Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Intractable disabling epilepsy, a localizable epileptogenic zone, and a low risk of (unacceptable) postoperative deficits are considered to be the three basic tenets that make a patient a candidate for epilepsy surgery.
One should apply surgical technique for extratemporal resections to match the underlying cause and functional boundaries.
Functional hemispherectomy techniques are especially effective in disease states involving one hemisphere, such as perinatal stroke, Sturge-Weber syndrome, or Rasmussen encephalitis.
Laser ablation therapy provides a less invasive and shorter hospitalization treatment for focal lesions with clearly definable boundaries.
Epilepsy represents a broad spectrum of disease processes sharing the common characteristic of repetitive, spontaneous seizures. Patients who are medically intractable and have surgically remediable foci (which may be highly focal or as broad as an entire hemisphere) have surgical resection as the only alternative with a reasonable chance of seizure freedom. Other surgical options can be effective as palliation as well.
The previous chapter explained temporal lobe epilepsy and surgery of temporal lobectomy. In addition, a significant number of epilepsy patients have an epileptogenic zone outside the medial temporal lobe. These so-called extratemporal lobe epilepsy (ETLE) patients present unique management challenges. As the characteristics of ETLE have become better understood, the distinctive management challenges have become better defined. The result has been the development of new concepts of epileptogenesis, new diagnostic technologies, and, from a neurosurgical perspective, the development and refinement of surgical techniques.
ETLE refers to epilepsy arising outside the temporal lobe (typically any involvement outside of the medial temporal lobe structures) and may be associated with a variety of etiologies. Seizure semiology in ETLE may be complex depending on the site of seizure origin. The nature of ETLE lends itself to areas of ictal onset that may not necessarily result in clinical manifestations until the symptomatogenic zone becomes activated. With extratemporal areas of ictal onset, the location suggested by semiology has a greater propensity to be a result of secondary spread, leading to potential diagnostic confusion.
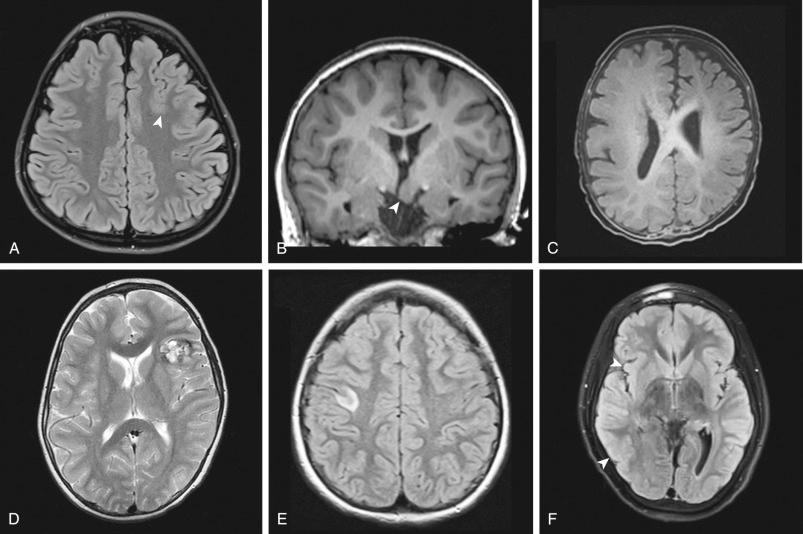
The International League Against Epilepsy (ILAE) simplified the classification of epilepsy by separating it into the “known” and “unknown” groups. The “known” or “symptomatic” group means epilepsy caused by a known disorder, including structural, metabolic, inflammatory, infectious, toxic, or genetic. By temporal relationship, the subdivision could be defined by acute (stroke, intoxication, or encephalitis), remote (posttraumatic, poststroke, or postencephalitis), and progressive (brain tumor). Imaging, particularly magnetic resonance imaging (MRI) examination, can define several potentially epileptogenic lesions, including cortical dysplasia and tumors along with other conditions such as tuberous sclerosis, Sturge-Weber syndrome, hemimegalencephaly, vascular malformations, and hypothalamic hamartoma ( Fig. 56.1 ). These factors can result in a broad spectrum of imaging findings, complex seizure semiology, and potentially diffused electroencephalography (EEG) data.
EEG data may be particularly difficult to interpret because of rapid spread and artifact from muscle movement during the seizure. It is particularly difficult to record epileptic activity from on-scalp EEG deep cortical areas, such as the interhemispheric and insular regions. Patients whose seizures start in these areas can present challenges, as electrical seizure activity may be absent on standard EEG arrays, or it may falsely localize as originating in another area entirely.
