Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
6.1
6.2
6.3
6.4
Visit Expert Consult ( expertconsult.inkling.com ) for videos on topics discussed throughout the text.
In this chapter, we begin our discussion of the aging changes of the face. In particular, we deal with the functional changes that affect the vision. We are mainly interested in how the patient “sees” rather than how the patient “looks." I want to remind you that although we separate functional and cosmetic indications for a procedure, the distinction is artificial, based on reimbursement concepts. Patients do not easily separate the seeing and the looking parts of the results of the procedure you perform. In Chapter 7 we look at the aging changes of the face in more detail. We discuss procedures where the goal is improving how the patient looks more than how the patient sees. You should understand that the anatomy and principles of the aging process are the same.
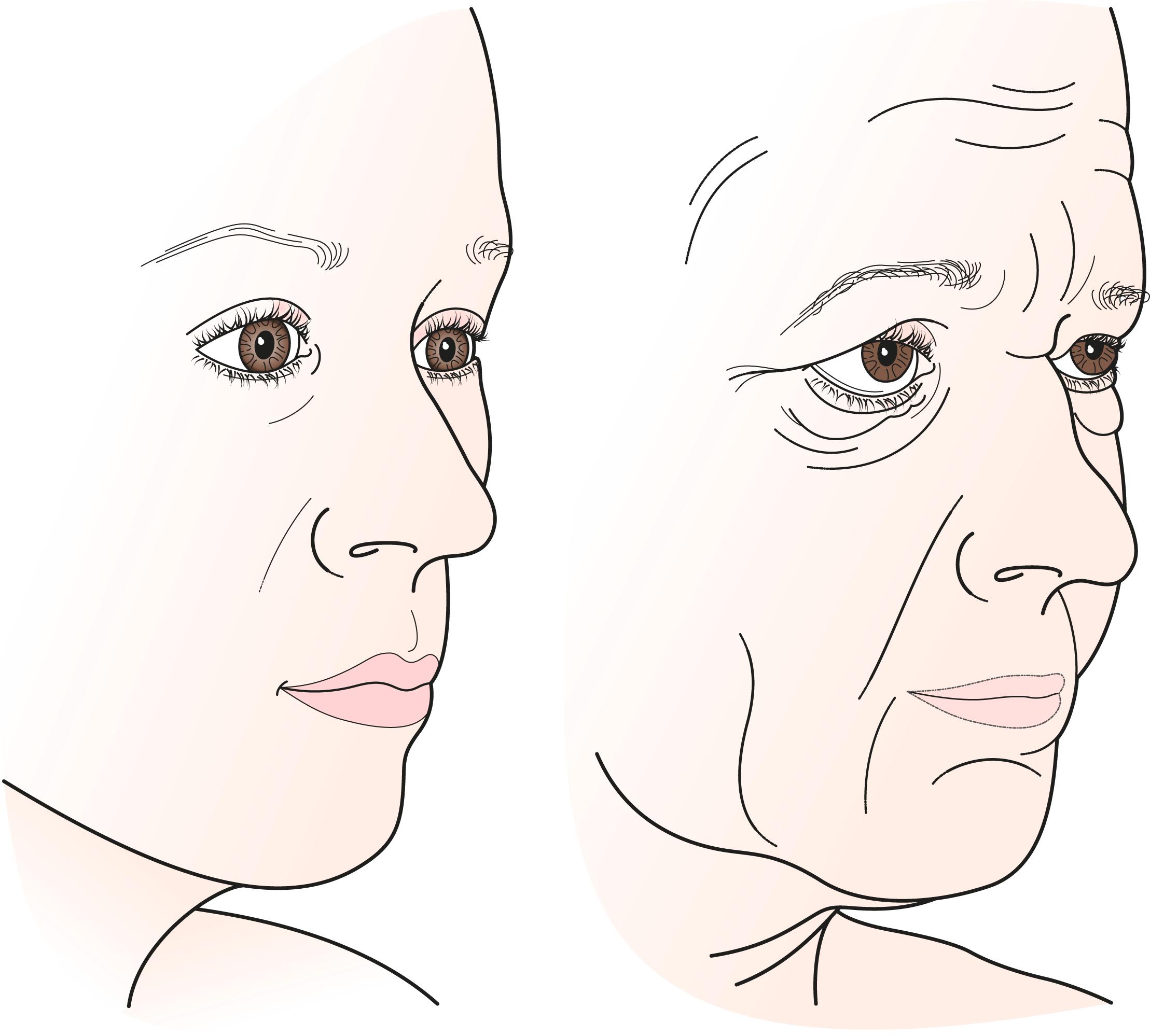
With time, the tissues in the periorbital area and face tend to sag and lose their youthful fullness. The periocular changes include a drooping of the eyebrow known as eyebrow ptosis , excessive accumulation of skin in the upper lid known as dermatochalasis , and a prolapse of orbital fat in the upper and lower lids caused by weakening of the fibrous orbital septum and orbital connective tissues. There is loss of the midface volume in the eyebrow and cheek fat pads. Characteristic changes in the lower face and neck occur, as well. These anatomic changes occur in all people to some degree as they age. More is offered on these changes in Chapter 7 . In some patients, family (genetic) traits may cause an exaggerated aging process. A common complaint is, “I’m starting to look like my mother (father).” In other patients, accidental or surgical trauma, sun exposure, or facial nerve palsy may add to the involutional process.
Let’s discuss some basic principles, or rules to live by, that apply to every patient interaction.
You must understand why the patient came to you.
What are the patient’s goals for the medical service that you are providing?
What are the patient’s expectations of the doctor–patient relationship?
You must to able to meet the patient’s goals.
Technically: The patient wants a correct diagnosis and correct treatment.
Emotionally: The patient needs to feel cared for.
All patients are the same, but each is different.
You need to individualize the care of each patient.
Always underpromise and overdeliver.
If you follow these rules, you have happy patients and a happy practice. If for some reason you feel that you are not in sync with a certain patient, it may be better to work a little more to get there before you proceed with an operation. If you find that you cannot follow these rules with that patient, it may be best to refer the patient to another doctor. For many years, I thought that I could and should be able to take care of every patient that came to see me. As I have gotten older, and maybe wiser, I have learned that this is not the case. I want you to have happy patients and a happy practice.
Regarding functional eyelid surgery, let’s apply these principles. In each case, you must seek out and understand the patient ’ s complaint regarding these changes . Many patients complain about decreased vision due to the sagging tissues around the eye. Other patients may be more concerned about their appearance . One of the most important parts of the history-taking process is to understand the patient’s complaint so that the appropriate concerns are addressed during surgery. In this chapter, the functional changes of the periocular region (those changes that affect the vision) are discussed. In Chapter 7 , the aesthetic changes of the eyelids and face are discussed. There is a big overlap between the two approaches. Patients with functional changes have aesthetic issues, and vice versa. I try to discuss the patient’s problems using statements such as
Are you concerned about how you see?
Are you concerned about how you look?
Part of your job is to sort out the relative importance of these complaints. In general, the patients with aesthetic concerns are more demanding and require more of your time. Your reimbursement for treatment to improve how the patient looks is higher than for treatment to improve how the patient sees. In many cases, the technical part of the operations is very similar, but the patient’s goals may be different. Be sure that you understand the patient’s goals. Equally important, make sure that the patient knows your goals. If your goal is a functional improvement, make sure that the patient understands that the purpose of the procedure is not to improve his or her looks. Your efforts to clarify the see-better versus look-better goals can help to avoid potential patient dissatisfaction. Should your patient have a particular look-better goal in mind, you may be able to offer that at as an out-of-pocket cosmetic procedure for the patient. This can be a tricky area. Over time, you develop your own style of discussion and learn to apply it to each individual patient.
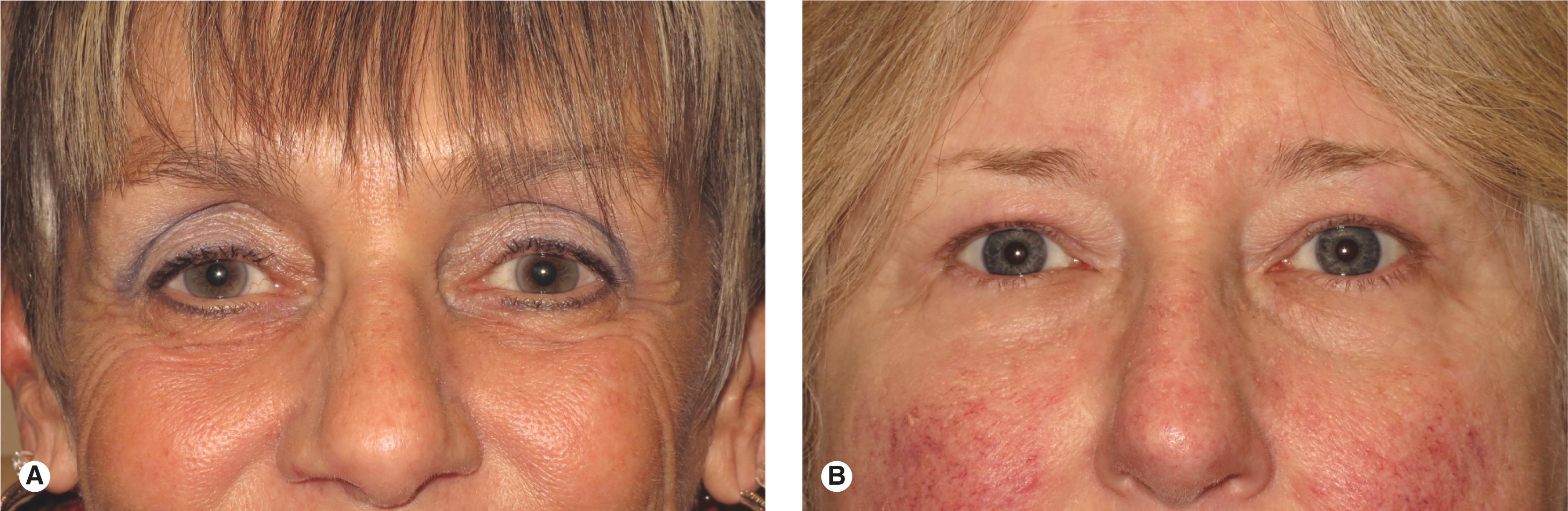
A detailed examination identifies the specific anatomic abnormalities that need to be addressed during surgery. These abnormalities include (1) low eyebrow position; (2) abnormal eyebrow contour, especially temporal droop; (3) redundant eyelid skin and muscle; (4) prolapsing orbital fat; (5) upper eyelid ptosis; (6) lower lid retraction; (7) lower eyelid laxity; (8) horizontal narrowing of the fissures, or phimosis; and (9) abnormal orbital bony architecture. Midface, lower face, and neck changes should be identified, as well. Once these individual factors are identified, their specific relationships to one another need to be determined ( Figure 6.1 ).
