Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The most common indication for pediatric cervical spine (C-spine) imaging is trauma. Although cervical spinal injuries are rare in children, the result can be devastating. The role of the radiologist is crucial in the early detection of cervical spinal injury (CSI) that may require immediate clinical attention. Imaging interpretation of the C-spine is particularly challenging and requires a thorough knowledge of its unique anatomic characteristics as the spine continues to develop and mature during childhood, reaching adult features at approximately 12 years of age. Knowledge of developmental changes allows differentiation of normal age-related anatomy from traumatic injury. Pediatric CSI results in extensive variability of injury patterns, closely related to age and mechanism of trauma. This chapter includes a review of the normal C-spine anatomy and common variants, a systematic approach for radiological interpretation, and illustrations of the most common traumatic injuries of the pediatric C-spine. The concept of “clearance” of the pediatric C-spine in the emergency department setting will also be discussed.
Trauma leads as the most common cause of pediatric morbidity and mortality. Spinal injury occurs in 5% of trauma cases, and the region most frequently affected in children is the C-spine (60%–80% of cases). The incidence rate of CSI in pediatric blunt trauma is 1% to 1.5%, occurring more often in boys. CSI tends to increase with age and peaks at 9 to 12 years of age. Although CSI is rare, it can result in devastating outcomes, such as significant neurological injury or even death. The anatomy and biomechanics of the immature pediatric spine predispose to specific patterns of injury that are different from the adult spine. A study recently published by evaluated a large, multicenter cohort of patients, including from 17 PECARN (Pediatric Emergency Care Applied Research Network) sites. This study retrospectively classified CSI in 540 patients and demonstrated that patterns of CSI with blunt trauma are closely related to age and mechanism of trauma , as has been also supported by other publications.
Assessment by age subgroups shows that motor vehicle collision (MVC) and falls are the most common mechanisms of injury in both the youngest children (<2 years of age) and children aged 2 to 7 years. Pedestrian struck by motor vehicle is also a common mechanism in children aged 2 to 7 years. In the group ≥8 years of age, sports injuries and MVC are more frequent. CSI related to sports accounts for a quarter of ER visits of children. A multicenter retrospective case control study in children younger than 16 by showed that football was the sport most frequently related to CSI, as well as diving, gymnastics/cheer, and hockey. CSI was also prevalent in unorganized activities such as trampolining, rough play or falls.
Patterns of CSI are closely related to age and mechanism of trauma. Injuries from the atlantooccipital articulation to the C2 level, known as axial injuries , are more often seen in children ≤3 years of age. Factors that contribute to this pattern of injury include a large head relative to the C-spine with a fulcrum of motion at the C2/C3 level, underdeveloped neck musculature, lax ligamentous structures, vertebral body morphology, and the presence of vertebral synchondroses. Axial injuries include C1 and C2 fractures, as well as atlantooccipital dislocation (AOD) and atlantoaxial rotary subluxation (AARS). Increased morbidity and mortality is seen with AOD and may result in death. Cord injury is also more common in the young age group and can lead to severe neurological deficits. In children younger than 8 years, the bony spinal column allows significant stretching without tearing, while the spinal cord is much less stretchable and can result in shear injury.
Subaxial injuries , from the level of C3 to C7, occur more often in children older than 8 years and can frequently present with ligamentous injury and/or vertebral body fractures. At this age the fulcrum of motion is at the C5/C6 level, the neck muscles are more developed, and most of the vertebral synchondroses are fused. CSI in the teenager is similar to the adult.
Multilevel injuries are extremely rare in pediatric CSI. Injury to other organ systems is common in high-energy trauma and contributes to unfavorable outcome. Head trauma is the most common associated injury.
SCIWORA (spinal cord injury without radiographic abnormality) is a term that was first used by to describe radiographically normal cases in patients with neurological abnormality. Historically, this term refers to spinal cord injury in the absence of findings on plain radiographs. However, with the advent of new imaging modalities to evaluate the spine, such as computed tomography (CT) and magnetic resonance imaging (MRI), this term has become confusing over time. Several authors have recently proposed the redefinition of this term, suggesting that “real-SCIWORA” should refer only to spinal cord injury with negative neuroimaging findings on all modalities, including plain radiographs, CT, and MRI. The incidence rate of SCIWORA in pediatric CSI ranges from 5% to 67%; this wide range may be in part related to differences in the use of this term among clinicians. The lack of MRI studies at the time of diagnosis may result in higher reports of SCIWORA by pediatricians and emergency department physicians, although it is often used less by neurosurgeons and orthopedic surgeons, who usually have magnetic resonance (MR) studies available at the time of diagnosis.
The radiologist must be aware of the normal developmental changes and anatomic variants of the pediatric C-spine on radiological studies to detect pathology and avoid misinterpretation. These include changes in vertebral morphology during the first decade of life, as well as the presence of synchondroses, apophyses, and secondary centers of ossification. Pitfalls may result from technically inadequate plain radiographs related to head positioning.
