Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hypoplastic left heart syndrome (HLHS) is a spectrum of disease characterized by underdevelopment of the left ventricle with obstruction or atresia of ventricular inflow and outflow. HLHS accounts for approximately 2% to 3% of all cases of congenital heart disease, with a slight male predominance. HLHS is most commonly isolated, but extracardiac anomalies occur in up to 30% and a variety of genes and syndromes may be associated.
The structural defects of HLHS include varying degrees of hypoplasia of left heart structures: hypoplastic ascending aorta and arch (often with discrete coarctation), aortic valve atresia or stenosis, hypoplastic left ventricle, and mitral atresia or stenosis ( Fig. 73.1 ). Patent ductus arteriosus (PDA) and patent foramen ovale or atrial septal defect (ASD) are essential for survival. The ventricular septum is intact, and endocardial fibroelastosis or thickening of the left ventricular endocardium may be present. Right heart structures are typically enlarged, and the tricuspid valve may be abnormal and regurgitant.
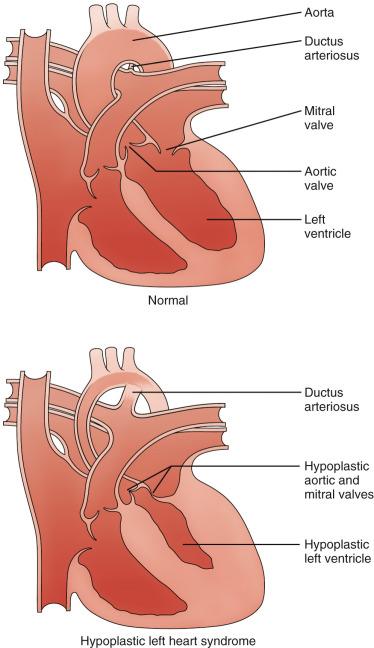
Both the pulmonary and systemic circulations depend on the right ventricle. Oxygenated pulmonary venous blood returns to the left atrium, and because of the significant left ventricular inflow obstruction and decreased compliance, an obligatory left-to-right shunt is present at the atrial level through a patent foramen ovale or ASD. In the right atrium, the oxygenated pulmonary venous blood mixes with deoxygenated systemic venous blood and flows into the right ventricle. Blood is pumped to the pulmonary artery, with systemic blood then flowing from right to left through the PDA. The brachiocephalic vessels and coronary arteries are perfused through retrograde flow from the PDA into the arch and ascending aorta. The descending aorta is perfused from antegrade flow through the PDA.
Cyanosis and tachypnea generally are apparent within hours to 2 days after birth. With the normal postnatal drop in pulmonary vascular resistance, pulmonary blood flow increases and systemic blood flow decreases, leading to respiratory distress and poor systemic perfusion. As the PDA constricts, perfusion of the ductal-dependent systemic and coronary circulations further declines, with resulting myocardial ischemia, shock, and death. In the setting of poor arteriovenous mixing as a result of inadequate interatrial communication, shock and death may occur almost immediately after birth without intervention.
HLHS is readily identified in utero by the obstetric ultrasound four-chamber cardiac view, with approximately 60% of cases diagnosed prenatally. Chest radiographic findings are variable. If the interatrial communication is unrestrictive, there is progressively increasing pulmonary overcirculation with increased vascularity and cardiomegaly after the first hours of life ( e-Fig. 73.2 ). With a restrictive atrial septum, the heart size may be normal with pulmonary venous congestion that may be misinterpreted as primary lung disease.