An operation is planned to correct the functional or aesthetic anatomic abnormality identified. Functional operations include browplasty and upper blepharoplasty . A variety of other procedures is available to complete the rejuvenation of the entire face, including operations on the lower eyelids, forehead, midface, face, and neck. We discuss these procedures in Chapter 7 . Neuromodulator injections (Botox, Dysport, and others) minimize wrinkles and shape facial features. A variety of fillers is used to add volume to the aging face. A full face is a young face. Fillers help to smooth the transitions from one area of the face to another, a primary feature of youth. You may also want to learn laser resurfacing and chemical peeling to improve wrinkles and variations in skin color and texture.
The procedures that make your patient see better are covered in this chapter. Here, we discuss the principles of upper blepharoplasty from a reconstructive point of view. Although this procedure is in principle the same for reconstructive and aesthetic purposes, there may be individual differences depending on the patient’s goals. Some of these nuances are presented. If I have not said this enough, each surgery should be directed at fulfilling the patient’s goals, whether the goal is functional or cosmetic, or both. As usual, during every operation you want to avoid complications of surgery, including asymmetry, dry eye, lower lid retraction, and postoperative hemorrhage.
Let’s discuss the anatomy of the eyelids and eyebrow. You should use this information as you examine your patient in preparation for either a functional or an aesthetic procedure. We have covered much of this in previous chapters, so I hope that some of this information is a review. Keep in mind the principles; you can always go back and learn the details. In this chapter, I introduce some information related to the aging changes of the face and also discuss upper blepharoplasty and eyebrow ptosis operations for functional improvement. The principles apply equally to cosmetic procedures of the face. In Chapter 7 , we focus on lower blepharoplasty, cheek lift, aesthetic eyebrow procedures, fillers, neuroparalytic agents, and an overview of the facelift operation.
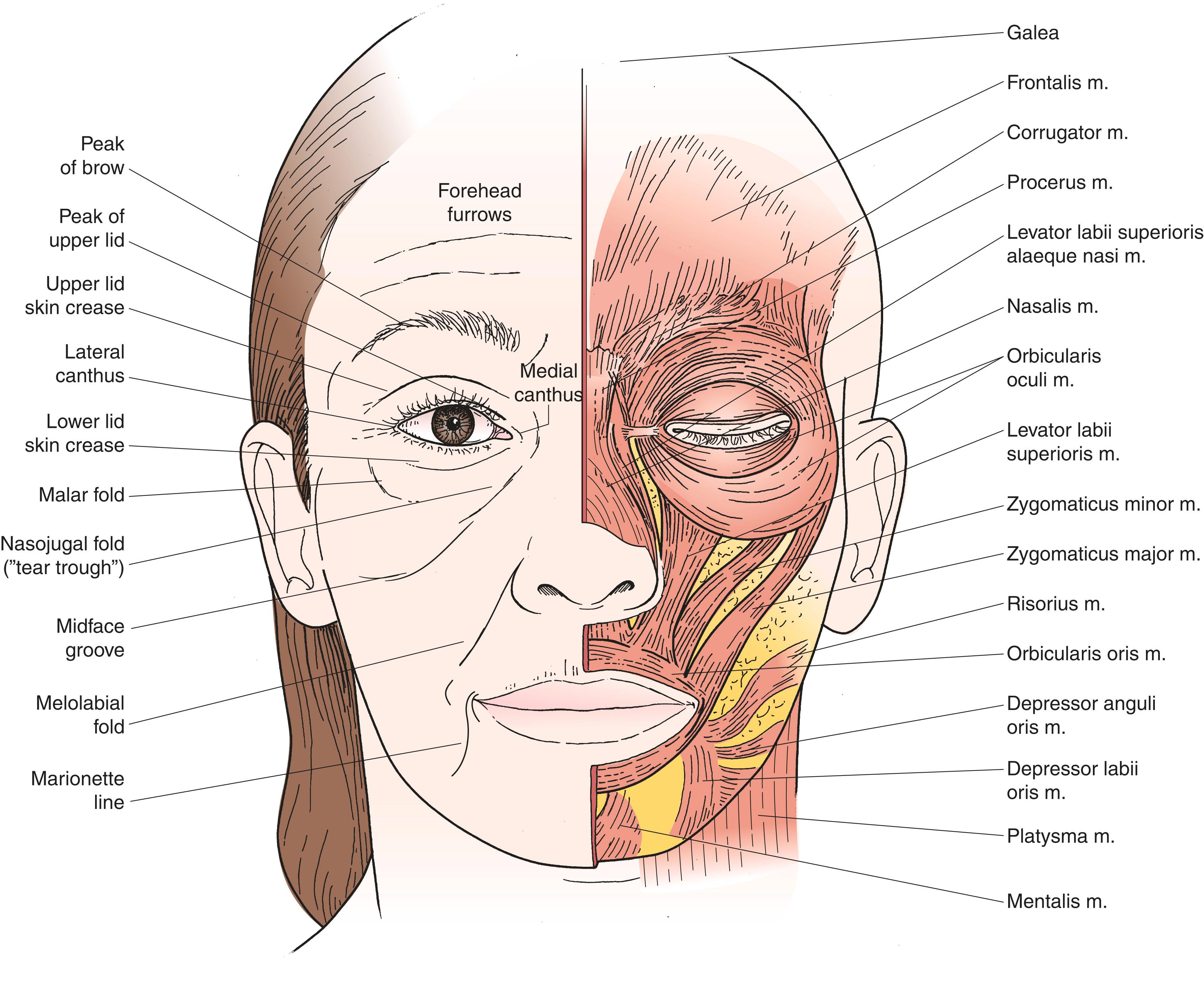
The eyebrow has three parts, the head , body , and tail . The direction of the eyebrow hairs varies from upward in the head of the eyebrow to horizontal and slightly downward in the tail of the eyebrow. The eyebrow is part of the forehead with similar thick skin and abundant sebaceous glands. The thick skin of the eyebrow blends in with the thinner upper eyelid skin of the skin fold ( Figure 6.2 ). You can see and feel this transition.
The male and female brows differ considerably in position and shape. The male eyebrow is lower than the female eyebrow , resting at the edge of the superior orbital rim. The female eyebrow is higher, especially in its temporal aspect, and sits above the orbital rim. The female eyebrow tends to be somewhat thinner and is frequently manicured to emphasize a temporal arch, with the highest point generally occurring at the junction of the body and tail of the eyebrow (see Figure 2.4 ).
Although we take these gender differences for granted, they are part of our culture, in which a youthful appearance is emphasized. Like other secondary sexual characteristics, the eyebrow position and contour send subtle clues regarding youth and reproductive ability. The thick low male eyebrow is considered a sign of virility. The high arched eyebrow of a woman is a sign of youth and vitality, which diminishes over time, seen as a temporal eyebrow ptosis.
