cervical spine, classic radiographs are often the first imaging study to be performed. However, the inability to visualize soft tissues in detail leaves potential for certain diseases to be overlooked. Conversely, MRI is a noninvasive technique offering excellent soft tissue resolution. Because it does not involve the use of harmful ionizing radiation, MRI has quickly become the imaging modality of choice for many patients. Several MRI sequences exist to image the cervical spine in multiple planes, including T1-weighted spin echo (SE), T2-weighted fast spin echo (FSE), axial gradient-recalled echo (GRE), and more ( Table 1 ). Each sequence is uniquely different to highlight different elements of cervical anatomy and physiology, therefore appropriate sequence selection is imperative to diagnostic evaluation.
| MRI Sequence | Clinical Context | Strengths | Weaknesses |
|---|---|---|---|
| T1-weighted spin echo |
|
|
|
| T1‑gadolinium contrast-enhanced |
|
|
|
| T2-weighted fast spin echo |
|
|
|
| Gradient-recalled echo |
|
|
|
| Short tau inversion recovery |
|
|
|
| Fluid-attenuated inversion recovery |
|
|
|
| Metal artifact reduction sequences |
|
|
|
| Kinetic MRI |
|
|
|
| Susceptibility-weighted |
|
|
With good image resolution and signal-to-noise ratios, T1-weighted SE sequences are best used to evaluate cervical anatomy, fracture lines, and osseous details. Superior depiction of bone marrow intensity also makes T1-weighted imaging a useful tool in identifying processes of bone marrow replacement, such as metastatic disease. However, T1-weighted imaging is less sensitive to many pathologies requiring clear differentiation of tissues. For example, poor distinction between intervertebral discs and the posterior longitudinal ligament or between muscle and nonfatty structures makes adequate assessment of these structures potentially difficult.
T1‑gadolinium contrast-enhanced (T1-Gd) sequences may be considered for detection of necrosis or inflammatory conditions. Increased blood vessel permeability secondary to disease permits accumulation of contrast agent which appears hyperintense to surrounding tissues. However, the use of contrast makes these sequences relatively invasive, time-consuming, and costly to perform.
T2-weighted sequences are produced using longer echo time (TE) and repetition time (TR) to improve visualization of pathologic changes in soft tissues (i.e., intervertebral discs), evaluation of cellular processes altering local water content, and assessment of spinal cord parenchyma for lesions and edema. In contrast to T1-weighted imaging, the spinal cord appears with intermediate signal intensity surrounded by high-intensity cerebrospinal fluid (CSF) on T2-weighted sequences, enabling clear identification of any areas of compromised central canal integrity. Specifically, T2-weighted FSE sequences have largely replaced SE sequences due to their faster imaging speed, improved resolution, superior signal-to-noise ratio, and decreased motion artifact. Disadvantages of T2-weighted FSE sequences include a decreased ability to detect small areas of calcification or hemorrhage, for which susceptibility-weighted MRI (SW-MRI) and T2-weighted GRE sequences provide better differentiation. Additionally, T2-weighted FSE may exhibit overly bright appearances of fat and CSF. Short tau inversion recovery (STIR) and fluid-attenuated inversion recovery (FLAIR) sequences are more appropriate for appreciating these tissues, respectively.
Although both T1-weighted SE and T2-weighted FSE sequences are good at detecting degenerative changes, each has its disadvantages. Neither clearly shows ossification of ligaments, so CT is the imaging study of choice should there be concern for this pathology. Further, fat can pose interference within these sequences, particularly in T1-weighted images. Fat-suppression sequences may therefore be necessary to achieve adequate contrast enhancement within the anatomic area of interest. Artifact, such as CSF pulsation on T2-weighted imaging or esophageal swallowing motions, may be present and should not be mistaken for pathology. Lastly, as with all MRI techniques, it is important to recognize that significant disease may be harbored within the areas between imaging planes on sequences. Gap size may need to be decreased in some cases to visualize tissues with more precise depth.
Should T1-weighted SE and T2-weighted FSE sequences produce inadequate images, axial GRE sequences can be ordered to supplement. Decreased imaging time and susceptibility to motion artifact establish GRE as superior in detecting many degenerative changes such as osteophyte formation and neural foraminal narrowing. Additionally, this sequence is also useful in detecting the presence of blood following spinal cord hemorrhage in the context of trauma or vascular malformation. While GRE demonstrates good sensitivity for extradural disease processes, its sensitivity for intradural pathology is less impressive.