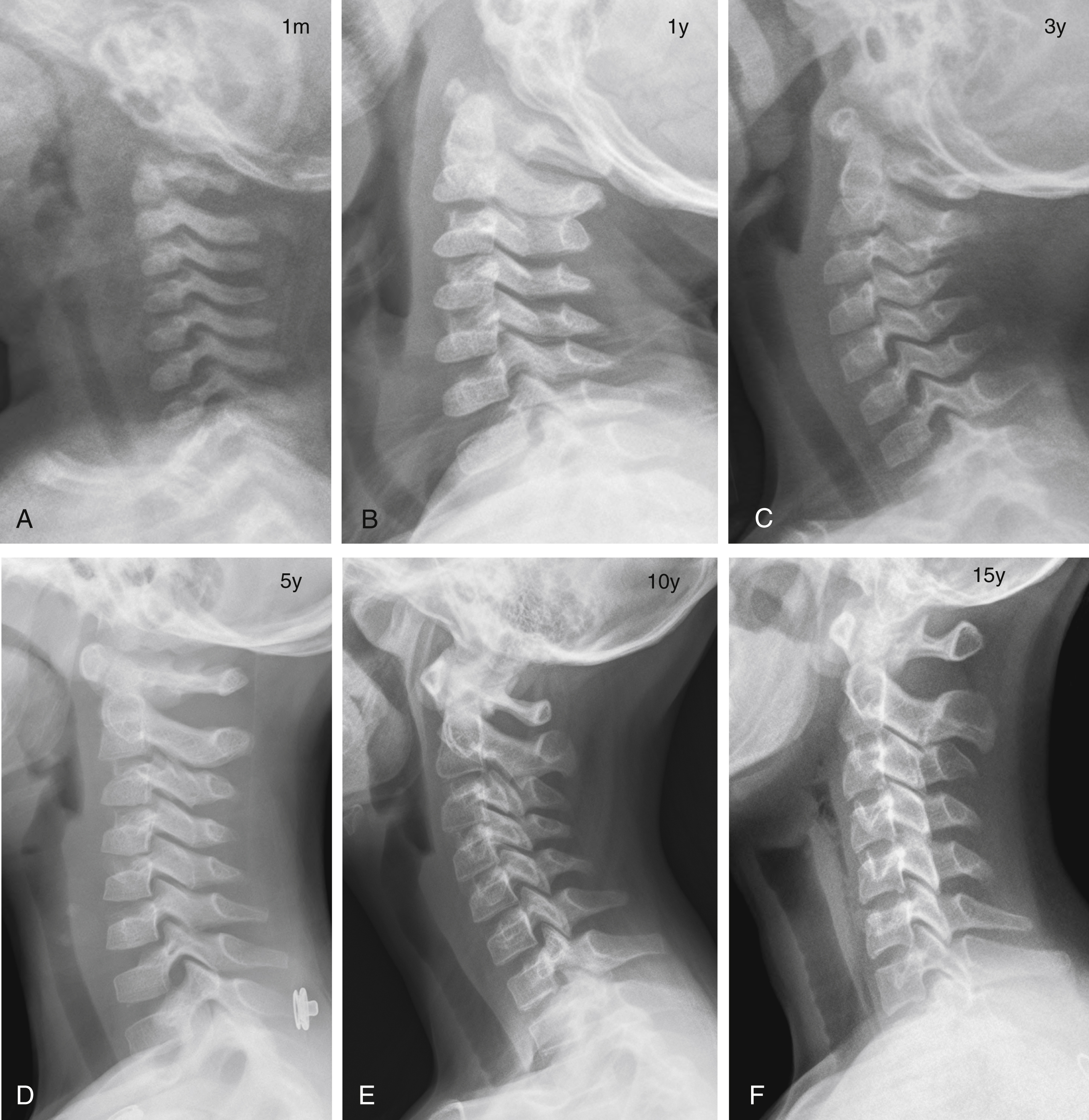
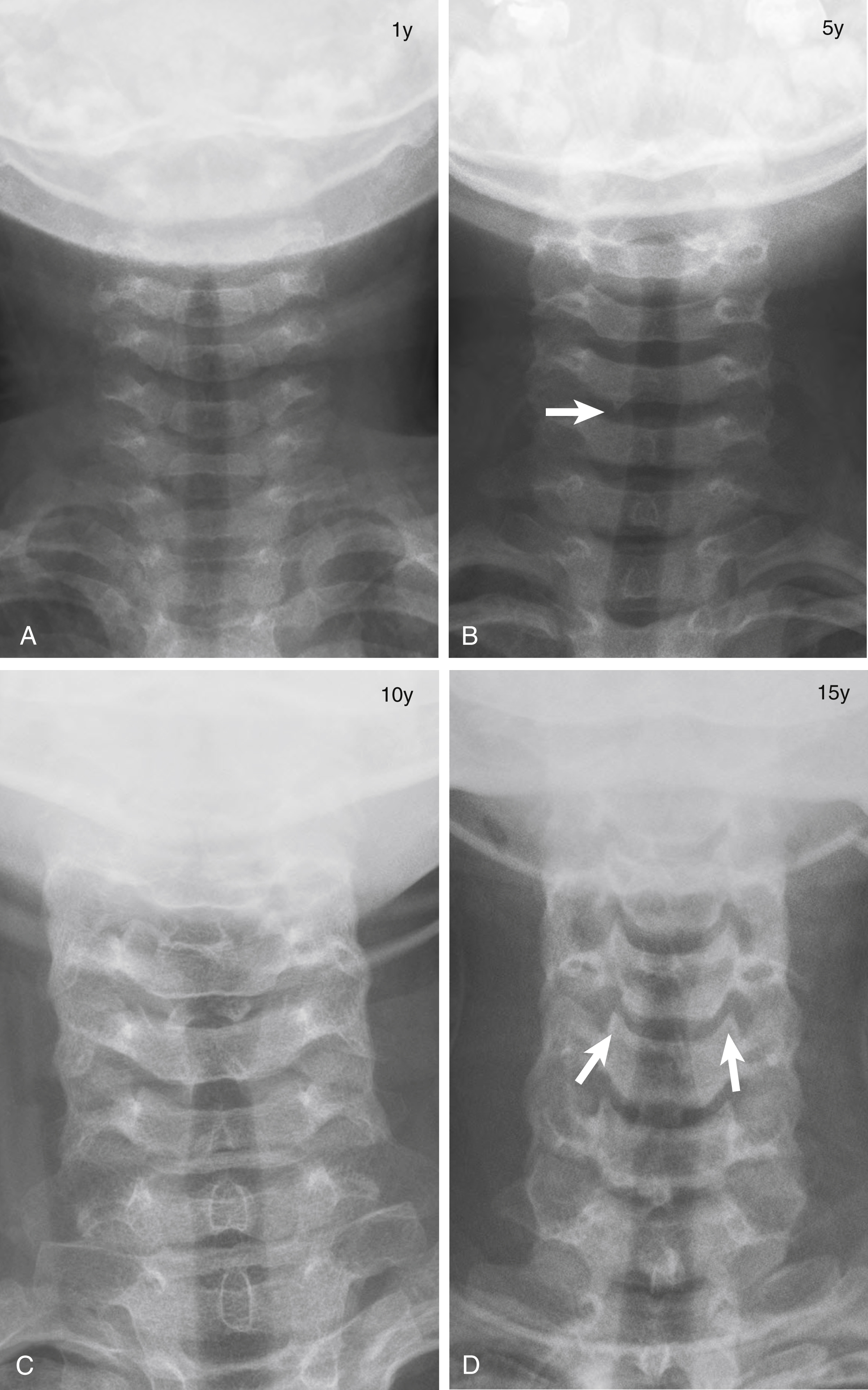
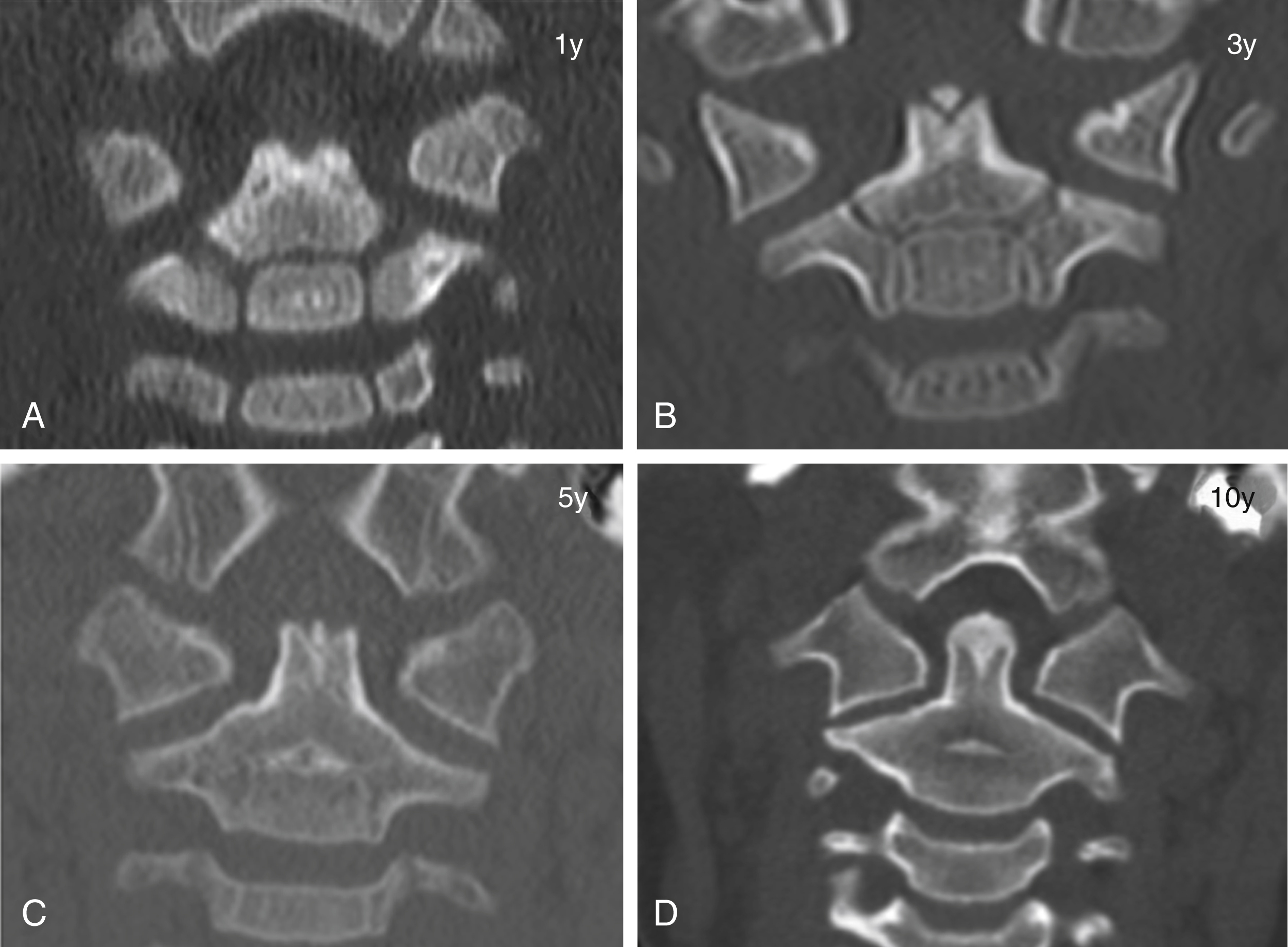
The shape of the vertebral bodies changes from birth until approximately the first decade of life. In infants, cervical vertebral bodies are oval shaped, whereas at around age 2 to 3 years, these appear relatively flattened. From 3 to 8 years of age, vertebral bodies demonstrate mild anterior wedging, especially C3 through C5, and should not be mistaken for compression fractures. At about 10 years of age, the cervical vertebrae acquire a more rectangular or square shape, similar to the adult spine. Other unique findings in the young child include shallow articular joints with slightly uncovered appearance of the facets and underdeveloped spinous processes with mild upward orientation ( Figs. 28.1 and 28.2 ). Uncovertebral joints form during adolescence (see Fig. 28.2 ).
