Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Preoperative assessment of leg length inequality should include a history, physical examination, and radiographic evaluation, including templating.
Preoperative education of the patient should include discussion of the patient's perception of leg length discrepancy and a discussion of the possibility of a postoperative leg length discrepancy.
Templating to plan leg length equalization involves planning for socket and stem placement, as well as neck resection levels and offset.
An intraoperative system is useful to assess leg lengths before dislocation of the native hip and after placement of prosthetic components.
Postoperative management of true and apparent leg length inequality may include physical therapy, a shoe lift, and, in rare cases, revision surgery.
True limb length is usually defined as the distance from the anterior superior iliac spine (ASIS) to the medial malleolus. True leg length inequality is defined as lengthening or shortening of this measurement as compared with the contralateral limb. Apparent leg length is defined as the distance from the umbilicus to the medial malleolus; thus, an assessment of the coronal plane equality of the pelvis or spine must be included in the evaluation. Table 109.1 lists the possible combinations of true and apparent leg lengths and their causes.
| Combination | Cause |
|---|---|
| TLL and ALL equal | Limb length is equal, pelvis is balanced. |
| TLL and ALL unequal same amount | Limb length is unequal, pelvis is balanced. |
| TLL equal and ALL unequal | Pelvic obliquity exists. |
| TLL unequal and ALL equal | Limb length inequality and compensatory pelvic obliquity are present. |
In 1979, Sir John Charnley stated that overlengthening of up to 1 cm can be justified because “It permits active rehabilitation … and patients very soon become adjusted to 1 cm overlengthening.” Nonetheless, in most situations with careful preoperative templating and intraoperative trialing, and with the neck length and offset options available with current prosthetic components, leg length discrepancies can be minimized.
No precise definition has been put forth for leg length inequality following total hip arthroplasty (THA); therefore, its prevalence following THA remains unknown. Incidence varies from 1% to 27%. Mean leg length discrepancy after hip arthroplasty as reported in the literature ranges from 2.8 to 11.6 mm, with some series reporting greater variability (1–15.9 mm). Leg length inequality is perceived in approximately 32% to 43% of patients with a substantial (defined as > 1 cm) limb length discrepancy following THA.
Notable leg length inequality may be associated with gait disorders, back pain, nerve injury, and the need in severe cases for revision surgery. Nerve injury is among the most feared and difficult to manage consequences of leg lengthening. Although some authors have documented an amount of lengthening associated with sciatic nerve palsy, the exact amount by which a limb can be lengthened is unclear. However, the majority of studies show that a range of 2 to 2.5 cm is safe in most patients. (See Chapter 110 for more information. ) Leg length inequality can give rise to patient dissatisfaction, which can adversely affect an otherwise good outcome and is a common reason for litigation following THA.
To minimize the chance of problems associated with leg length inequality, the surgeon should take precautionary steps both before and during the operation.
Evaluation should begin with a thorough history and physical examination. Patients should be asked if they perceive any leg length inequality or have any history of unequal hemming of pants or the tendency to flex one knee while standing. A history of prior femur or tibia trauma or surgery, spinal deformity or surgery, hip dysplasia, muscular dystrophy, or poliomyelitis may be associated with leg length inequality. Physical examination can include an assessment of true and apparent leg length inequality, contractures around the hip joint, spine curvatures, and pelvic obliquity. Clinical methods such as tape measurement and standing blocks can be used as screening tools for measurement of leg lengths.
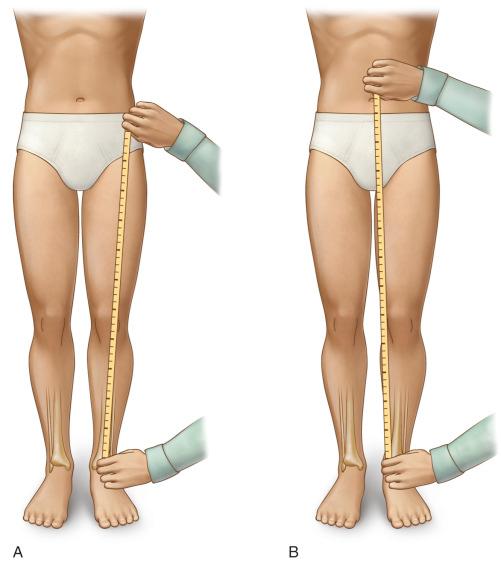
A tape measure can be used to assess both true and apparent leg lengths. In the estimation of true leg lengths, the tape measures the distance from the ASIS to the medial malleolus; this reflects the actual length of the extremity. The range of error of this measurement has been reported to be 0.5 to 1.0 cm. This is also known as the direct method of measuring leg length ( Fig. 109.1 ). However, difficulty in identifying bony prominences, particularly in obese patients, and angular deformities in the lower limb can contribute to error when this clinical measurement tool is used.