Intractable epilepsy, a localizable epileptogenic zone, and a low risk of postoperative deficits are three components that determine whether a patient can be considered a candidate for epilepsy surgery. It is important to recognize that medical intractability makes a patient a candidate for further investigation regarding the appropriateness to undergo surgery for epilepsy, but it does not guarantee that surgical management should ultimately be offered. The evaluation for epilepsy surgery should be comprehensive and include a high-resolution MRI scan, video-EEG monitoring, positron emission tomography (PET), and neuropsychiatric testing. A high probability of improving a patient's overall quality of life must be confirmed before undertaking the procedure.
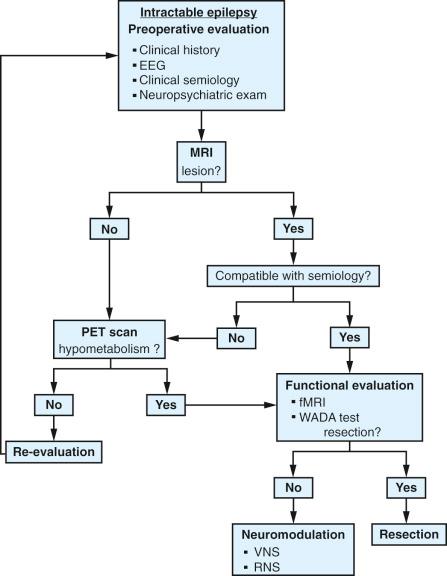
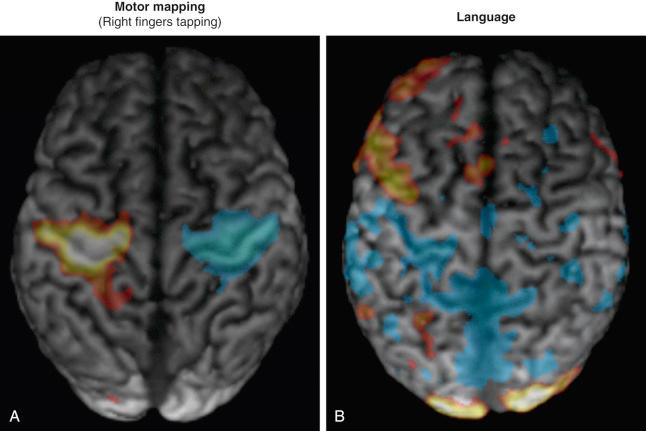
The starting point for any patient evaluation should include a detailed history and physical examination, with special focus on seizure semiology. Lateralizing and localizing signs, such as ictal eye movements, motor or sensory features, the presence or absence of ictal speech, and the presence or absence of aura, should be noted. Video-EEG monitoring data allow correlation of a patient's behavior during seizure with the changes recorded on scalp EEG. MRI studies, including an axial T2 sequence, axial and coronal fluid-attenuated inversion recovery (FLAIR) sequences, a sagittal T1 sequence, and a high-resolution (thin-cut) coronal magnetization prepared rapid gradient echo (MPRAGE) sequence, help to localize for patients with suspected extratemporal lesions. If MRI and EEG information is inconclusive or MRI is normal, additional studies, such as subtraction single-photon emission computed tomography (SPECT), PET, or magnetoencephalography (MEG), provide complementary information and may help in the formulation of a surgical hypothesis ( Fig. 56.3 ). These studies may also be used as an adjunct in patients with multilobar lesions or discordant data. Functional studies, such as functional MRI (fMRI) and the Wada test (intracarotid sodium amobarbital test), may be used to study eloquent regions of the brain ( Fig. 56.4 ).