Increasing in popularity are inversion recovery sequences such as STIR and FLAIR. With their reduced scan time and low susceptibility to metal, these sequences are ideal for imaging patients with orthopedic hardware. As mentioned previously, STIR is a fat-suppression sequence that proves useful when adipose tissue is obstructing the images. STIR can be added onto T1- or T2-weighted sequences, but it cannot be used after a gadolinium injection due to inadvertent nulling of certain tissues. Due to its superior sensitivity for detecting edema, STIR sequences are commonly ordered for the evaluation of traumatic injury. FLAIR sequences may be added onto T2-weighted scans for suppression of motion artifact caused by water, making them a preferred sequence for pediatric patients or those who cannot remain supine for extended periods of time. By attenuating the high-intensity signal of CSF, these sequences can better distinguish the spinal cord, CSF, and intervertebral disc for evaluation of degenerative changes. FLAIR further serves as a valuable tool in assessment of demyelinating disease, such as multiple sclerosis.
Artifact reduction is also achievable using metal artifact reduction sequences (MARS). These sequences are particularly useful for imaging the cervical spine in patients with metal implants, as use of a low-powered magnet reduces the size and intensity of metal artifact produced by magnetic field distortion without sacrificing signal-to-noise ratio.
Kinetic MRIs, such as flexion/extension sequences, are newly emerging techniques used to assess the effects of movement and gravity on the cervical spine. Utilizing these methods may allow physicians to unveil motion-dependent pathologies not seen in more classic imaging orientations. Several pathologies can be exacerbated with movement and should be evaluated using kinetic MRI, including central spinal stenosis, spondylolisthesis, and rheumatoid arthritis (RA). Furthermore, cervical alignment may also be better assessed with these techniques, as the effects of gravity contribute to a more accurate clinical evaluation of spinal curvature.
Susceptibility-weighted MRI (SW-MRI) is an emerging MR technique that has demonstrated improved visualization of calcified structures, such as osteophytes. SW-MRI has high sensitivity and specificity for identifying and locating osteophytes relative to classic T1- and T2- weighted images, which often fail to distinguish osteophytes from disc herniations. Whereas T1- and T2-weighted sequences show both as hypointense, SW-MRI depicts calcified structures with a hyperintense signal, a useful benefit for preoperative planning not available with conventional 2D radiography.
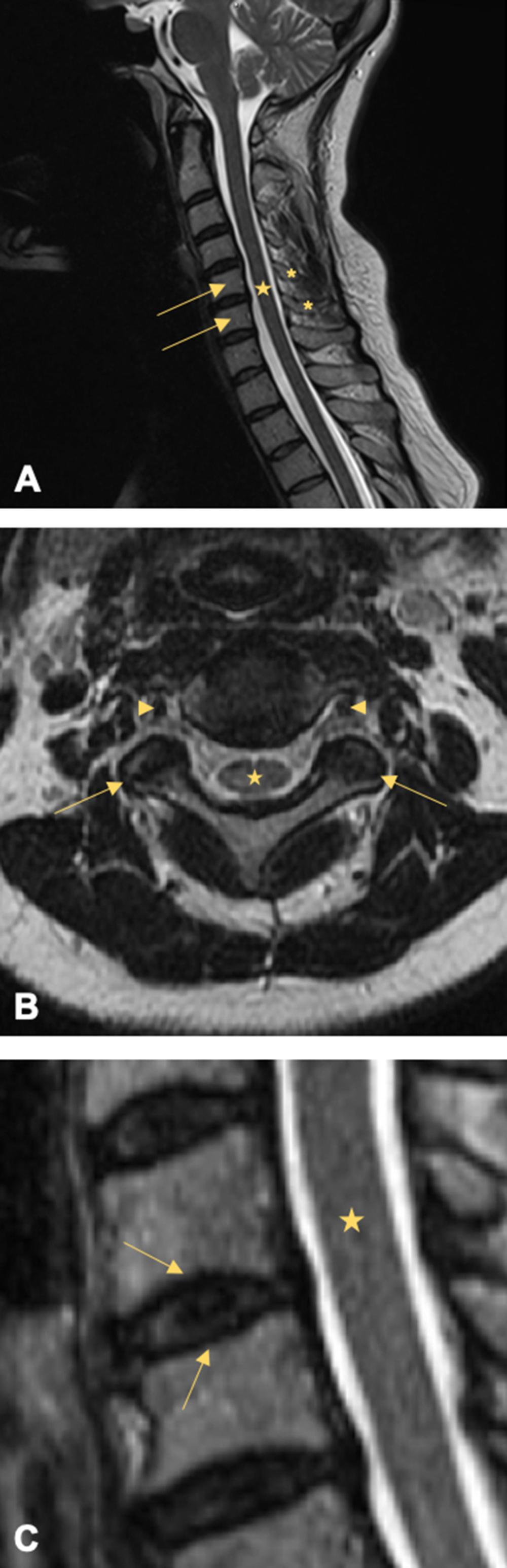
The cervical spine consists of seven vertebrae arranged vertically from the base of the skull to the level of the shoulders. In coordination with associated muscles, tendons, and ligaments, these bony structures provide structure, support, and flexibility to the neck while serving to protect the spinal cord coursing within. Generally, the cervical spine shares characteristics with other spinal segments, including a vertebral body, vertebral arches, transverse processes, a spinous process, and facet joints. In midsagittal view, MRI of the healthy cervical spine shows small lips protruding from the anteroinferior border of the vertebral bodies, facilitating a normal lordotic curvature from C2-T2 with the apex around C4-C5. In contrast, the superior faces appear concave in the lateral direction and convex anteroposteriorly, and the vertebral body walls are slightly concave in nature. The fatty composition of the marrow within the healthy vertebral body conveys a bright signal