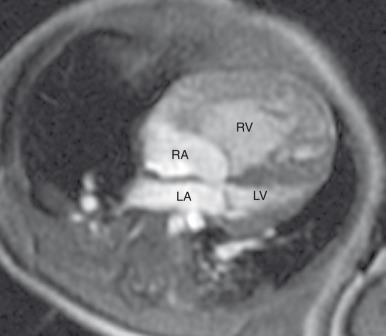
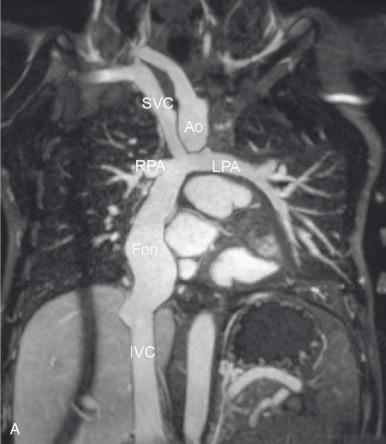
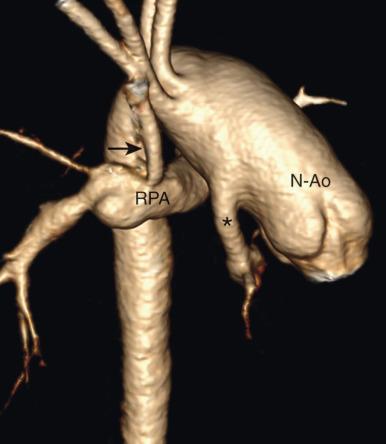
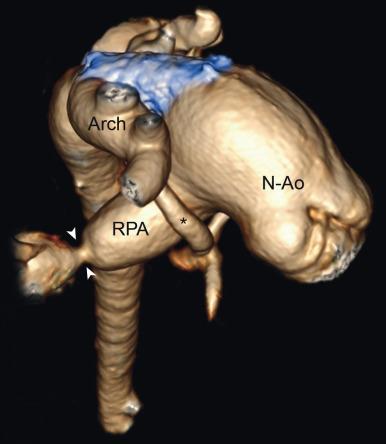
Echocardiography is the imaging method of choice and generally delineates all relevant presurgical anatomy. Cross-sectional imaging can be performed as an adjunct to echocardiography in complex cases. Magnetic resonance imaging (MRI) may be especially useful when the left ventricle is marginally hypoplastic and the possibility exists of a two-ventricle surgical repair, whether in the neonatal period or after initial single-ventricle palliation ( Fig. 73.3 and ). In these cases, MRI quantifies left ventricular volume, left versus right ventricular stroke volumes, and mitral versus tricuspid valve inflows to help plan the most appropriate surgical repair. MRI is also increasingly being used after the first stage of the palliative single ventricle surgery to quantify systemic right ventricular systolic function and tricuspid regurgitation and to evaluate for residual or recurrent coarctation and pulmonary artery stenosis or hypoplasia before the second-stage bidirectional cavopulmonary anastomosis. Less frequently, cardiac computed tomography angiography (CTA) may be used for preoperative vascular evaluation. After the third-stage Fontan completion procedure, MRI ( Fig. 73.4 ) is complementary to echocardiography, particularly in older patients with poor acoustic windows, and can improve risk stratification for transplant-free survival in this population.
Initial medical management includes intravenous prostaglandin E 1 (PGE 1 ) to maintain ductal patency. Ventilatory strategies and medications may be required to maintain adequate systemic perfusion and minimize pulmonary edema by optimizing the ratio of pulmonary to systemic blood flow.
Surgical treatment consists of a three-stage reconstruction procedure ( Fig. 73.5 ). The goal is to create in-series pulmonary and systemic circulations, with right ventricular support of the systemic circulation and passive flow through the pulmonary circulation. This allows for normal arterial oxygen saturation and decreases the volume load on the systemic right ventricle, but the reconstruction must be staged to account for the high neonatal pulmonary vascular resistance and subsequent decrease over the first year of life.
