Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since flexible endoscopy of the colon was introduced in 1963, it has become the gold-standard diagnostic test for evaluation of colonic disease. Improvements in technique and technology have also led to advances in therapeutic procedures, and the boundary between endoscopic and surgical procedures is becoming increasingly blurred. A good understanding of both the technique and technology is essential for an endoscopist to perform high-quality, safe endoscopy. This chapter gives an insight into how lower gastrointestinal (GI) endoscopy is influencing the practice of colorectal surgery.
Indications for colonoscopy or flexible sigmoidoscopy must be weighed against the risk/benefit profile. Diagnostic colonoscopy has a higher risk of complications relating to sedation and bowel preparation than diagnostic flexible sigmoidoscopy. Flexible sigmoidoscopy is also quicker, cheaper and easier to perform, and detection of distal pathology can be considered as a marker for possible proximal pathology, prompting full colonoscopy.
The only absolute contraindications are a competent patient who is unwilling to give consent or a known free colonic perforation. Relative contraindications include: acute diverticulitis, immediately post-operative patients, a recent myocardial infarction (within 30 days), acute pulmonary embolism, severe coagulopathy (particularly for therapeutic procedures) or haemodynamic instability. In fulminant colitis, a limited examination to ascertain extent of disease and acquire confirmatory biopsies is often helpful. In general, colonoscopy or flexible sigmoidoscopy is considered to be safe in pregnancy but should only be performed for strong indications and after careful consent and liaison with an obstetrician.
Checklists prevent errors, have a positive impact on patient morbidity and mortality in surgical settings and are now commonplace, or mandatory, in many endoscopy units.
Sedation during colonoscopy is the subject of much debate and research. A large multicentre European audit showed that most colonoscopies were done using moderate (conscious) sedation and that although deep sedation was associated with shorter procedure times and fewer technical difficulties, it was also more resource-intensive and required more hospitalisations for complications. American Society of Gastrointestinal Endoscopy recommendations are that routine use of deep sedation in average-risk patients cannot be endorsed. A recent British position statement noted that the need for deep sedation and anaesthesia is increasing because of the growing complexity of GI endoscopy. Flexible sigmoidoscopy is most often performed unsedated, as the use of intravenous sedation would negate many of the potential benefits of the procedure. Unsedated colonoscopy is certainly possible with few complications and good acceptability. Nitrous oxide (Entonox) can be a useful adjunct in unsedated patients as it is short acting and reversible, but does have a cost implication and is implicated in climate change, as it is 300 times more potent as a greenhouse gas than carbon dioxide.
Research and audit have identified continued avoidable morbidity and mortality from sedation. Recommendations are for competency-based formal training for all healthcare professionals involved in sedation.
Insertion technique varies even amongst expert colonoscopists. Technique depends on local circumstances, sedation practice, endoscopist preference and equipment available. However, there are some basic principles that are recognised to contribute to safe, efficient colonoscopy.
Most skilled colonoscopists now adopt the one-person, single-handed approach, where the right hand is used to manipulate the shaft and the left hand operates the angulation controls. Tip control is gained by a combination of up/down angulation with the large wheel and clockwise/anti-clockwise torque applied with the right hand. Left/right angulation using the small wheel is used for maintaining the luminal view while torque is being applied with the right hand.
A digital rectal examination should be performed to lubricate the anal canal and detect any anal and distal rectal pathology before insertion. Intubation of the anus should be under direct visualisation. The initial view is often a ‘red-out’ because of the lens pressing against the rectal mucosa. Gentle insufflation, slow withdrawal and small amounts of tip angulation are used to gain a view of the lumen. Rectal retroflexion is best performed at the start of the procedure to identify any distal pathology.
Pull back more, push in less. The first rule of good colonoscopy is to keep the shaft straight. This allows accurate tip control, prevents stretching of the mesentery, minimises discomfort and shortens the colon by a ‘concertina’ effect, telescoping the bowel wall over the shaft. Pulling back often reduces acute angles of bends, disimpacts the tip of the scope and improves the view. In contrast, excessive pushing of the scope often results in formation of large loops, excessive pain, loss of one-to-one tip control and increases the risk of iatrogenic perforation.