intensity to T1-weighted images. Moving parasagittally brings the transverse processes into frame, which serve as significant points of attachment for various muscles and ligaments and provide conduits for neurovasculature. The vertebral artery and venous systems can be seen in the axial perspective passing vertically through the foramen transversarium of the transverse processes on each side of the vertebra. Notably, the spinous processes of the typical cervical vertebrae demonstrate a classically bifid structure. Representative MRI images of the normal cervical spine are shown in Fig. 1 .
There are a few exceptions to these anatomic generalizations within the cervical spine. C1, often referred to as the atlas, is unique in its replacement of a vertebral body with the anterior tubercle. As the only vertebra without a vertebral body, the atlas assumes a ring-like shape and connects the occipital condyle above with the proper cervical spine below via the atlanto-occipital joint. Extensions of the anterior longitudinal ligament and ligamentum flavum comprise the atlanto-occipital membranes, which support the atlanto-occipital joint in conferring a majority of the flexion/extension motion to the head. Inferior to the atlas is the C2, or axis, so named due to the bony odontoid process protruding upward into the ring of C1 with which it forms the atlanto-axial joint. This synovial joint permits the atlas to rotate around the axis and accounts for nearly 50% of the rotational motion of the head. Because they exhibit such unique morphologies, C1 and C2 are classified as atypical vertebrae. Additionally, the most inferior vertebra of the cervical spine, C7, has a number of distinguishing features. Known as vertebra prominens, C7 can be identified on midsagittal view by its particularly prominent spinous process, which is not bifid as in the rest of the cervical spine. This specialized projection ensures optimum fit with T1 in the cervicothoracic junction and provides attachment points for more muscles than any other cervical vertebra. Furthermore, the foramina in the transverse processes where the vertebral arteries normally pass are absent at this level and will not be seen on axial view.
At each vertebral level except C1, the laminae and pedicles merge laterally into lateral masses before separating into the paired superior and inferior articular processes. The inferior processes from the vertebra above articulate with the superior processes of the vertebra below to form the facet joints. Formally termed zygapophyseal joints, these true synovial joints contain cartilage and menisci to permit small movements across the motion segment while restricting hyperflexion and hyperextension. Movement across each motion segment is quite limited; however, the cumulative effect across the entire spine enables significant rotation, flexion, extension, and lateral bending. Notably, whereas these joints are oriented vertically within the lumbar spine, their 45-degree orientation within the cervical spine facilitates flexion and extension. Paired with the abundance of proprioceptive and pain receptors innervating the area, the susceptibility of the facet joints to age- or trauma-related degeneration denotes a plausible role for the facet joints in chronic neck pain. Visualization of the facet joints is best achieved with T2-weighted imaging, which shows a smooth homogenous signal of the hyaline cartilage overlying the low-signal cortical bone. Despite the paucity of literature surrounding visualization of the normal facet joints with MRI, this imaging method becomes increasingly important in the context of pathology such as joint inflammation and age-related cartilage degeneration.