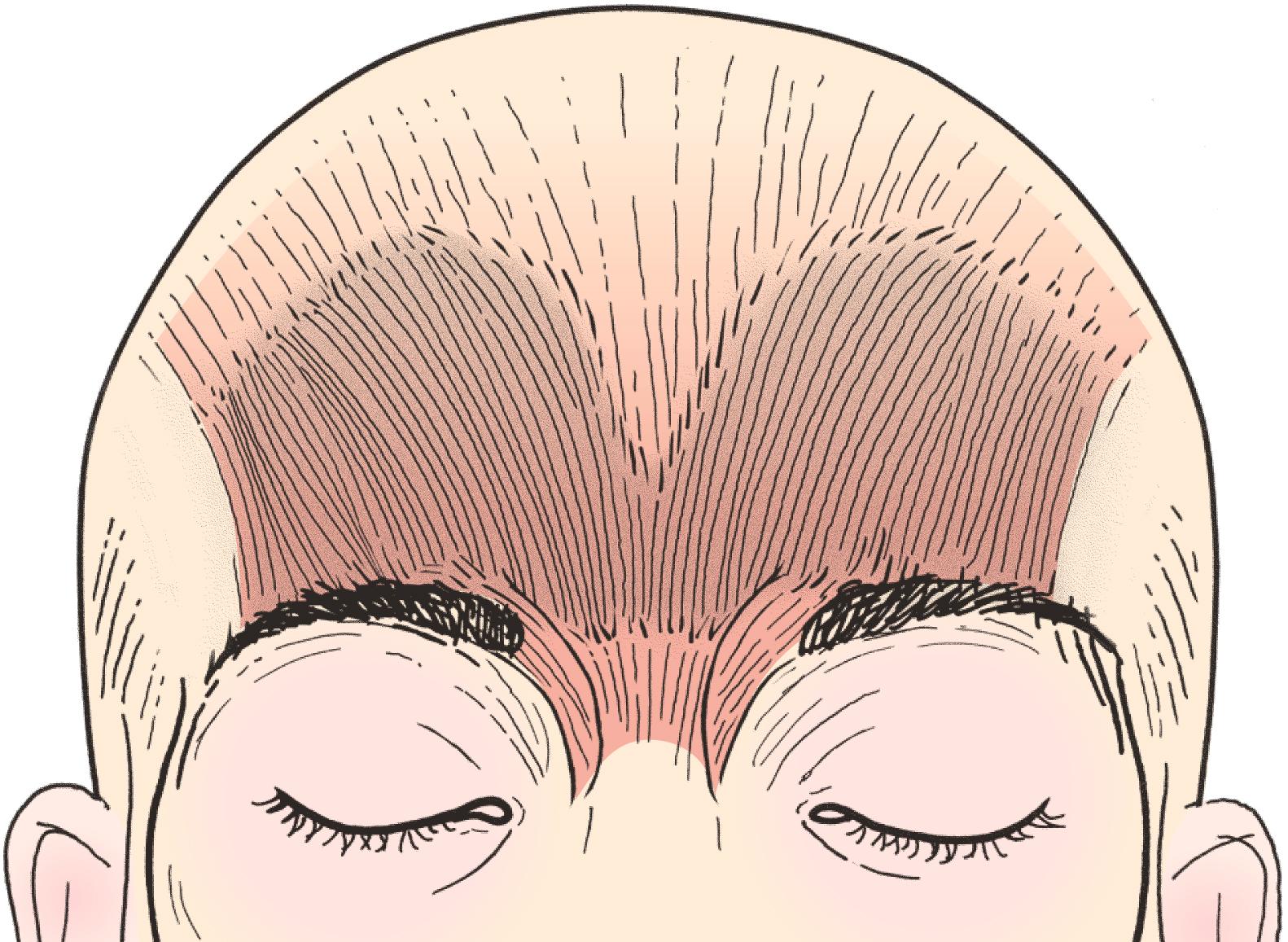
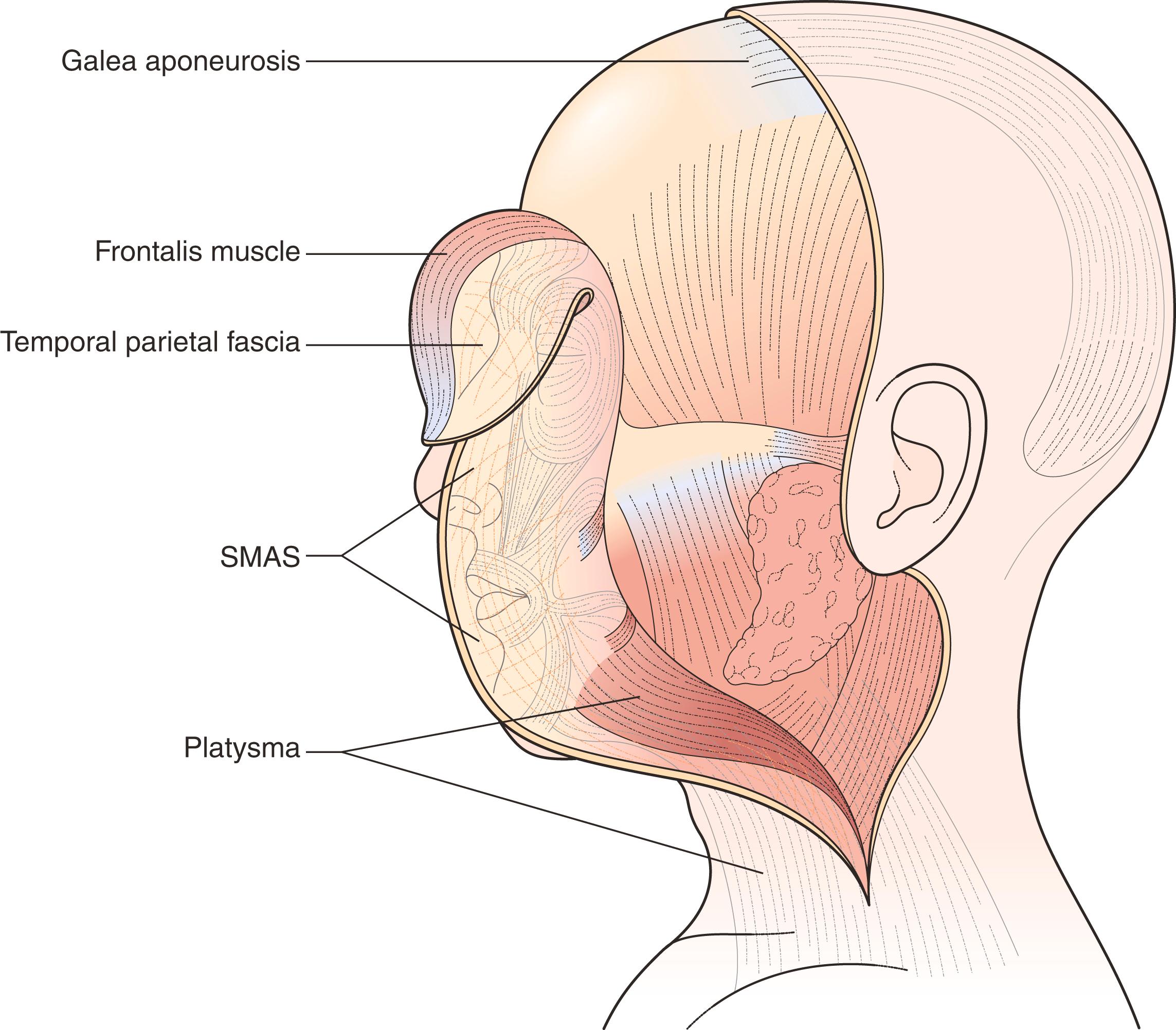
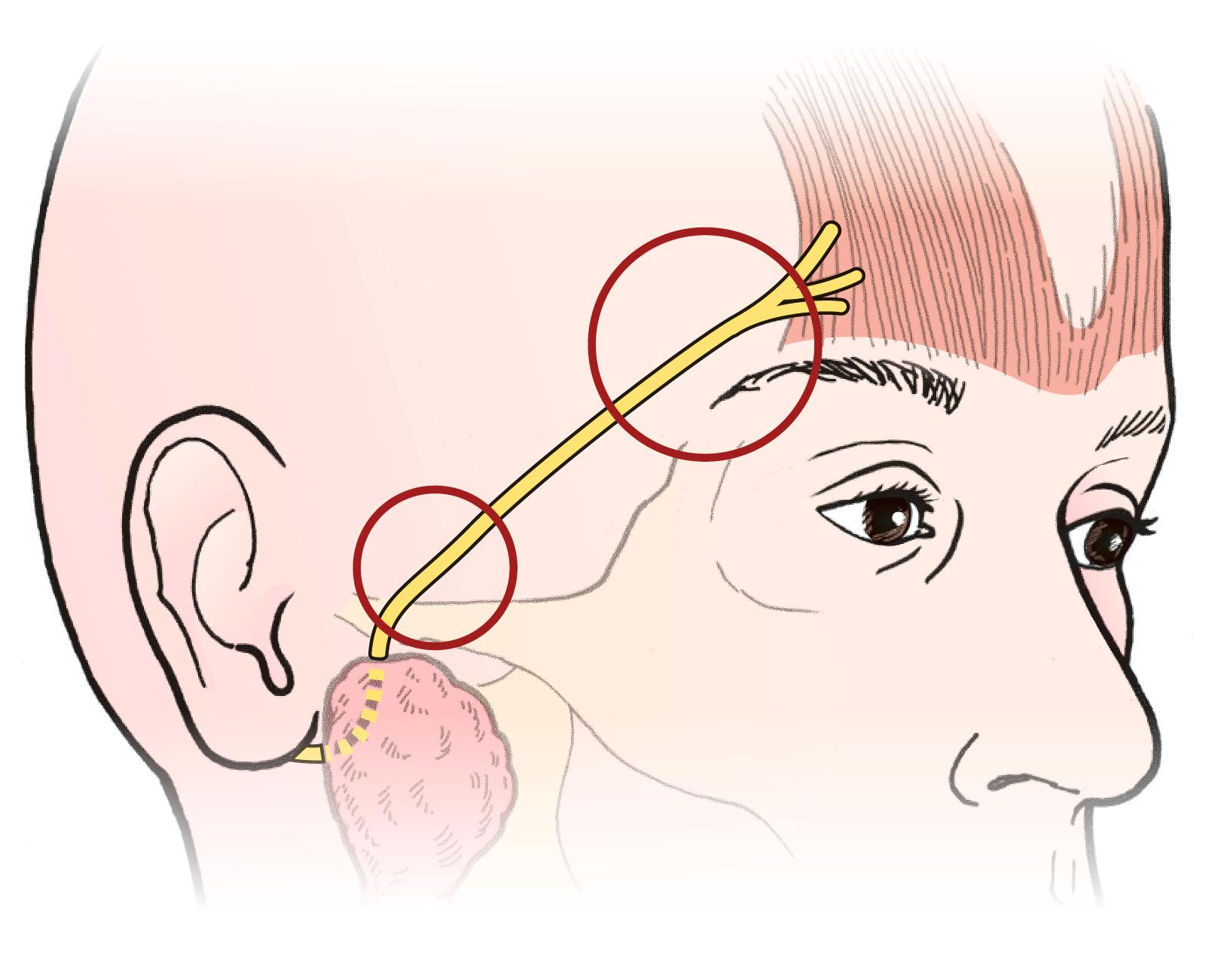
The normal eyebrow moves independently of the upper lid. Extreme elevation of the eyebrow, as seen with severe upper lid ptosis, causes only slight elevation of the eyelid. The elevator of the eyebrow is the frontalis muscle ( Figure 6.3 ), which extends from the eyebrow over the forehead to merge with the broad fibrous tissue of the galea aponeurotica. Elevation of the frontalis muscle causes the horizontal furrows frequently seen in the forehead. Innervation of the frontalis muscle, like that of other muscles of facial expression, comes from a branch of the facial nerve , the temporal branch (also known as the frontal branch of the facial nerve ). This single nerve branch provides innervation to the eyebrow on the same side. The approximate position of the temporal nerve can be estimated by drawing a line from the tragus of the ear to 1 cm above the tail of the eyebrow (see Figure 2.32 ).