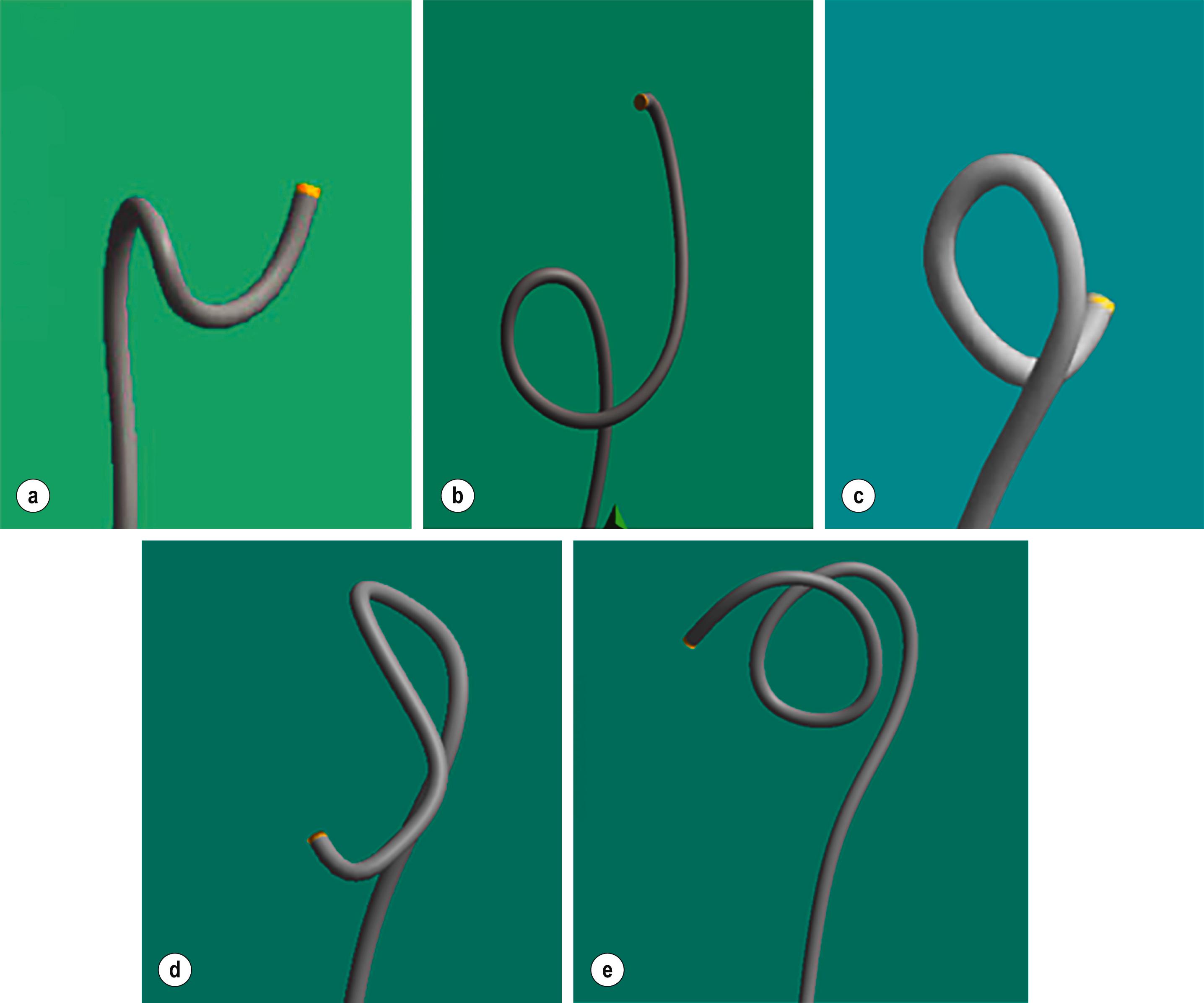
Use torque frequently. Twisting clockwise or anti-clockwise with the right hand applies torque to the shaft of the scope. With a straight shaft and bent tip, use of torque will provide lateral movement at the tip and help to stiffen the scope to prevent looping during advancement. Application of torque is also essential for loop resolution. Without the use of an image guidance device, the application of torque will be determined both by frequency of loop type and ‘feel’ of the instrument. The majority of sigmoid loops (N-loops, 80%; alpha loops, 10%) require clockwise torque and pull-back to resolve; atypical loops (reverse sigmoid N-spiral, 1%; reverse-alpha, 5%) require anti-clockwise torque.