With the exception of the atlanto-occipital and atlanto- axial joints, intervertebral discs are interspersed between adjacent vertebral bodies throughout the cervical spine. These avascular structures provide support to vertebral bodies, permit flexibility throughout the full range of head and neck movements, and cushion the impact of various stresses and loads on the cervical spine. The anatomy of the intervertebral disc consists of two basic components. The nucleus pulposus is the soft inner core of mucoprotein gel that assists in providing cushioning and flexibility to the disc. Surrounding the nucleus pulposus is the annulus fibrosus, a durable external layer composed of concentric rings of alternating obliquely oriented collagen fibers functioning to distribute forces, protect the inner core, and stabilize the motion segment. MRI is used to assess the integrity of the intervertebral discs through quantification of disc hydration primarily based on proton density and water content. Specifically, normal discs exhibit a bright signal within the nucleus pulposus on both T1- and T2-weighted images due to its high water and proteoglycan content, often with a horizontally oriented area of decreased intensity at the core’s center in the adult. The more fibrous composition of the annulus fibrosus emits a darker signal, generating a marked distinction between the nucleus pulposus and annulus fibrosus in the healthy disc ( Fig. 1 C). Coronal views show the superior face of the disc is concave, while the inferior face is convex. In midsagittal view, one can determine that the six intervertebral discs of the cervical spine are thinner than the greater load-bearing discs of the lumbar spine but thicker than those of the less-mobile thoracic region. The discs of the healthy cervical spine also demonstrate greater thickness anteriorly, which in conjunction with the lipped nature of the vertebral bodies facilitates a lordotic curvature. Normally, an intervertebral disc will be entirely contained within the anterior and posterior margins of the vertebral bodies and will not vary in height by more than 25% compared to adjacent normal disc spaces.
Vertebral endplates mark the transition between the intervertebral disc and the adjacent vertebral body. Without a blood supply of its own, the intervertebral discs rely on the transport of nutrients and small amounts of blood from the subchondral bone through the hyaline cartilage and porous bone of the vertebral endplate for nourishment. These structures also function to buffer disc pressures on the vertebral bodies and limit protrusion, provide points of insertion for the inner fibers of the annulus, and serve as growth plates responsible for endochondral ossification. On T1-weighted MRI, normal endplates display uniform intensity with the vertebral body and a clear demarcation from the adjacent intervertebral disc, whereas alterations in signal intensity relative to the vertebral body indicate endplate abnormalities ( Fig. 1 C).
One of the most critical functions of the vertebral column is to house and protect the spinal cord within a spinal canal created by stacked vertebral foramen. The spinal cord itself is immediately surrounded by the pia mater, subarachnoid space, arachnoid mater, and dura mater. At the level of each intervertebral disc, bilateral spinal nerves project off of the spinal cord to innervate their respective body segments. The entirety of the cervical spinal cord is best visualized in midsagittal view. On T1-weighted images, the spinal cord will appear with an intermediate signal due to abundance of lipids within the cord. However, due to low water content of the cord, this structure emits low-intensity on T2-weighted images.
Despite the paucity of MR-based studies describing the normal configuration of the cervical canal, dural tube, and cord, a few generalizations can be made. From the axial and sagittal perspectives of T2-weighted sequences, the healthy spinal cord will show a homogeneous signal without intrinsic abnormalities. Typically measured on T2-weighted images, canal size varies by vertebral level, as well as by the sex and age of the patient. Canal diameter normally tapers from the first vertebrae to the third vertebrae, where the spinal cord undergoes a slight enlargement before retaining a more uniform diameter throughout the remainder of the cervical spine. Notably, cross-sectional area, sagittal diameter, and axial diameter of the spinal cord peak in the third decade of life and tends to decrease thereafter ( Table 2 ).
| Age | Men | Women |
|---|---|---|
| 20–29 | 12.7–14.4 mm | 12.6–14.3 mm |
| 70–79 | 11.0–13.6 mm | 10.8–13.5 mm |
In sagittal view, the entirety of the vertebral column assumes a slightly S-shaped appearance to efficiently perform the necessary functions of each spinal region ( Fig. 1 A). Generally, the curves of the spinal column serve to absorb shock, provide balance, and permit motion. To aid in supporting the weight of the head, the cervical spine maintains a lordotic curvature that should be apparent in sagittal view of any radiograph or MRI sequence. The extent of lordosis is best measured on upright/standing X-ray, as conventional MRI is performed in the supine position where gravity can alter the patient’s typical alignment. However, if upright/standing films are not available, methods do exist to estimate the extent of lordosis on MRI (in supine position), such as Cobb angles. However, the translation of these measurements to MRI sequences has been only scarcely reported in literature and their validity is yet to be established.