Surgery in the path of the temporal branch of the facial nerve should be undertaken with caution to avoid damage to this nerve. Because this single nerve branch causes elevation of the eyebrow, inadvertent injury to the eyebrow may cause a prolonged paresis or permanent paralysis of the eyebrow.
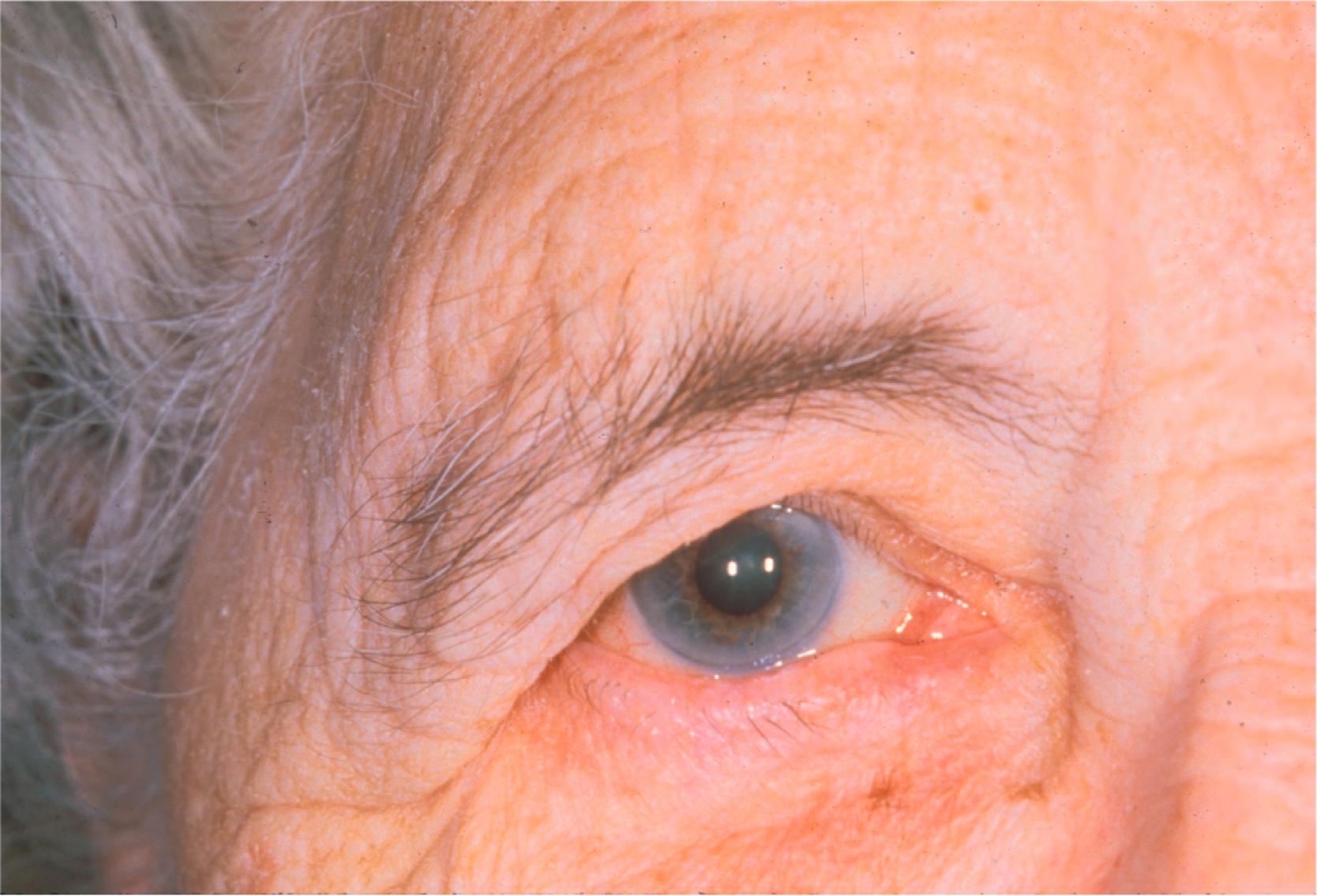
The width of the frontalis muscle stops short of the tail of the eyebrow. Consequently, elevation of the temporal eyebrow often becomes deficient with aging, causing a temporal eyebrow droop ( Figure 6.4 ). As the eyebrow droops, the upper lid skin fold is pushed down, accentuating the upper lid fold, often misinterpreted as redundant skin. Look for this problem in your older patients. It is so common that you may be ignoring it. You should contemplate eyebrow repositioning (browplasty) in every older patient for whom you are recommending a blepharoplasty. More is said about this later.
The eyebrow as an anatomic unit starts where the thin eyelid skin stops, not where the eyebrow hairs begin. Remember that a well-supported eyebrow rests on or above the superior orbital rim. The underlying fat, the retroorbicularis oculi fat (ROOF), should cushion the superior orbital rim. This temporal support and fullness of the brow is a sign of youth.
As you get more experience, you pay attention to the orientation of the eyebrow hair follicles. As you move from medial to lateral, the brow hairs change orientation from more vertical to more horizontal. In the unmanicured brow, there is a peak of hairs at about the lateral third of the brow where the hair orientation changes. This can be a useful landmark for judging symmetry and marking the eyebrow before any eyebrow surgery.
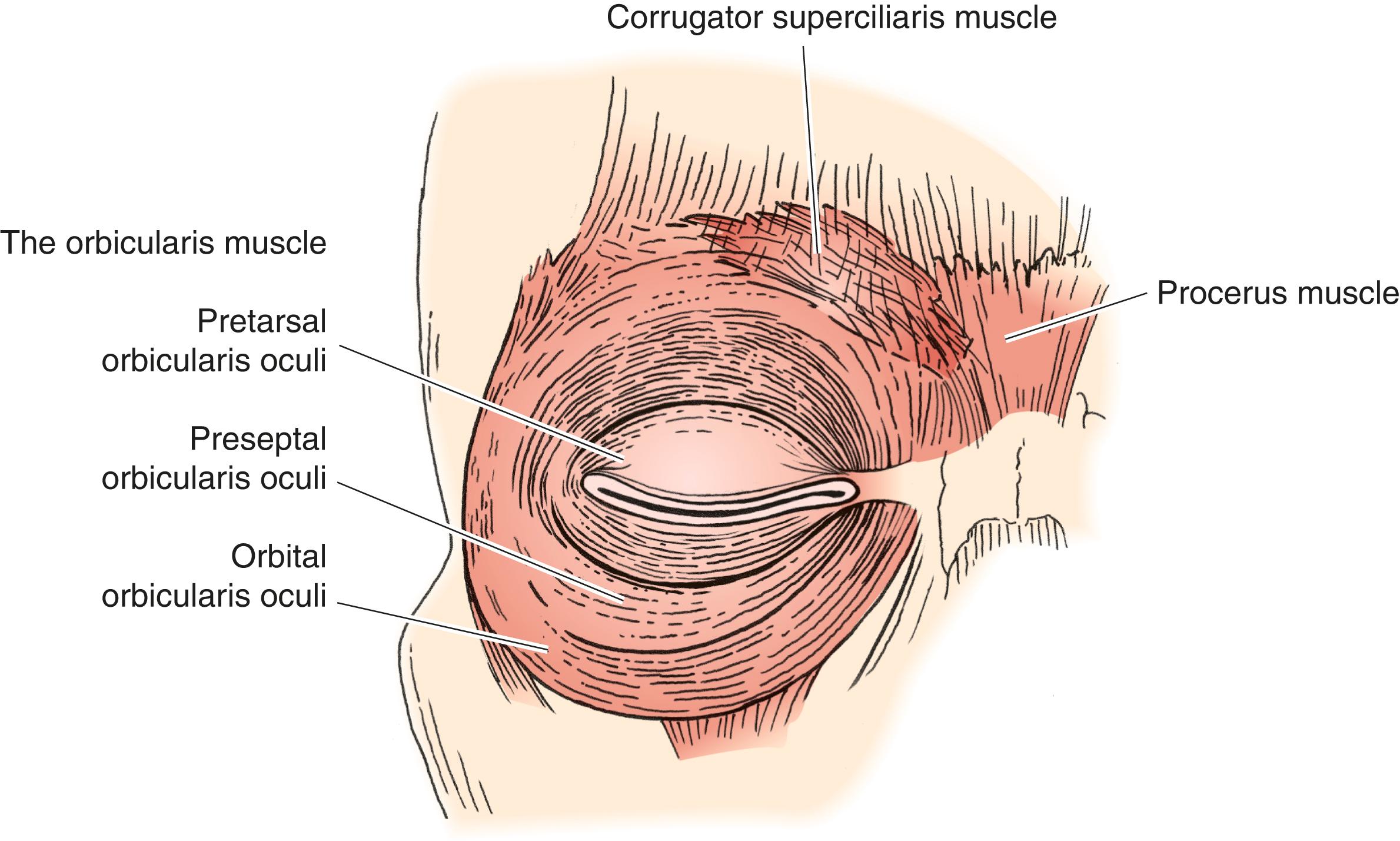
The protractors , or depressors , of the eyebrow are the orbital orbicularis, procerus, and corrugator muscles ( Figure 6.5 ). Contraction of the orbicularis muscle closes the eye and pulls the eyebrow down. The vertical fibers of the procerus muscle at the head of the eyebrow are responsible for the horizontal furrows in the glabella. The C-shaped corrugator muscle pulls the head of the eyebrow medially and downward, causing the vertical glabellar wrinkles . Wrinkles in the area of the glabella are a common cosmetic concern among women. In many cases, these wrinkles may give an anguished or angry look to the face (see Figure 2.17 ).