![Figure 56.3, Examples of left frontal hypometabolism seen on [ 18 F]-fluorodeoxyglucose (FDG) positron emission tomography (PET) scanning. (A) Frontal view. (B) Left midsagittal view. (C) Axial view. (D) Three-dimensional reconstruction. Figure 56.3, Examples of left frontal hypometabolism seen on [ 18 F]-fluorodeoxyglucose (FDG) positron emission tomography (PET) scanning. (A) Frontal view. (B) Left midsagittal view. (C) Axial view. (D) Three-dimensional reconstruction.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/ExtratemporalProceduresandHemispherectomyforEpilepsy/2_3s20B9780323431408000561.jpg)
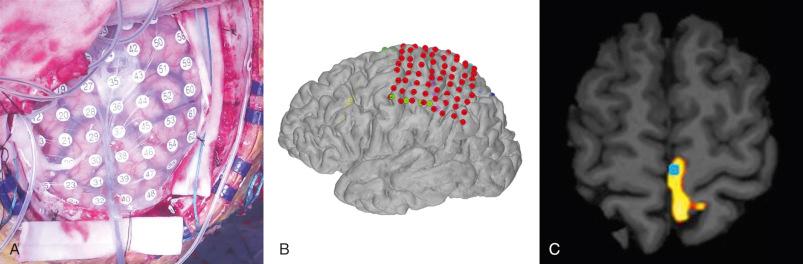
All the data gathered should be presented in a multidisciplinary conference that includes epileptologists, neurosurgeons, and neuropsychologists, with input from psychiatrists, social workers, and neuroradiologists on the team. When localization predicted from the various studies is concordant, then a strong hypothesis can be made about seizure onset and, therefore, the surgical plan. If a focus is suspected but not confirmed, an invasive monitor may help to localize the seizure focus, whether using depth electrodes, subdural electrodes, or a combination, ideally driven by whatever would be most useful for a given patient.
Invasive intracranial electrodes also have a distinct advantage in mapping the functional cortex. Consequently, their placement should be considered when epilepsy is thought to arise from within or near the eloquent cortex. They are especially useful for localizing functional cortex in patients who are unable to tolerate an awake craniotomy ( Fig. 56.5 ).
A broad range of surgical techniques can be considered for the treatment of extratemporal epilepsy. These procedures can be divided into resective techniques and palliative techniques. Resective techniques include lesionectomy, tailored focal resection, lobectomy, multilobar resections, and hemispherectomy and its variants. Palliative techniques include corpus callosotomy, multiple subpial transections, vagal nerve stimulation, and responsive cortical stimulation. Other stimulation techniques currently under investigation include thalamic targeted deep brain stimulation and transcranial stimulation.
The surgical approach depends not only on surgical and functional anatomy, but also on age of the patient, medical comorbid conditions, and anticipated underlying disease. Certain types of focal cortical dysplasias, neoplasms, and cavernomas can often be resected with electrocorticographic guided lesionectomy, typically resulting in a good surgical outcome. The general tenet is focal resections for focal disease and progressively larger areas of resection for more diffused or multifocal disease. The extension of a resection beyond the area of visible lesion may be performed with the assistance of intraoperative electrocorticography, somatosensory evoked potentials (SSEPs), or extraoperative recording with the use of implanted intracranial electrodes.
To be considered for hemispherectomy, the ideal patient should have epilepsy arising from a single affected hemisphere. Techniques of hemispherectomy were sorted into two major groups: (1) those that completely remove the cortex from the hemisphere and (2) those that associate partial cortical removal and disconnection. Anatomic hemispherectomy remains in use for selected pathologic processes such as hemimegalencephaly and diffuse malformations of cortical development, in part because of the highly distorted anatomy that can be encountered. It is also commonly utilized when prior disconnective hemispherectomy techniques have failed. Disconnective hemispherectomy techniques are usually considered in patients with perinatal stroke, Sturge-Weber syndrome, or Rasmussen encephalitis. The goal of these procedures is to isolate the hemispheric cortex while reducing the perioperative risks that are more prevalent with the anatomic technique (blood loss and, possibly, a reduced rate of postoperative hydrocephalus). From a practical standpoint, this translates to disconnection of the horizontal frontal fibers, mesial temporal structures, corpus callosum, and the internal capsule and corona radiata. The completeness of disconnection, in addition to seizure etiology, relates directly to surgical outcome.
Each hemispherectomy technique has unique advantages and disadvantages, with selection of technique individualized to the patient's anatomy and underlying disease. For patients with malformations of cortical development, such as hemimegalencephaly, anatomic hemispherectomy is the most direct way to completely remove the malformed tissue. These patients often have small ventricles and no clearly defined gray/white interface; it is difficult to complete disconnection via a less invasive hemispherectomy technique. However, the disadvantage to the anatomic technique is a slightly higher risk of perioperative morbidity and a higher incidence of postoperative hydrocephalus. The functional technique is well suited to patients with Rasmussen encephalitis, where the normal gray/white anatomy is preserved. Advantages to these less invasive techniques include reduced blood loss and risk of hydrocephalus. The disadvantage is the higher reoperation rate when seizures persist postoperatively and cortical tissue is left in place.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here