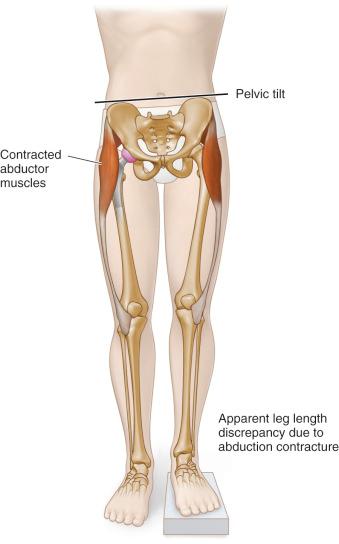
Apparent leg lengths are measured from the umbilicus to each medial malleolus. When a patient has apparent leg length inequality, despite true leg lengths being equal, the patient feels that one limb is longer, and the measurement from umbilicus to medial malleolus on that side is longer. Apparent leg length measurement takes into account contractures around the hip and lumbar spine pathology, both of which can lead to pelvic obliquity. An abduction contracture of the hip, which is common in the early postoperative period after hip arthroplasty, results in an apparent leg length discrepancy on the involved side, but an adduction contracture of the hip has the opposite effect ( Fig. 109.2 ).
Eichler described several potential sources of error when measurements are obtained using a tape measure, including poor reproducibility of finding the ASIS and abduction or adduction contractures of the hip. Beattie and colleagues reported on the reliability of tape measure method (TMM) measurements. They found low reliability (interclass correlation coefficient [ICC] of 0.668; ICC is a descriptive statistic that describes how strongly units in the same group resemble each other) when measurements were obtained by different examiners (interobserver variability). However, when the mean value of paired measurements taken by the same observer was used, intraobserver variability was much lower (ICC, 0.910). Investigators concluded that the reliability of tape measure measurement improved when the mean value of repeated measurements by the same observer were compared with measurements by other observers.
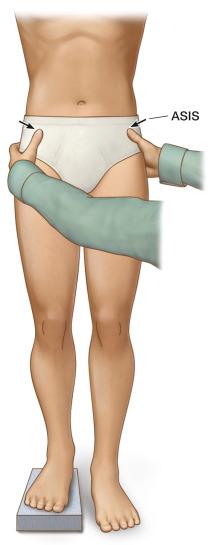
The use of blocks placed underneath the patient's foot is known as the indirect clinical method of assessing leg length inequality. It is helpful in differentiating fixed from flexible pelvis obliquities. Causes of fixed pelvic obliquities include lumbosacral fusion and severe lumbar degenerative scoliosis as well as previous pelvic fracture. The surgeon can inspect and palpate the spinal curvature and pelvic tilt; then, the pelvis should be leveled by placing a series of blocks under the short leg until the spinal curvature and pelvic tilt disappear ( Fig. 109.3 ). If the pelvic tilt corrects, then the pelvic obliquity is flexible; if not, the patient has a fixed pelvic obliquity and will be unable to compensate for any change in leg lengths. Regardless of whether the patient has a fixed or flexible pelvic obliquity, the height of the block that the patient identifies as making the patient feel equal indicates the amount of length discrepancy that the surgeon may consider correcting.
Hanada and colleagues studied the reliability and validity of measuring leg length inequality using the iliac crest palpation and block correction method in 34 healthy volunteers with simulated leg length inequality; they compared clinical observations with those obtained using standing anteroposterior (AP) pelvis radiographs. Iliac crest palpation underestimated the leg length discrepancy by a mean of 4 mm. Similar findings have been reported by other authors.
Radiographs may be used to confirm clinical measurements and the following:
Assessment of radiographic leg length inequality
Preoperative templating, including component sizes, component position, offset and neck osteotomy height
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here