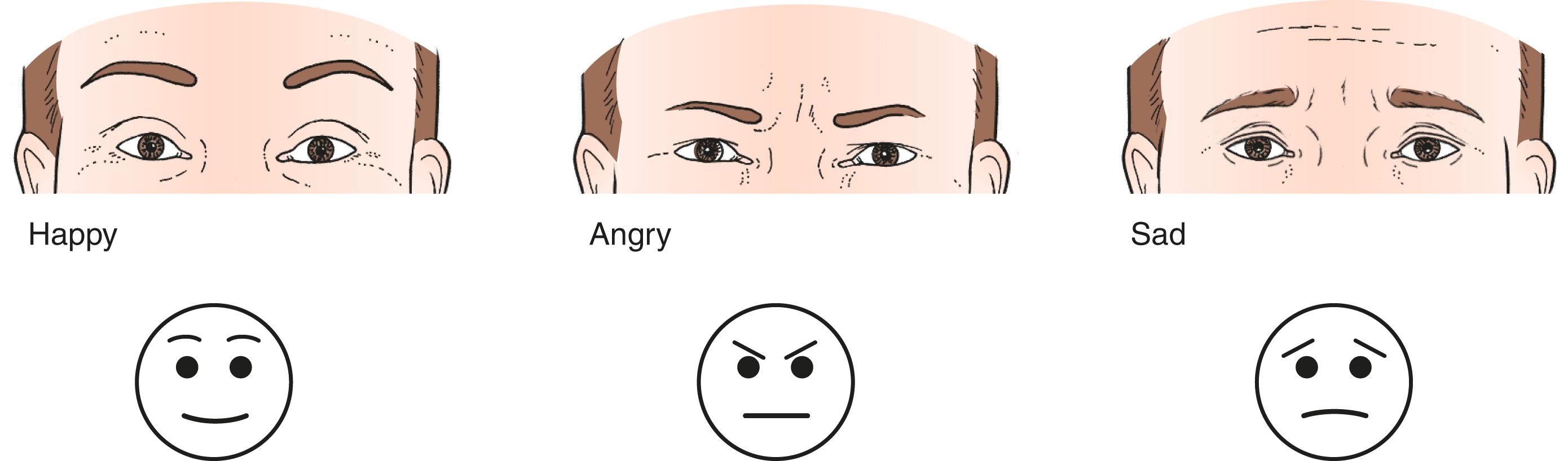
The muscles of the eyebrows are among the most important muscles of facial expression. They are strong indicators of mood and feeling. This is best demonstrated by a simple diagram of the familiar happy face ( Figure 6.6 ). A downward slope to the medial aspect of the eyebrows with associated glabellar wrinkles tends to convey anger . A drooping of the temporal eyebrow suggests melancholy . Arched, normally contoured eyebrows indicate happiness . Elevation of the arched eyebrow with associated forehead furrows tends to indicate surprise . You may have seen this diagram in other texts. It is a very useful concept. You will apply this concept in using Botox or browplasty procedures to minimize glabellar lines and change the shape of the eyebrows.
There are many operations that raise the eyebrows. Compare the extremes—a temporal direct eyebrow lift and a coronal forehead lift—the former lifting the lateral part of the eyebrow and the latter lifting the eyebrows and entire forehead. The temporal lift uses a short incision placed at the lateral third of the eyebrow hairs. It corrects the temporal sag and helps to clear the field of vision. It does nothing for the medial eyebrow or the glabella. The coronal forehead lift is performed through an incision across the top of the head from ear to ear. The entire forehead and eyebrows are raised. In addition, the glabellar folds, forehead furrows, and redundancy of the eyelid skin under the medial eyebrow are all improved. The overall result of the coronal lift is more aesthetically pleasing. Most forehead lifts are done for cosmetic improvement and are self-pay procedures. The operating time and recovery time for the two procedures are much different than for the simpler browplasties. Although there is a long scar at the hairline (pretrichial forehead lift) or in the hair (coronal forehead lift), it is less visible than the shorter scar over the eyebrow from a direct browplasty incision. However, the top of the head is left with some degree of numbness. You learn which procedure is the best choice for your patient. I have somewhat arbitrarily divided these procedures into functional eyebrow lifting procedures and cosmetic forehead lifting procedures and discuss them in separate chapters.
The proportions of the normal face are divided into thirds : the upper third from the hairline to the pupil; the middle third from the pupil to the alae of the nose (the midface), and the lower third from the nose to the chin. These thirds occur in roughly equal portions in a well-balanced face. Your patient’s facial proportions may have been less than perfect since youth or may have changed over time. Changes in the male forehead associated with aging and male pattern baldness affect the proportions of the face. A woman’s hairline may thin with age. In a general sense, a person with a high forehead is assumed to be somewhat more intellectual; hence, the term highbrow. Lower hairlines, on the other hand, are associated with lower intelligence (the caveman or Cro-Magnon look). A forehead that is too high or too low is generally considered less aesthetically pleasing ( Figure 6.7 ). The height of your patient’s forehead is changed by the type of operation that you perform. Incisions placed between the eyebrow and the hairline shorten the forehead. Incisions placed in the hair elevate the hairline, increasing the length of the forehead. These factors may contribute to the choice of incision placement in the patient’s forehead. More is said later about rejuvenation operations that lift the upper, lower, and midface. More is learned about the aesthetic proportions of the face. This is a simple but important concept that guides many of your aesthetic decisions. The rule of thirds discussed is a simplification of the golden ratio , a principle used in many design applications (check out www.goldennumber.net/beauty and www.phimatrix.com/design-composition-golden-ratio for more information).

The upper eyelid consists of three parts:
Upper lid skin fold
Upper lid sulcus
Pretarsal eyelid
The skin and muscle between the eyebrow and the lid crease form the upper lid skin fold (see Figure 6.2 ). To have normal movement of the eyelid, there needs to be some redundancy in the eyelid tissues. The redundancy of the skin fold allows this movement. The eyebrow above and the skin crease below bound the skin fold.
The upper lid skin crease is formed by attachments of the levator aponeurosis extending through the orbicularis into the skin. As the levator contracts, the skin crease is pulled upward, creating or deepening the superior sulcus . The upper lid skin crease is slightly higher in women than in men. A man’s skin crease is usually at 6 to 8 mm, whereas a woman’s skin crease is usually between 8 and 10 mm above the lid margin. This varies among individuals. As the patient ages, the pretarsal skin sags somewhat and the upper lid skin crease may change. The natural skin crease position can be estimated in a simple procedure performed before marking for blepharoplasty. Elevate the eyebrow and give the patient a target. As you elevate the target, the upper eyelid skin tucks into place. This is the line of the original natural skin crease. In general, this position corresponds to the height of the upper eyelid tarsus. If you are uncertain where to place the crease, evert the eyelid and measure the tarsal height with a caliper. Use this number as the eyelid crease height. As you gain experience with upper blepharoplasty patients, you may want to lower the crease mark by a millimeter or so. Excising tissue above the crease tends to pull the crease superiorly. This creates tightening of the saggy pretarsal skin but also tends to raise the crease somewhat. A common error by many blepharoplasty surgeons, in my opinion, is to place the upper eyelid crease incision too high, which tends to age the eyelid by deepening the superior sulcus. Later, we talk about the option of placing skin crease–forming sutures to make sure that the eyelid crease stays at the correct location.
A complex interaction of anatomic factors affects the fullness of the skin fold and the depth of the sulcus. Younger patients tend to have a full, but not excessive, skin fold supported by a full eyebrow. The youthful eyebrow is at or above the superior rim. A full fat pad posterior to the eyebrow softens and shapes the eyebrow. The contour of the bony temporal rim is visible. There is prolapse of orbital fat into the fold. The skin is supple without loss of elasticity or the addition of a crepelike texture. The levator muscle pulls the pretarsal portion of the lid into the orbit, under the skin fold. In children, the skin fold appears to blend into the eyebrow. As the bony forehead develops in children and young adults, the fold lifts and remains tight against the eyebrow, and varying degrees of superior sulcus develop. With age, the eyebrow descends and the orbital fat prolapses, tending to cover the sulcus of the older adult ( Figure 6.8 ). Do not be fooled, however; many young adults never had a deep sulcus or much pretarsal skin visible. You may want to reread this. These are important concepts if you want to attain any level of sophistication in performing blepharoplasty.