Minimise insufflation. Pain or discomfort during colonoscopy is often caused by stretching of the bowel wall by excessive gas insufflation. Pneumatic perforation of the right colon from over-insufflation has been reported. Frequent suctioning of gas prevents this and may often allow progression of the tip through the colon by the concertina effect. The use of carbon dioxide rather than air has been shown to cause less discomfort and is widely recommended. The use of water-aided (either water-immersion or water-exchange) colonoscopy is also now advocated to improve comfort scores and may improve adenoma detection rate.
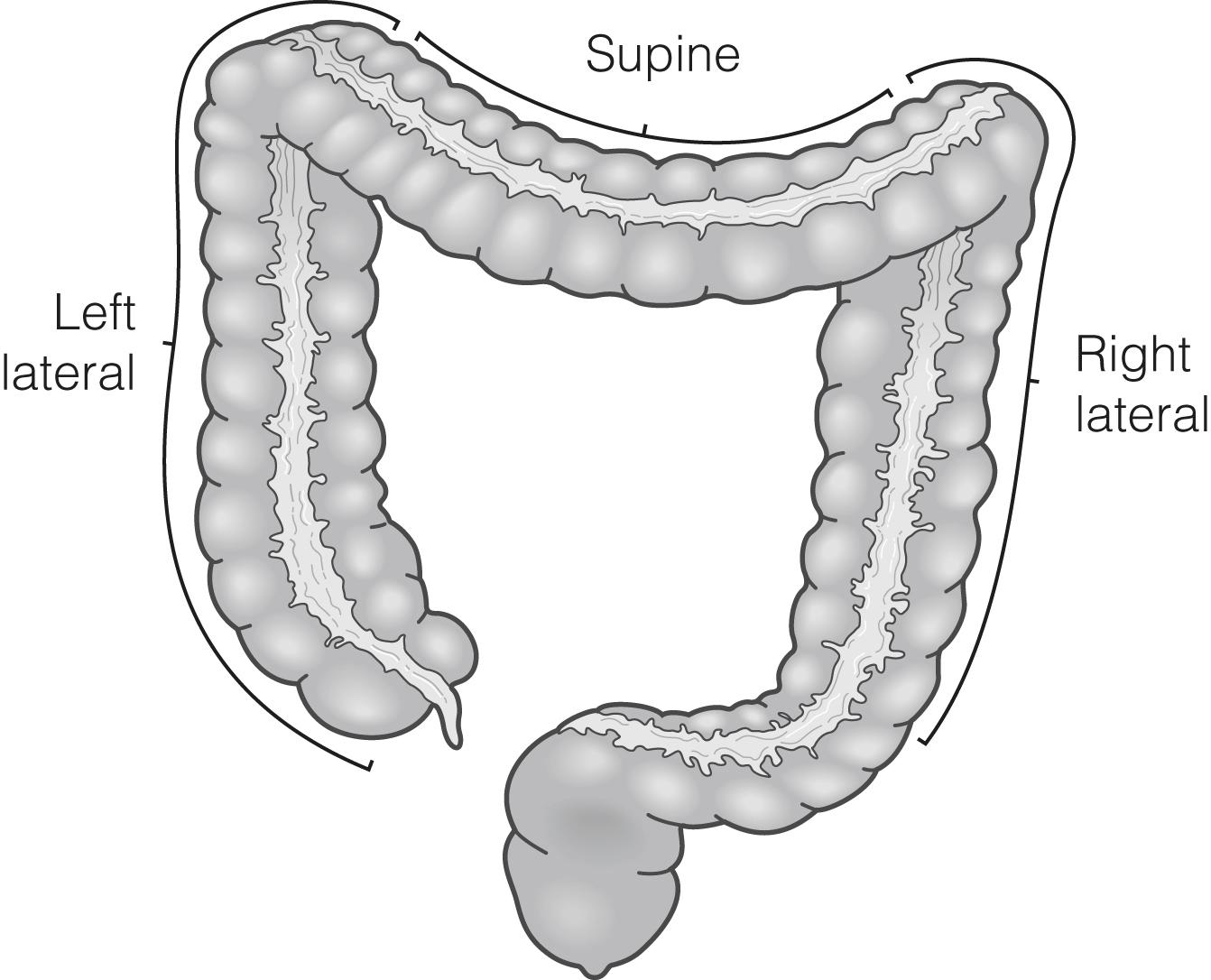
Moving the patient’s position from the left lateral position during both insertion and withdrawal can shift both fluids away from, and air into, the uppermost segment of bowel, preventing unnecessary suctioning of fluid and insufflation of gas. It can provide mechanical advantage by opening up acute bends, especially at the rectosigmoid junction, splenic and hepatic flexures. The effective use of gravity to assist the passage of the endoscope is a simple, technique that is easily learnt. It has been shown to be effective in promoting endoscope tip advancement in two-thirds of cases, but it does require cooperation from the patient and can be difficult if heavy sedation or general anaesthesia is used ( Fig. 1.1 ). If water immersion or exchange is used, the patient should remain in the left lateral position while negotiating the left colon, as the water helps weigh down the sigmoid, minimising loop formation by reducing acute bends and tight angulations.