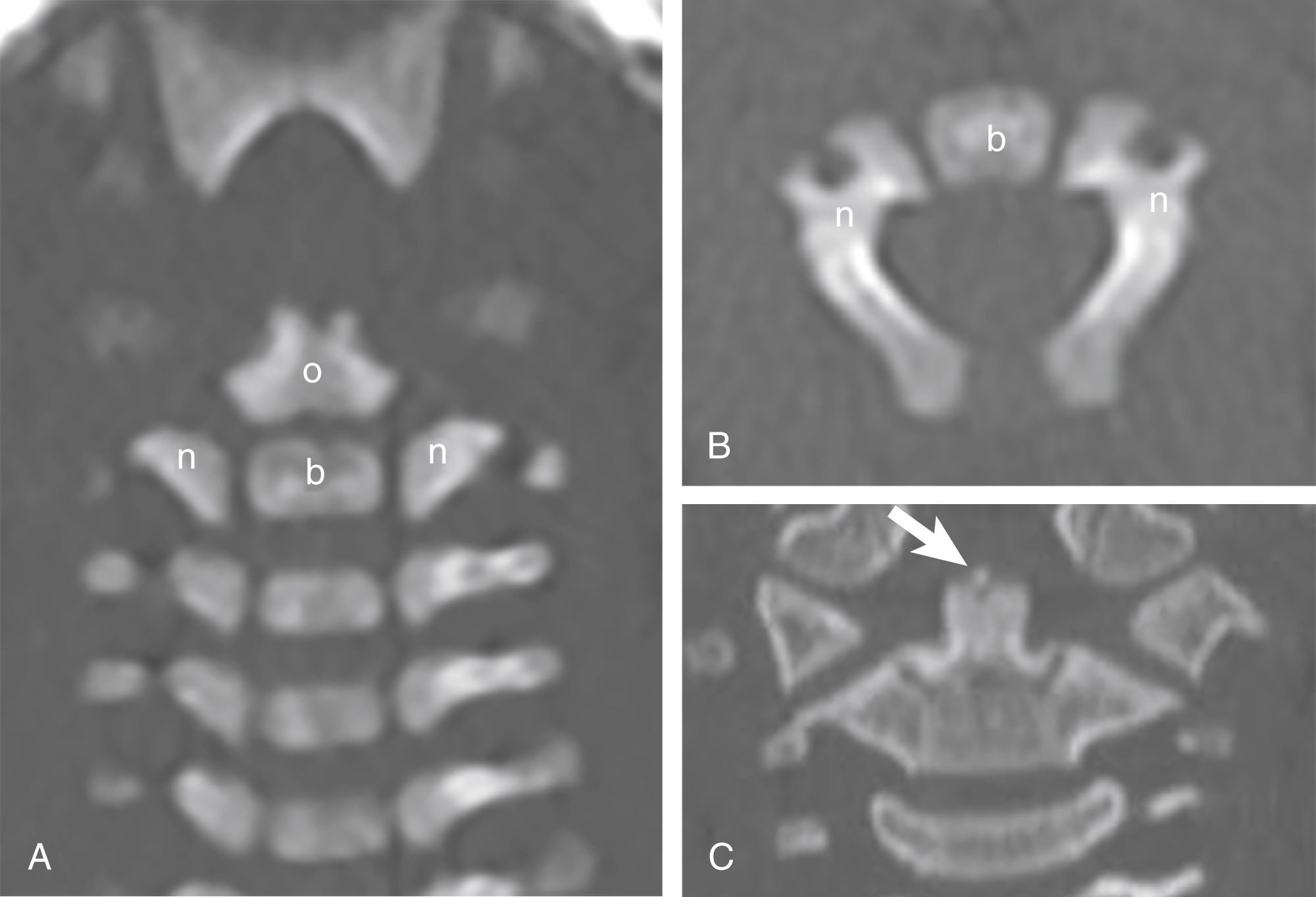
C1 is formed from three primary ossification centers ( Box 28.1 ): the anterior arch and two neural (posterior) arches ( Fig. 28.3 ). C1 is a ring structure and does not have a body. The anterior arch is mainly cartilaginous at birth, but some degree of ossification may be present in 20% of newborns. Otherwise, ossification of the anterior arch is expected to be visible at around 12 months of age but can be delayed until 24 months of age. The C1 anterior arch can also form from multiple ossification centers (2–4) in 25% of children. The most common variant is two ossification centers in 18% of the population ( Fig. 28.4 ). Occasionally the anterior arch can be absent, and the neural arches may fuse anteriorly.
Ossification: present at birth (20%), visible by 12 months
Fusion: 6–8 years
Ossification: begins at seventh week of fetal life
Fusion: 3–5 years
Ossification: present at birth
Fusion
Odontocentral synchondrosis: begins at 3–6 years, complete by 11–12 years
Odontoneural and neurocentral synchondroses: 3–6 years
Posterior arches: 2–3 years
Ossification: appears by 3–6 years
Fusion: 10–12 years
Ossification: present at birth
Fusion: neurocentral synchondroses: 2–3 years
Posterior arches: 3–6 years
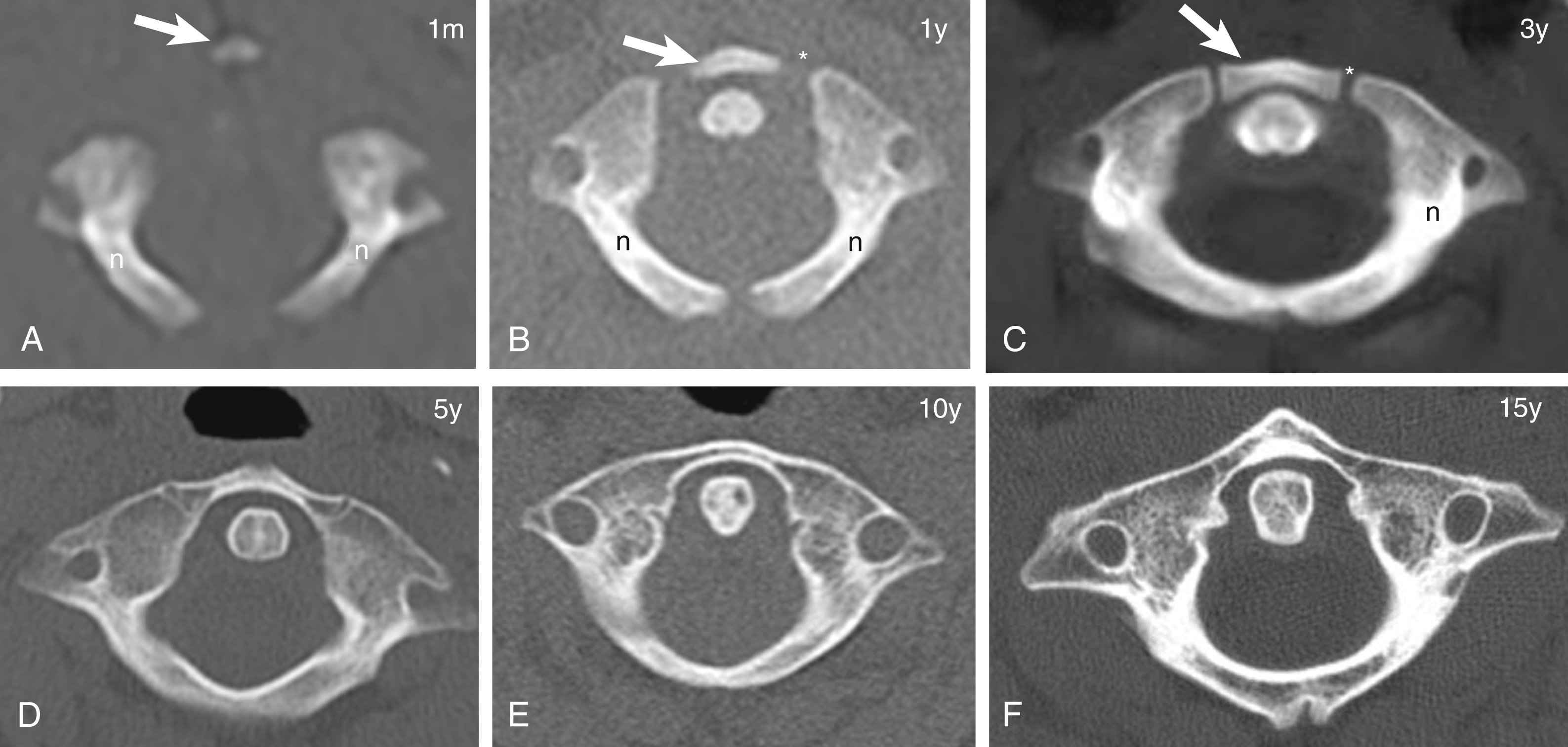
The posterior arches begin to ossify in the seventh week of fetal life. The neurocentral synchondroses are between the anterior arch and posterior arches (see Fig. 28.3 ). A completely ossified anterior arch with fused neurocentral synchondroses usually occurs by 6 to 8 years of age. The posterior arches usually fuse by 3 to 5 years of age (see Fig. 28.3 ). Although rare, incomplete fusion of the posterior arches or a midline cleft may be seen in children ≤8 years of age. Another anatomic variant includes unilateral or bilateral paramedian clefts (see Fig. 28.4C ).