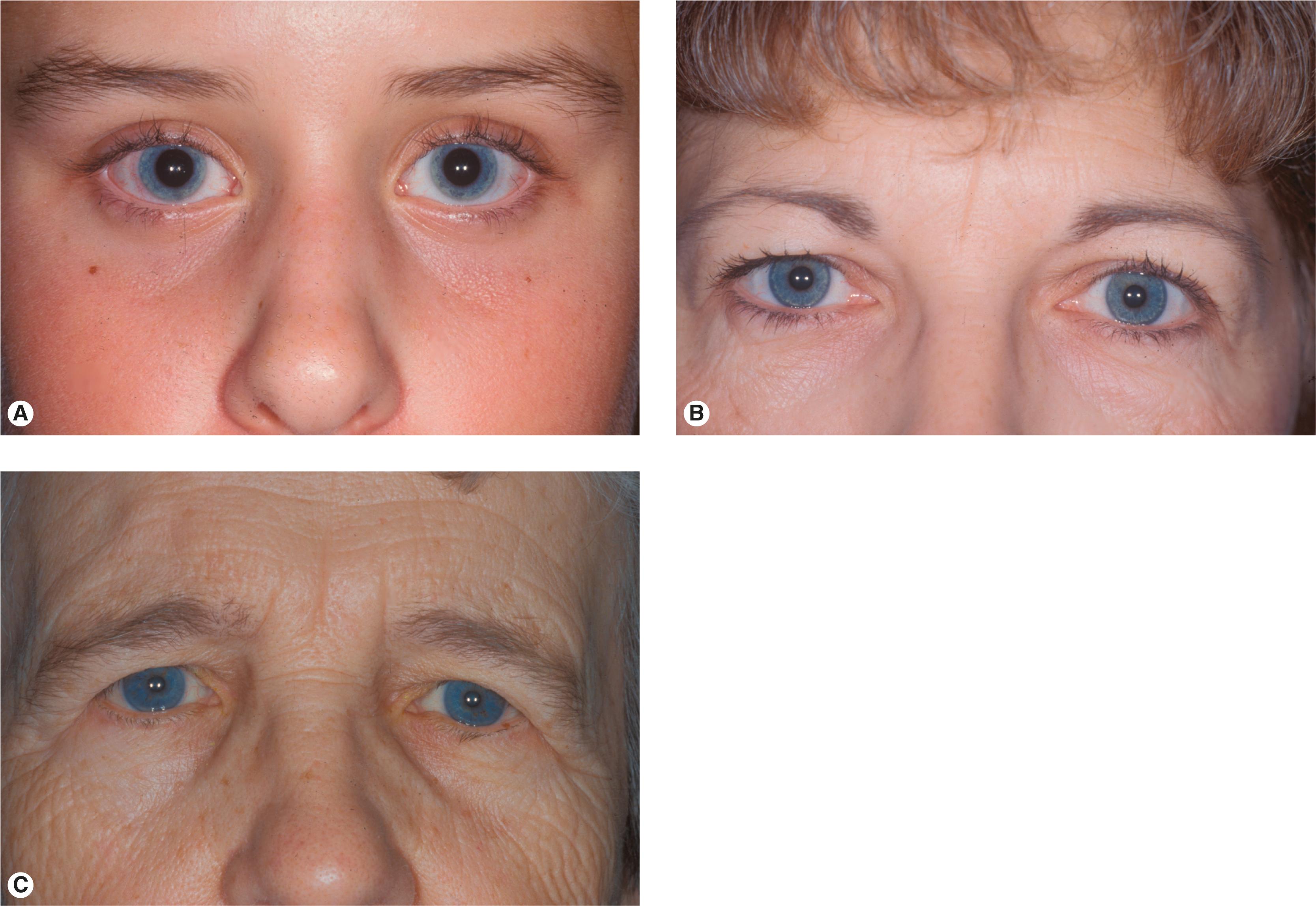
Individual facial proportions and bony features greatly influence the size of the skin fold ( Figure 6.9 ). Some patients with a high or prominent eyebrow always have a minimal skin fold with a deep superior sulcus. Other patients with a flat eyebrow have a full skin fold and shallow sulcus even as children. It is important to recognize these anatomic features because browplasty and blepharoplasty do not give the same results for each patient. Ask your preoperative blepharoplasty patients to bring in photos of themselves as a teen or young adult. Often a wedding photo is available. The variety of normal youthful skin folds, superior sulci, and eyebrow positions is surprising. This is a helpful, and often revealing, exercise for both you and your patient! Evaluating these features helps to create a reasonable expectation of rejuvenating surgery. Many of your female patients had never had the high arched eyebrow or deep sulcus that you are trying to achieve.
The discussion of the transition from the lower eyelid to the cheek is extensive. This contemporary thinking is just starting to extend to the eyebrow and upper eyelid but is equally important if rejuvenation is the goal. In the past, emphasis has been on the eyebrow position and height. The fullness of the eyebrow and its contour play an important role in creating a smooth youthful transition from the eyelid to the forehead, more so than does the height of the eyebrow alone.
The upper eyelid skin is the thinnest skin of the body, allowing free movement of the eyelid. The eyelid skin is much thinner than the eyebrow skin above. The eyelid skin is often somewhat more pigmented than the surrounding facial skin (part of the reason that many patients complain about dark circles under the eyes). Looking at a few of your next patients delivers this point home to you. Look for the junction of the eyebrow skin and the eyelid skin; there is a difference in color, texture, and thickness ( Figure 6.10 ). This becomes important in judging if you need to lift the eyebrow when also performing a blepharoplasty. I reinforce this necessity several times in this and the next chapter.

The muscle underlying the eyelid skin is the orbicularis muscle. You are familiar with the three portions of the orbicularis muscle: the orbital, preseptal, and pretarsal portions. The orbital orbicularis muscle interdigitates with the procerus, corrugator, and frontalis muscles at the glabellar region (see Figure 6.5 ).
Relaxation of the frontalis muscle causes the eyebrow (and underlying orbital orbicularis muscle) to fall. Correction of eyebrow ptosis repositions the eyebrow and orbital orbicularis muscle at the rim. Upper lid blepharoplasty removes a portion of the preseptal skin and, often, the underlying orbicularis muscle. This reduces the skin fold and tightens the pretarsal orbicularis muscle and skin. Preserving the fullness of the sulcus and eyebrow fat is important, as has been discussed above. In the past, a significant amount of orbital fat was removed from the eyelid. Currently, most surgeons retain almost all the fat in the upper eyelid, removing only obviously prolapsed medial fat.
The wrinkle lines in the lateral canthus, or crow’s feet, arise from contraction of the orbital orbicularis muscle. As was discussed in Chapter 2 , wrinkle lines form perpendicular to the underlying muscle fibers (circularly oriented fibers make radial lines).
The orbital septum lies directly beneath the orbicularis muscle. It is a fibrous layer arising from the periosteum of the orbital rims. The septum functions as an anatomic boundary of the lids, separating the eyelids from the orbit ( Figure 6.11 ). Although this fibrous tissue is quite tough, it also allows for vertical movement of the eyelid. With aging, weakening of the orbital septum allows fat to prolapse forward into the eyelid. When no fat prolapse is present, the orbital septum is not opened during upper lid blepharoplasty. When orbital fat prolapse is present, the orbital septum may be opened, and a small amount fat can be excised or repositioned. In the lower eyelid, fat prolapse is the main indication for blepharoplasty. Because the septum is not elastic, once it has been opened it is not sewn closed. Inadvertently sewing the septum into the eyelid closure can contribute to lagophthalmos of the upper eyelid or retraction of the lower eyelid. Of course, rules are meant to be broken. In the lower eyelid, there may be times when you want to tighten the septum during lower eyelid blepharoplasty to prevent fat prolapse, especially of the lateral fat pad. This is an advanced lower blepharoplasty technique that you may want to try as you get more experienced, but for now, do not sew the septum closed!
The upper eyelid preaponeurotic fat is divided into two compartments, the preaponeurotic or central fat and the nasal or medial fat . The lacrimal gland fills in the temporal aspect of the preaponeurotic space in the upper lid ( Figure 6.12 ). The lacrimal gland is distinguished from the fat by its whitish color and lobulated surface. A branch of the palpebral artery runs posterior to the nasal fat pad. You should be careful not to inadvertently cut this artery because brisk bleeding ensues. The nasal fat pad is whiter in color than the central fat pad.