The soft tissue of the cervical spine refers to the muscles, ligaments, fascia, blood vessels, nerves, and lymphatics that traverse and supply structures of the region.
Musculature accounts for the majority of soft tissue volume and contributes to movement of the head, neck, upper back, and shoulders. At the dorsolateral aspect of the cervical spine from superficial to deep are the trapezius, splenius capitis, splenius cervicis, levator scapulae, rotatores, rectus capitis, obliquus capitis, and semispinalis muscles. Anterolaterally are the platysma, sternocleidomastoid, strap muscles of the larynx, hyoid muscles, scalenes, longus cervicis, and longus colli muscles. The bodies of these muscles are illustrated well on nonfat-saturated T1-weighted MRI, while T2-weighted imaging allows assessment of edema and fluid.
Muscles are assisted in providing stability to the cervical spine by a network of ligaments, including the anterior longitudinal ligament (ALL), posterior longitudinal ligament (PLL), and posterior ligamentous complex (PLC). The ALL and PLL course along the anterior and posterior aspects of the subaxial vertebral bodies, respectively, demonstrating a narrow, thick morphology over the bodies but stretching wide and thin while coursing over the intervertebral discs. The PLC is located posterior to the neural arch, consisting of the ligamentum flavum (LF), interspinous ligaments, and ligamentum nuchae. Within the cervical spine, the interspinous ligaments are particularly thin and poorly developed. Due to their fibrous composition, ligaments appear as dark bands on all MRI pulse sequences, with discontinuities in signal void suggesting acute ligament rupture.
Structures of the cervical spine are supplied by branches of the vertebral, ascending cervical, deep cervical, and occipital arteries. The vertebral arteries originate from the subclavian arteries, coursing between the longus colli and anterior scalene before entering the vertebral column at the level of C6 and ascending through the transverse foramina toward the foramen magnum. Anterior and posterior vertebral veins accompany the vertebral arteries, surrounding them in a venous plexus at the lateral aspect of the spine. Upon entering the spinal canal, the left and right vertebral arteries merge to form the basilar artery that supplies the brainstem. Several segmental radicular arteries stem from the vertebral arteries, mostly directed toward the ALL, intervertebral disc, and vertebral body. Others feed into the muscles of the neck, where they anastomose with branches of the ascending cervical artery traveling between the anterior scalene and longus capitis along the transverse processes. The deep cervical artery arises from the costovertebral trunk and travels between the facet joints toward the posterior spinal muscles, while the occipital artery stems from the external carotid artery on its way to supply the posterior scalp. Conventional MRI can be used to evaluate vasculature in the cervical spine. Because MRI cannot recognize flow, however, vasculature is illustrated as focal areas of absent signal, or “flow voids” ( Fig. 1 B). Normal vasculature should exhibit a single lumen and generally follow the course outlined above. Administration of contrast dye in magnetic resonance angiography (MRA) enables enhanced visualization of these structures and is the preferred method for their assessment.
Assessment of the nerves and the foramina through which they pass is a critical component MR-based evaluation of the cervical spine. On midsagittal view, the spinal cord can be appreciated extending inferiorly from the medulla oblongata and pons. At each vertebral level, branches stem from the spinal cord to form the eight spinal nerves of the cervical spine, termed C1 through C8. These then travel along the costotransverse lamella and between the anterior and posterior tubercles of the transverse processes before exiting the vertebral column via the intervertebral foramina toward their respective dermatomes and myotomes. Parasagittal views depict normal spinal nerves with intermediate intensity surrounded by high-intensity fat on T1-weighted imaging. Because of the 45-degree oblique orientation of the intervertebral foramina, however, oblique imaging offers optimal viewing to assess whether compression or irritation may be contributing to any pain or dysfunction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here