The use of abdominal hand pressure aims to prevent the shaft of the endoscope looping by opposing pressure close to the anterior abdominal wall. Pressure is best used to prevent a loop forming rather than applying it to an already formed loop, which is unlikely to be successful and may increase the discomfort felt by the patient. Specific pressure on anterior-protruding loops is more likely to be helpful than non-specific pressure. Magnetic imaging devices can help with guided pressure, although efficacy in promoting tip advancement is less than for patient position change, as many loops do not protrude anteriorly. The use of deep inspiration can also be used to splint the diaphragm and provide pressure on the splenic and hepatic flexures if external pressure is unsuccessful.
Magnetic imaging systems (ScopeGuide, Olympus Optical Company; ScopePilot, Pentax Medical) use low-voltage magnetic fields to produce a real-time, three-dimensional image of the entire colonoscope shaft in both anteroposterior and lateral views, allowing the colonoscopist to visualise the configuration of the scope within the patient ( Fig. 1.2 ). This can help determine if there is an anterior component to a loop and so assist with loop resolution, as well as aiding accurate tip location. A sensor can assist with accurate hand-pressure placement.
![]() Meta-analysis of eight randomised controlled trials has shown real-time magnetic imaging to be of benefit in training and educating inexperienced endoscopists and improves the caecal intubation rate for experienced and inexperienced endoscopists.
Meta-analysis of eight randomised controlled trials has shown real-time magnetic imaging to be of benefit in training and educating inexperienced endoscopists and improves the caecal intubation rate for experienced and inexperienced endoscopists.
It should be remembered that the aim of colonoscopy is to visualise the whole of the colonic mucosa to identify pathology. A systematic review of back-to-back studies has shown a polyp miss rate at colonoscopy of 22%, even in expert hands, although most missed polyps were small (<1 cm). All studies investigating miss rates have shown a variation in performance between endoscopists, and this can be wide even with expert examiners (>10 000 procedures), with sensitivities ranging from 17–48% in one large study. This implies that there is a link between individual technical skill and outcome measures. Studies looking at the causes of post-colonoscopy colorectal cancers have shown that up to 89% may be avoidable, although tumour biology may be more important than endoscopist factors.
Recent publications have stressed the importance of spending sufficient time inspecting the colonic mucosa on withdrawal as a key marker for the adequacy of the examination.
![]() The current recommendation is that colonoscopists should spend more than 6 minutes during withdrawal inspecting the colonic mucosa in colonoscopies with normal results. A landmark study looking specifically at withdrawal time found that endoscopists who spent longer than 6 minutes on withdrawal in a negative colonoscopy had significantly higher adenoma detection rates (ADR) than quicker examinations, but there was no advantage in taking over 10 minutes.
The current recommendation is that colonoscopists should spend more than 6 minutes during withdrawal inspecting the colonic mucosa in colonoscopies with normal results. A landmark study looking specifically at withdrawal time found that endoscopists who spent longer than 6 minutes on withdrawal in a negative colonoscopy had significantly higher adenoma detection rates (ADR) than quicker examinations, but there was no advantage in taking over 10 minutes.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here