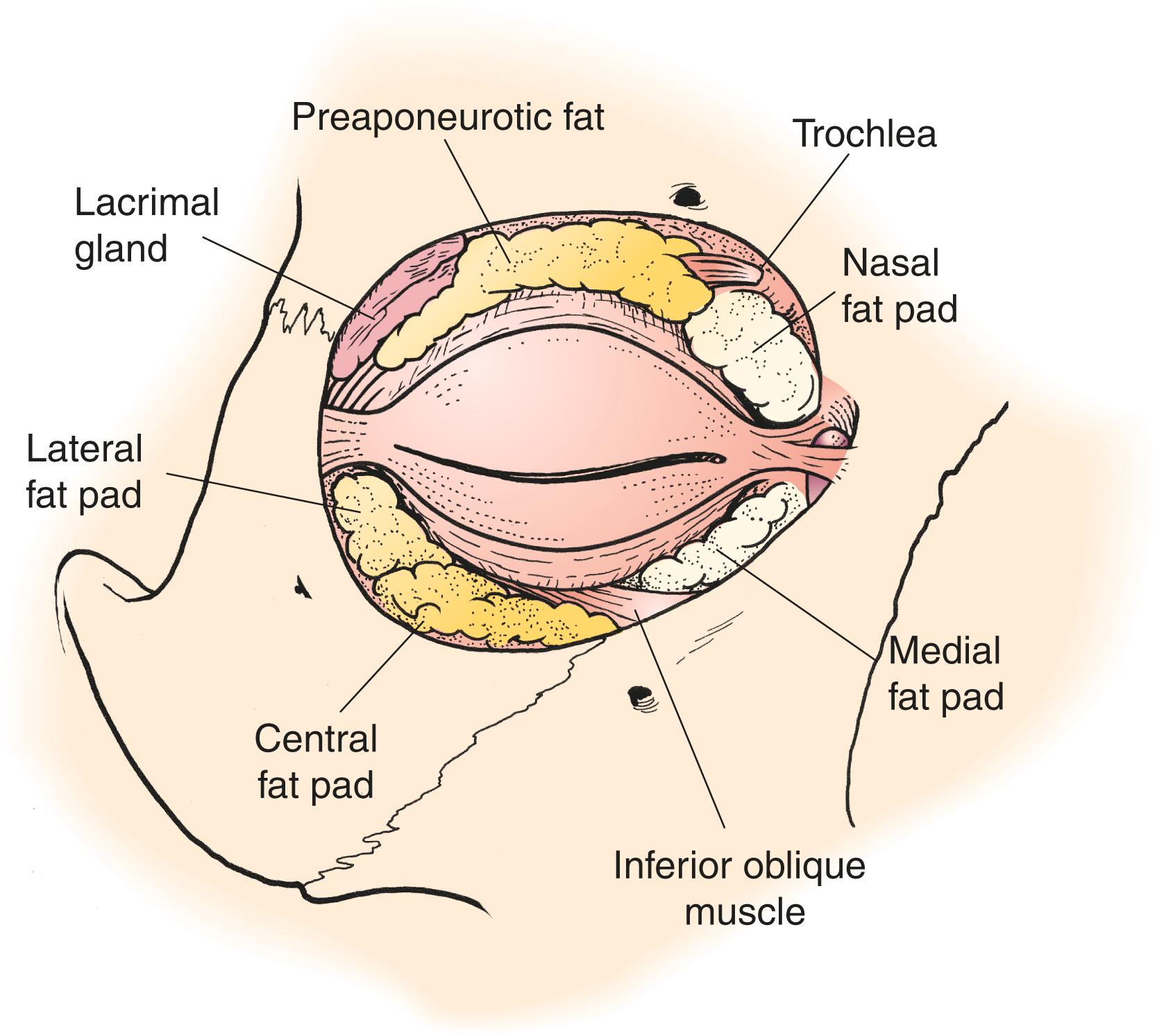
The amount and position of the fat prolapse varies from patient to patient. No fat prolapse is seen in many patients. These patients may have dermatochalasis only and do well with only skin and/or skin and muscle being removed during upper lid blepharoplasty. Nasal fat prolapse is especially common, but patients may have fat prolapse in any combination of locations ( Figure 6.13 ). Unless a very large amount of preaponeurotic fat is present, most blepharoplasty operations remove only a portion of the nasal fat pad. On occasion, you need to reposition a prolapsed lacrimal gland to reduce the fullness and improve the contour of the lateral skin fold.

Your examination of the upper and lower eyelids moves back and forth between the upper and lower eyelids constantly while you examine the face as a whole, also. Many of the aging changes of the lower eyelid affect function; ectropion, entropion, and poor lacrimal pump. In the next chapter, we look closely at the anatomic features of the lower eyelid that affect appearance. We leave the details of the lower eyelid examination until then.
Let’s do a quick review of the anatomy of this region in regard to eyebrow surgery. Consider two regions: medial to the temporal line and lateral to the temporal line . The temporal line is the anterior attachment of the temporalis muscle and the adjacent fascial layers to the skull. The forehead medial to the temporal line has the familiar SCALP layers ( s kin, sub c utaneous, a poneurosis, l oose areolar tissue, p eriosteum). The galea aponeurotica is the broad band of tissue that extends from the eyebrow to the occiput. The galea aponeurotic layer is the equivalent to the SMAS (superficial musculoaponeurotic system) in the forehead region of the scalp. Anteriorly, this layer consists of the frontalis muscle and its very thin anterior and posterior fascial layers. At the back of the head, the galea becomes the occipitalis muscle and its fascial layers. Remember how the SMAS in the face envelops and secures the facial muscles to one another. The galea aponeurotica does the same thing, connecting the frontalis muscle to the occipitalis muscle ( Figure 6.14 ). You can easily see the transition from the frontalis to the aponeurosis anteriorly by asking your patient to raise the brows strongly. You see where the horizontal furrows no longer form (see Figure 2.31 ). Also, recall the position of the corrugator and procerus muscles in the glabellar region. The arched C-shaped corrugator contraction creates the angled lines in the glabella and the vertically oriented procerus produces the horizontal lines of the glabella (see Figure 2.17 ). You can also see how these muscles and the orbicularis muscle essentially are part of the SMAS, although they are not strictly defined as such.
The temporal branch of the facial nerve provides the motor innervation of the frontalis muscle. This branch runs from the tragus to about a centimeter above the tail of the eyebrow ( Figure 6.15 ). The motor innervation to the frontalis muscle is from the posterior surface, as it is for most muscles innervated by the facial nerve. I usually draw a line showing the path of this branch of the nerve as a reminder to not be deep to the frontalis muscle at the tail of the eyebrow when doing a temporal direct browplasty. The line also reminds me that the most superficial position of the temporal branch is overlying the zygomatic arch. The sensory innervation to the forehead is from branches of the first division of the trigeminal nerve (V 1 branches, including the supraorbital, supratrochlear, and lacrimal branches). It is difficult to prevent some degree of hypesthesia when making incisions in the forehead.
In my mind, the main function of this region of the face is expression and opening the eyes widely. The expression function is possible because of the firm attachments of the subcutaneous tissues to the frontalis muscle. The movement function is facilitated by the loose attachments of the frontalis muscle to the underlying tissues. You should note that like the lateral parts of the midface there is little movement in the temple. Feel your own skull. Feel the ridge of bone that separates your forehead from your temporal region, the temporal line . Now wrinkle up the skin on your forehead. Next wrinkle the skin on your temple. It is pretty much impossible. Try the same for your cheek and the area over your parotid. The anatomy serves the function.
Somehow, the anatomy lateral to the temporal line seems extra difficult to understand. Let’s start deep and work our way from the skull to the skin. Recall that the temporal line is the curved ridge of bone on the lateral aspect of the skull where the temporalis muscle attaches. The ridge runs across the parietal bone onto the frontal bone anteriorly. The temporal line is actually two lines. The superior temporal line is the arc of attachment of the temporalis fascia. The inferior temporal line is the arc of the attachment of the temporalis muscle. We have already said that from the surface of the skin, the temporal line marks the transition anatomically between the temple and the forehead. Intraoperatively, on a deeper plane, you see that a line of fusion of the layers of the temporalis muscle with the periosteum, the conjoined tendon , represents the boundary between the forehead and the temple.
The temporalis muscle is a muscle of mastication, not a muscle of facial expression. Its origin is the dense attachment of the muscle to the skull. The contraction of the temporalis muscle closes the mouth via the insertion on the coronoid process of the mandible. Motor innervation to the muscles of mastication is via the trigeminal nerve (V) rather than via the facial nerve (VII) for the muscles of facial expression.
Compare the function of this region lateral to the temporal line with the forehead medially. The temple has little expressive role. The main function is as a soft tissue covering that allows the movement of the underlying temporalis muscle. Unlike the frontalis muscle, which has loose attachments to the tissue posterior to it (the l oose areolar tissue of the pneumonic SCALP), the temporalis muscle has a strong attachment to the tissues posteriorly (the skull). The muscles of facial expression are anchored to the skin. The muscles of mastication are anchored to the underlying bones. The anterior fascial layers of the temporalis muscle have loose attachments to the skin anteriorly. This arrangement allows contraction of the temporalis muscle with minimal movement of the overlying soft tissue. Again, this is the opposite of the frontalis muscle, where the muscle fibers are strongly attached anteriorly. It is in this loose tissue plane, the superficial temporalis fascia, that the temporal branch of the facial nerve travels on its way to innervate the frontalis muscle.
Why all this discussion? Because when you understand human anatomy it should make sense. When you are learning anatomy it is more about memorization than understanding. As you learn anatomy, attempt to make the move to understanding whenever possible. As I have said many times before, keep in mind that like anatomy our educational process has layers. Come back to this anatomy a few times as you perform operations around the forehead and temple. You need this understanding to do the more complicated transblepharoplasty browplasty and the endoscopic and pretrichial forehead lifts. This anatomy is difficult to understand without seeing it in vivo or at least on video.
Now a bit of memorization is helpful (on the way to understanding). Learning the temporalis muscle fascia nomenclature is actually more complicated than understanding the anatomy! The fascial layer just anterior to the temporalis muscle itself is a part of the deep temporal fascia . This layer is easy to identify as a glistening layer of white tissue known as the superficial layer of the deep temporalis muscle fascia. This is the most important plane in the temple for the surgery you do. In most cases, you should go out of your way to identify this fascial layer. The temporal branch of the facial nerve lies in the loose fascia anteriorly, called the superficial temporal fascia or temporal parietal fascia (TPF) . To avoid damage to the temporal branch, you should just dissect anteriorly, directly against the glistening temporalis fascia ( Figure 6.16 ). Make every possible effort not to dissect within the loose fascial layer, the TPF. If you are unsure about whether you are at the proper depth over the temporalis muscle, make a small cut in the white fascia to see the underlying reddish muscle!