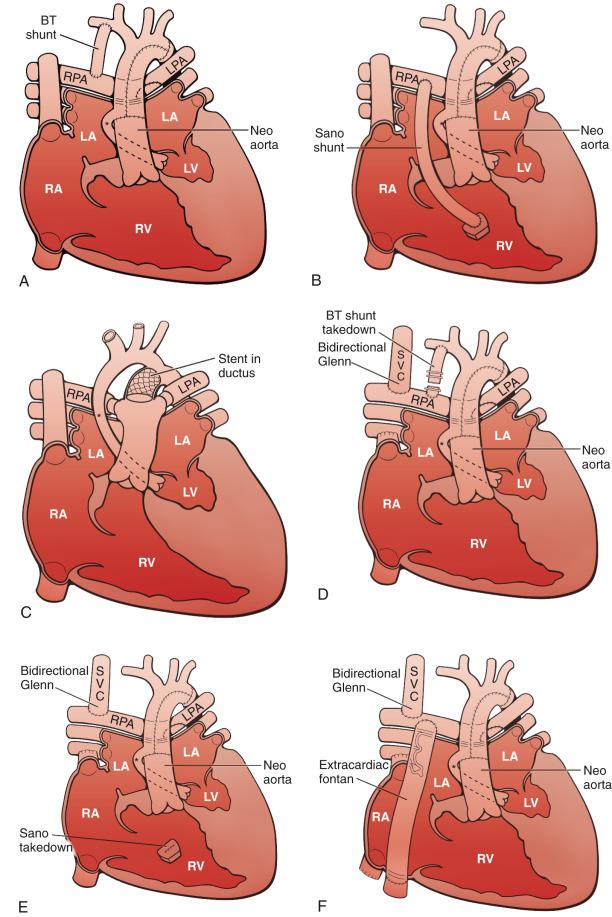
Stage I of the reconstruction—the Norwood procedure—often is performed in the first week of life. The goals of this procedure are to relieve any obstruction to atrial mixing, provide unobstructed systemic and coronary blood flow, and create a stable but restrictive source of pulmonary blood flow. A complete atrial septectomy is performed. The PDA is ligated, and the neo-aortic outflow is created by transecting the main pulmonary artery and anastomosing it to the hypoplastic ascending aorta (Damus-Kaye-Stansel anastomosis), with use of a homograft patch to augment the hypoplastic ascending aorta and aortic arch. Blood flow to the lungs is reestablished either via a right ventricle to pulmonary artery (RV-PA) conduit (Sano shunt) or via a modified Blalock-Taussig shunt (BT shunt) from the subclavian or brachiocephalic artery to the branch pulmonary arteries ( Fig. 73.6 ). If a BT shunt is used, there is diastolic runoff through the shunt that may lead to excessive pulmonary blood flow and “steal” from the coronary and systemic circulation. Conversely, the RV-PA conduit is associated with pulmonary regurgitation and potential right ventricular volume overload, a need for ventriculotomy and potential right ventricular dysfunction, and potential aneurysm formation or pulmonary artery distortion at the site of the conduit insertion.
By approximately 3 to 6 months of age, pulmonary vascular resistance has physiologically dropped, and stage II of the reconstruction—the bidirectional cavopulmonary anastomosis (Glenn) or hemi-Fontan procedure—is performed to redirect the upper body systemic venous return directly to the lungs. The superior vena cava (SVC) is anastomosed to the right pulmonary artery, and the SVC is either transected from the right atrium (Glenn procedure) or isolated from the right atrium with a patch (hemi-Fontan procedure). The BT shunt is divided or the RV-PA conduit is obliterated, and, if necessary, tricuspid valve repair and pulmonary artery angioplasty are performed.
As an alternative to the typical stage I and II procedures previously described, a “hybrid” approach may be undertaken to avoid cardiopulmonary bypass in the fragile neonatal period, particularly when mortality risk is high (e.g., low birth weight or cerebrovascular accident). The hybrid stage I procedure combines transcatheter ductus arteriosus stenting to provide systemic flow and surgical branch pulmonary artery banding to limit pulmonary blood flow ( e-Fig. 73.7 ). The comprehensive stage II procedure then must involve creation of the Damus-Kaye-Stansel anastomosis and reconstruction of the aortic arch, removal of the PDA stent and pulmonary artery bands, repair of the pulmonary arteries, atrial septectomy, and the Glenn or hemi-Fontan procedure.
Stage III of the reconstruction—the Fontan completion procedure—is generally performed at 18 to 36 months of age (see Fig. 73.4 ). Inferior vena cava blood flow is directed to the pulmonary arteries either via an extracardiac conduit or an intracardiac right atrial baffle (lateral tunnel). If the stage II procedure was a hemi-Fontan, the lateral tunnel is created and the SVC patch is removed. The Fontan procedure achieves complete separation of the systemic and pulmonary circulations. A fenestration may be left in the Fontan circuit as a “pop-off” into the heart if Fontan pressures are high, and this may lead to a more stable postoperative course. Many fenestrations close spontaneously, or they can be closed with a device at later cardiac catheterization.
Survival after the three-stage palliative procedure has improved steadily and now approaches 70%. The stage I Norwood procedure carries the highest mortality, ranging from 7% to 19%. Cardiac transplantation had been considered an alternative to staged Norwood palliation in the past, but because of limited donor availability and the recent improvement in survival after Norwood palliation, transplantation now generally is reserved for patients in whom staged palliation has failed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here