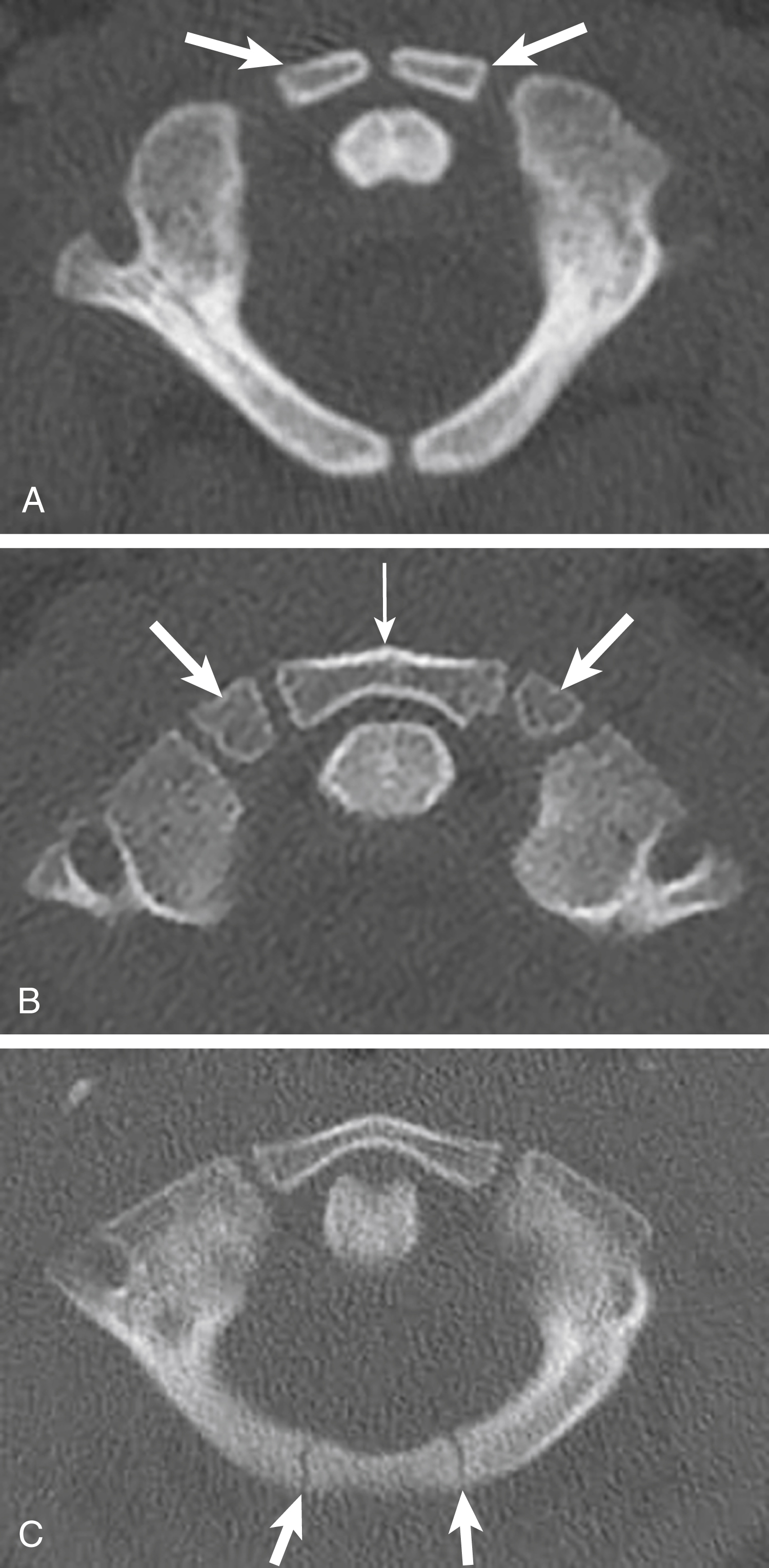
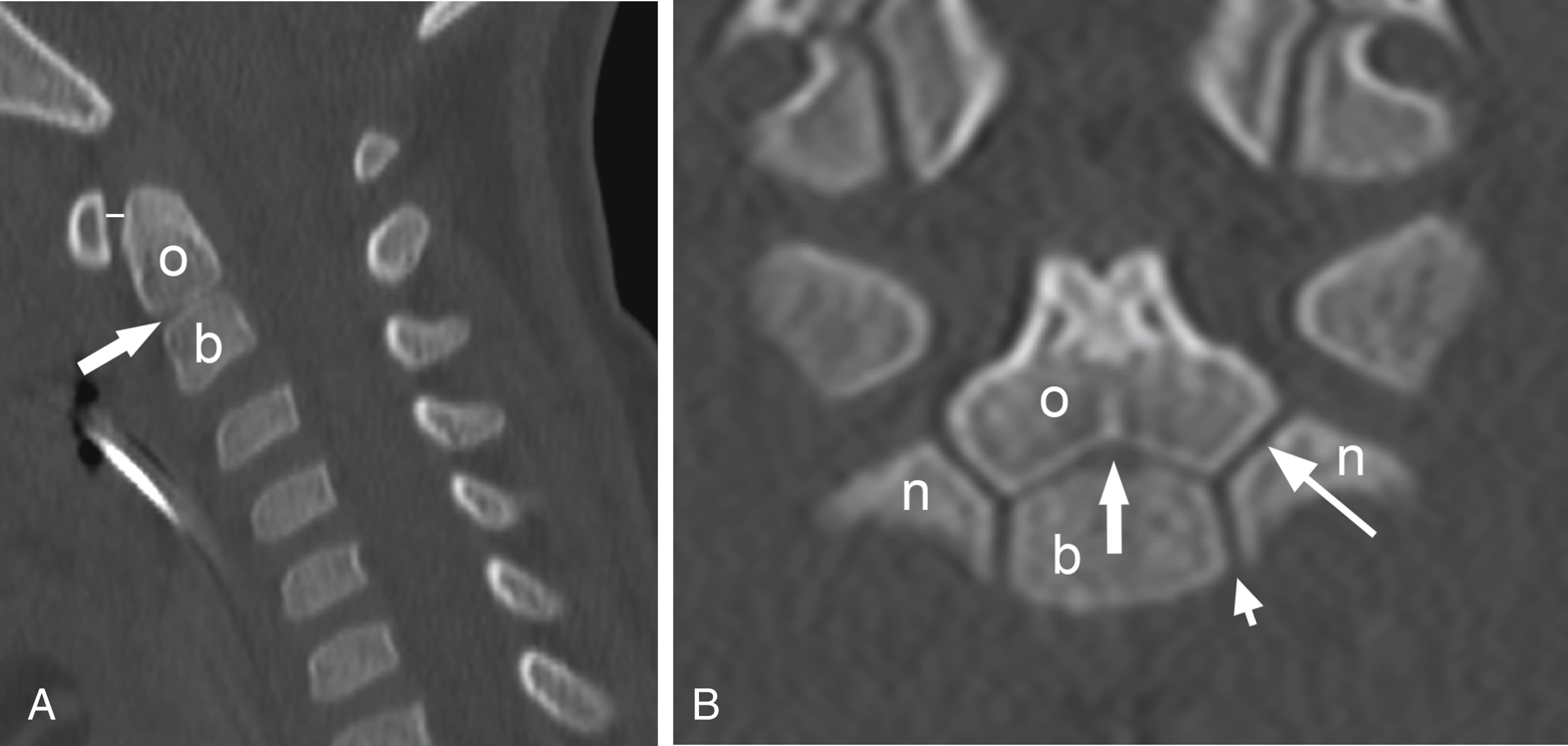
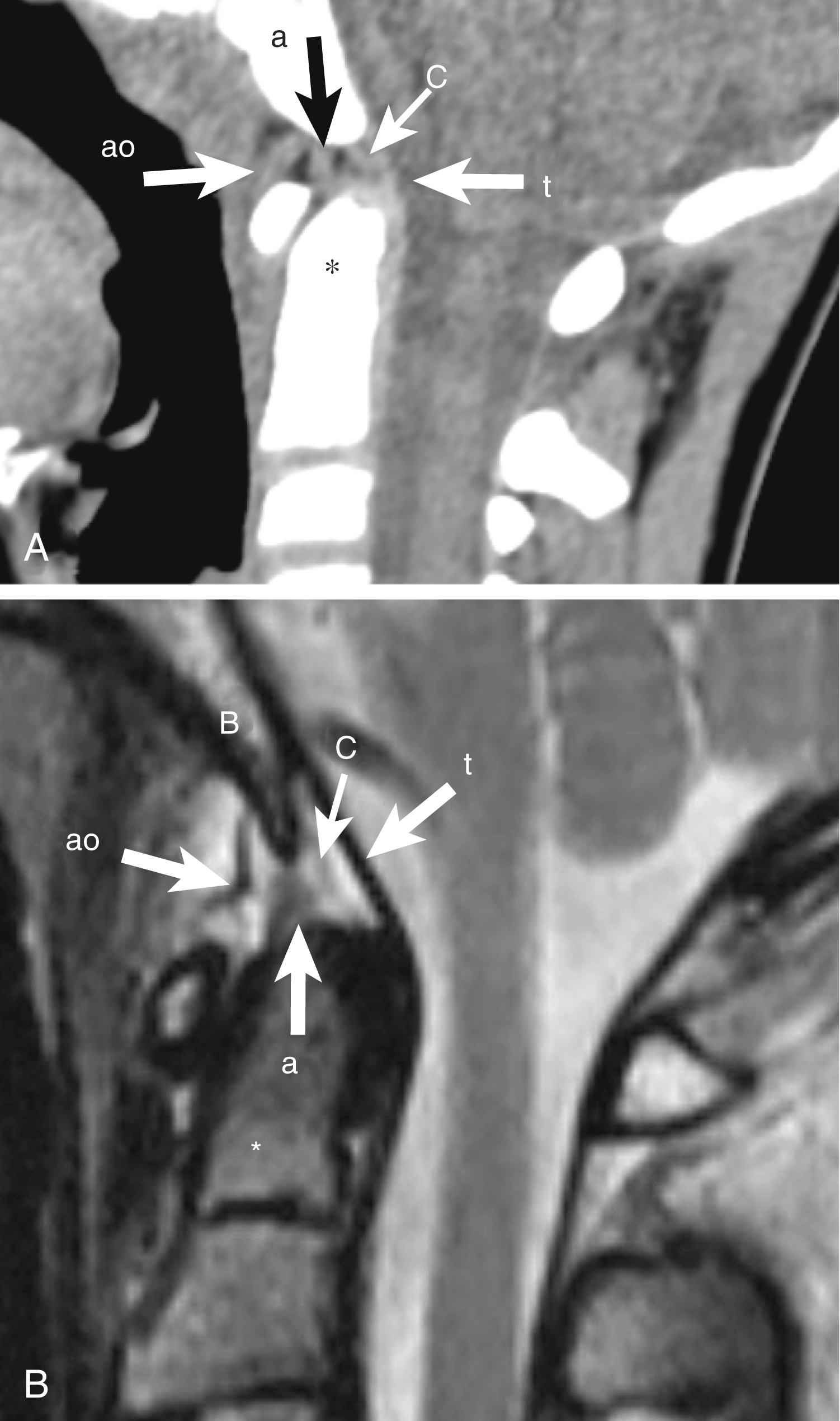
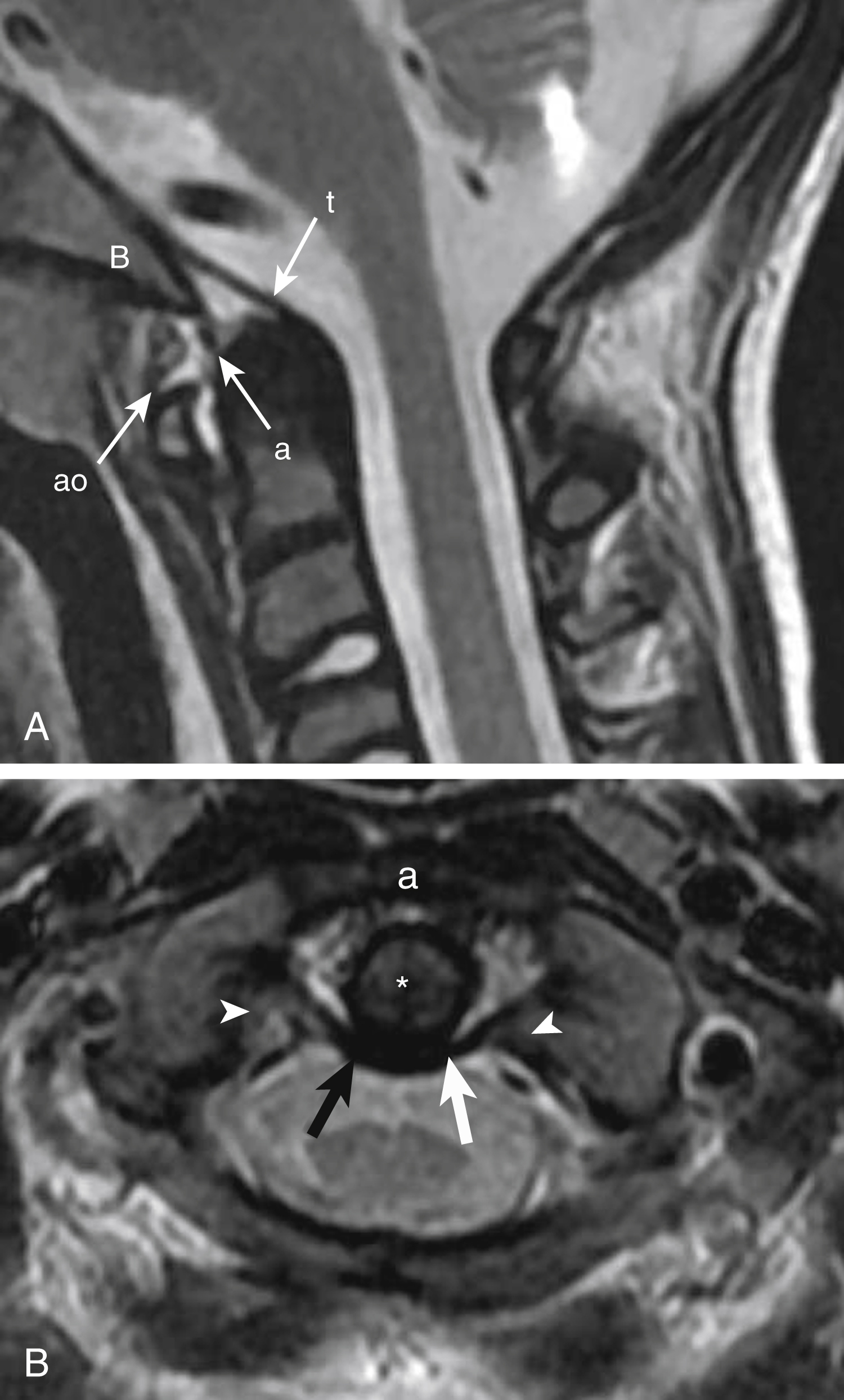
C2 is formed by four primary ossification centers that are present at birth: the body, two neural arches, and the odontoid process ( Fig. 28.5 ). A single secondary ossification center, the os terminale (tip of the odontoid process), appears between 3 and 6 years of age (see Fig. 28.5C ). C2 synchondroses can be seen until approximately 8 years of age and should not be mistaken for fractures. The subdental (odontocentral) synchondrosis ( Figs. 28.6 and 28.7 ), located between the odontoid process and the body, begins to close around age 3 to 6 years of age and usually fuses around 11 to 12 years of age. Bilateral neurocentral synchondroses separate the body from each neural arch, while bilateral odontoneural synchondroses separate the odontoid process from each neural arch; these fuse between 3 and 6 years of age (see Figs. 28.6 and 28.7 ). The tip of the odontoid process (os terminale) fuses at approximately 12 years of age. Because the odontoid process forms from two ossification centers in utero, a vertical remnant synchondrosis can occasionally be seen. The posterior arches fuse around 2 to 3 years of age.