For the sake of our discussion, I use the term temporal parietal fascia (TPF) to mean the superficial temporalis fascia. When I refer to the temporalis fascia or deep temporalis fascia, I am referring to that fascial layer directly over the muscle (officially called the superficial layer of the deep temporalis fascia). As you would expect, it is an understanding of the anatomy that is really important, more than the terms, but these terms are definitely confusing.
Okay, get ready to ignore this; you might want to skip ahead. To make matters more confusing, there are two layers of deep temporalis muscle fascia. As you move inferiorly along the temporalis fascia toward the zygomatic arch, there is a fat pad. The temporalis fascia splits around the fat pad, becoming the superficial and deep layers of the temporalis fascia. You do not really need to know this anatomy for brow elevations, but learning about it is worthwhile if you do facial fracture repairs and facelift procedures.
Why again do you need to learn this? Because identifying the temporalis muscle fascia is the way to protect the temporal branch of the facial nerve. When performing browplasty operations, the temporal branch is safe if you are deep to it, dissecting against the temporal muscle fascia. A good way to learn this plane is when you do a temporal artery biopsy. The temporal artery lies in the same plane as the temporal branch of the facial nerve. To remove a piece of artery, you should dissect to the superficial layer of the deep temporalis muscle fascia ( Figure 6.17 ).

Now let’s add a few other layers of understanding to help with the forehead lift operations. We have already mentioned the conjoined tendon , which is a dense attachment of the periosteum to the scalp tissues at the temporal line. This is the anatomic boundary that separates the forehead from the temple. To allow the scalp to lift, you need to cut this attachment. In pretrichial, coronal, and endoscopic forehead lift operations, the dissection medial to the conjoined tendon is subperiosteal or preperiosteal. The lateral dissection is the plane we just discussed, anterior to the deep temporalis fascia (the glistening white layer). In the transblepharoplasty browplasty that I do, the medial portion of the brow dissection is preperiosteal in the loose tissue behind the frontalis muscle. The lateral dissection over the temple is the same as for the forehead lift operations, deep to the TPF anterior to the deep temporal fascia. Another way to think about this is to ask yourself Where is the temporal branch of the facial nerve? Lateral to the temporal line, the nerve runs in the layer superficial to the area you are dissecting. In any facial operation, it is always a good idea to know where the facial nerve branches are relative to where you are operating.
One last layer of learning is helpful for a jump-start in understanding facelift operations. The SMAS extends across the top of the skull into the temple and down into the face and neck, physically uniting the muscles of facial expression. To review, the SMAS envelops these structures:
Forehead: frontalis muscle and galea (extending to the occipitalis)
Temple: temporal parietal fascia (TPF)
Periocular: orbicularis, procerus, corrugator muscles
Face: all of the facial muscles
Neck: platysma muscle
As with eyebrow elevation operations, the strength of the lift is provided by tightening the SMAS. In the next chapter, we look at the same principle of SMAS tightening applied to facelift operations, lower blepharoplasty, and neck lifts.
Taking the history and doing the physical examination tend to occur simultaneously with our patients. Before the patient even speaks, you formulate an opinion about the patient’s structural abnormalities and the potential for correcting each abnormality. But beware; what you see and what the patient sees may be different. Resist the temptation to skip the history taking. Let the patient tell you what is bothering him or her. You may be surprised.
The most important part of the patient interview is the patient ’ s complaint . You should be asking yourself Why is the patient coming to see me? A complete understanding of the patient’s concerns and expectations for the outcome of the operation is essential to the success of your service to the patient. Is your patient concerned about the loss of the visual field? Or is your patient interested in changing the appearance of the eyes? Both are valid reasons for seeking your help, but each goal may require a different approach to meet your patient’s expectations. At some point during your discussion, you should ask your patient about the primary purpose of the operation: “Do you want to look better, or do you want to see better?”
Even functional goals involve a change in the patient’s appearance. Often it is helpful to have the patient show you the problem in a mirror. Remember, what you see may not be what the patient sees. When you think that you understand the patient’s problem, explain your perception, again using the mirror, to confirm that you and the patient have the same understanding of the problem. The ultimate success of the blepharoplasty and browplasty has as much to do with understanding the patient’s concerns and goals as it has to do with your surgical technique. For a moment, put yourself in the patient’s place. You may be having a procedure that in some way may change your appearance, whether that is the main intent or not. You, quite rightly, would like to know that your surgeon understands your goals! As a patient, you would welcome the reassurance of a statement such as:
You will look the same, but your peripheral vision will be better.
You will look the same but more rested and refreshed and less tired.
Every patient knows of someone, celebrity or friend, that has had an unwelcome result of plastic surgery!
Here is a warning : Remember that even though your patient may be having a blepharoplasty for functional reasons, he or she may anticipate a certain cosmetic result. If the main complaint is related to loss of vision, you and your patient should have a common understanding about what would be a reasonable cosmetic outcome related to the proposed operation. This avoids postoperative complaints after functional blepharoplasty, such as, “What about this wrinkle here?” or “I thought my eyelids would look more open.” If the patient’s primary concern is the aesthetic outcome, the patient is more likely to be pleased if the procedure is tailored to rejuvenation even if there is a visual function component to the problem. These procedures are generally not billed to medical insurance. When the goal of the operation is to restore visual function, this should be noted in the medical record as part of the documentation of the necessity for surgery.
You have my apologies for repeating some of this information. It is very important! If you apply it, both you and your patient will be more satisfied.
You need to review the patient’s general medical condition and medications. Most patients are healthy enough to tolerate the surgery you plan. Make sure hypertension is controlled. Estimates are that as many as one third of patients are taking an anticoagulant. In the past, the general recommendation for platelet inhibitors was to stop them for about 10 days before an operation. The thoughts on this recommendation are changing, however. First, many patients are taking these drugs for a good reason. You may be causing them more harm than good by stopping them. Second, there is good information in the literature showing that there is reasonable platelet function in less than 5 days. In fact, by day 4, platelet aggregation studies are at 80% normal. In general, I prefer that eyelid patients stop aspirin-containing medications 5 to 7 days preoperatively. A similar discussion is going on regarding discontinuing other anticoagulants. The general recommendation to stop warfarin and related medications is for 4 to 5 days. If the surgery is risky and discontinuing the anticoagulant is not advisable, bridging with heparin is an option. Most patients can stop antiinflammatory medications and any herbal supplements for 5 days with only minimal or moderate inconvenience.
The newer anticoagulants known as direct oral anticoagulants have a shorter duration of action. These medications include etexilate, apixaban, and rivaroxaban. They can be stopped 48 hours ahead of surgery if your patient has a creatinine clearance greater than 50 mL/min. In cases where bleeding presents a significant risk (as with deep orbital surgery), you might consider stopping them for up to 4 days with your patient’s internist’s approval. This is one of those judgment call issues discussed in the next paragraphs.
There is no simple answer to the question of when to stop antiplatelet or other anticoagulant therapy for the type of surgery that we are discussing. The complicated answer is an individual risk/benefit ratio. If the risk of bleeding is high and the risk of stopping the anticoagulant is low, it is obviously best to stop it. If the risk of bleeding is low and the risk of stopping anticoagulation is high, you should keep the patient anticoagulated and perhaps not do the operation. Every situation between these two is a judgment call. Timing issues come into play, also. An elective procedure can be delayed while anticoagulant effects wear off. More urgent situations involving fractures and tumors may not offer that option. These are also judgment calls.
Again, there is no simple answer. The recommendations for discontinuing anticoagulants as a whole favor less cessation. The wisest choice is to consult with the patient’s primary physician or cardiologist. They know the patient’s overall health better than you do and can help you make the decision. There are many papers regarding this topic in other surgical specialties (Mohs, cardiac, and carotid operations). The only paper regarding oculoplastic surgery specifically was written by Custer and Trinkaus in 2002. This paper and the majority of the current literature support this summary.
How about the feared “dry eye?” It is best to ask about a burning or foreign body sensation in the eyes and the use of artificial tears. Sensitivity to moving air from ceiling fans, air vents, or windshield defrosters may indicate a dry eye. Asking if the patient has been told if she or he has a dry eye is not helpful. Many patients have been given this diagnosis incorrectly, and it will not likely complicate your blepharoplasty result. A patient who benefits from using artificial tears once a day does not really have a dry eye. We talk about this topic more in Chapter 10 .
It is helpful to know if the patient has had a previous blepharoplasty. If so, any drooping upper lid skin is usually the result of untreated eyebrow ptosis. You should inquire as to any other facial operations or trauma. During your interview, you may notice a sign of facial asymmetry and want to ask about any preexisting facial nerve palsy.
In the physical examination, you answer these questions:
What is the normal anatomy and function?
What is the structural abnormality? How does the patient’s anatomy differ from normal? How are functions altered?
What is the patient’s complaint? What are the patient’s goals (functional or cosmetic)? What is the patient’s desired outcome (specific postoperative appearance)? What is the potential for meeting these goals?
What are the options for attaining the patient’s goals? What is the best surgical plan?
Are there contraindications for getting the desired result?
Do not memorize these questions. You are already answering these questions about your patients without knowing it. Many of the problems that we address in this chapter are really not abnormalities; rather, they are the normal anatomic consequences of aging. For most patients, you compare their current anatomy with the youthful anatomy present many years before. We look at the examination now with these thoughts in mind.
Examine each portion of the periorbital anatomy, including the eyebrow, upper lid, and lower lid. It is a good idea to perform an anterior segment examination to identify any coexisting eye abnormalities, especially factors related to maintaining a healthy precorneal tear film.
During the examination, compare the patient’s periocular anatomy to the stylized normal or desirable anatomy for the patient’s gender. As you gain experience, you learn to visualize the patient’s potential for that perfect look or normal function.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here