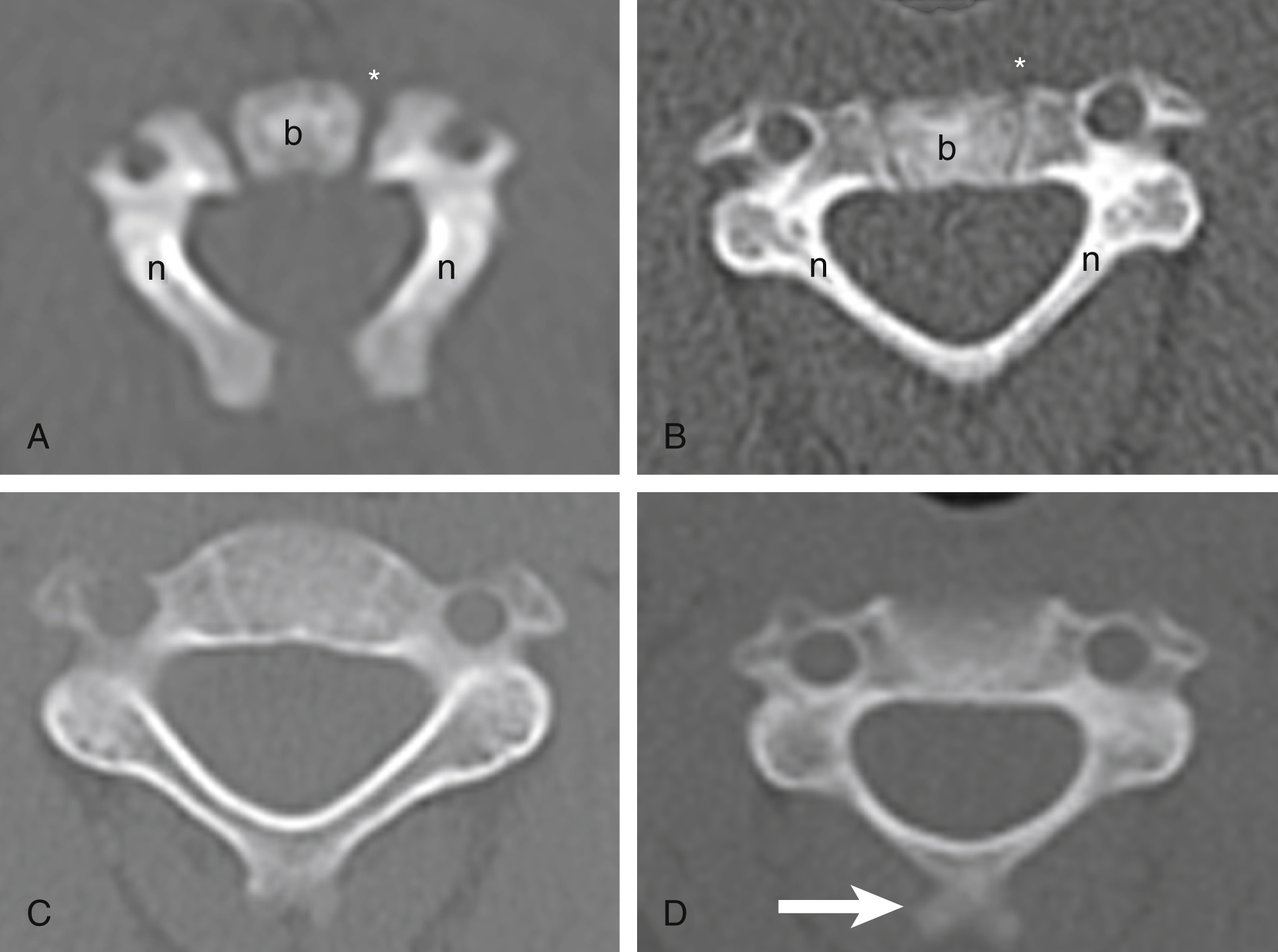
C3–C7 vertebrae each form from three ossification centers: the body and two neural arches. The neural arches fuse posteriorly at around 2 to 3 years of age, while the body and neural arches fuse between 3 and 6 years of age. C7 has the longest spinous process and C3 to C7 commonly have bifid spinous processes ( Fig. 28.8 ).
Secondary ossification centers of C3–C7 include ring and spinous process apophyses. A ring apophysis is a wedge-shaped ossification center along the anterior and inferior aspect of the vertebral body and may be present at multiple levels. Ring apophyses ossify around 10 years of age and fuse between 18 and 25 years of age. The apophysis of the tip of the spinous process is seen more often at the C6 and C7 levels ( Fig. 28.9 ).

The craniocervical junction (CCJ) is composed of the atlantooccipital and atlantoaxial joints, which are responsible for preserving stability, mobility, and rotation of the CCJ. The atlantooccipital joint allows for flexion and extension (F/E) movements and mainly depends on bony structures (the occipital condyles over the C1 sockets). The atlantoaxial joint allows for rotational movements and mostly depends on ligamentous structures. The major ligaments of the CCJ include the transverse ligament (major component of the cruciate ligament), alar ligaments, apical ligament, tectorial membrane (continuation of the posterior longitudinal ligament), anterior atlantooccipital (AAO) membrane and atlantoaxial ligament (continuation of the anterior longitudinal ligament), and posterior atlantooccipital (PAO) membrane (continuation of the ligamentum flavum) ( Fig. 28.10 ).
Additional ligamentous complex of the posterior C-spine includes the ligamentum flavum and interspinous ligaments (continues cephalad as the ligamentum nuchae).
The transverse ligament is the thickest and strongest of the CCJ and is a major component of the cruciform ligament, serving as the major stabilizing ligament of the atlantoaxial joint ( Fig. 28.11 ). The superior and inferior limbs of the cruciform ligament are small and do not provide significant CCJ stability. The transverse ligament courses posterior to the odontoid process of C2 and attaches to each lateral tubercle of C1, keeping the odontoid process anteriorly against the posterior aspect of the anterior C1 arch. The spinal cord is located posterior to this ligament. The transverse ligament allows for atlantoaxial rotation up to approximately 47 degrees, whereas the alar ligaments limit excessive rotation. Rupture of the transverse ligament results in C1/C2 subluxation.
The alar ligament attaches to the odontoid process and skull base. This ligament limits excessive rotation and lateral bending of the neck. It also stabilizes the atlantoaxial joint, preventing C1/C2 subluxation. The alar ligament may have a cranial caudal or horizontal orientation, and its shape is variable: tubular, round, elliptical, rectangular, or wing-shaped.
The apical ligament attaches to the tip of the odontoid process and basion and courses posterior to the alar ligament. Some have suggested the lack of function of this ligament. A study in cadavers demonstrated the absence of the apical ligament in 20% of specimens.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here