Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Design and plan the suite about 12–18 months in advance of the anticipated starting date for using the suite.
Consult experts in medical office design and construction.
Decide which type of surgical facility is right for your practice.
Decide if accreditation should be pursued.
A bigger facility can often be better in the long term.
Ensure patient privacy.
Plan for plenty of storage.
Ensure that walls and floors are washable.
Equip surgical rooms with power operating tables.
Plan for maximum use of light.
Consider used equipment.
Be prepared for emergencies.
Study reimbursement trends.
Well-designed surgical office space is critical for the comfort of the surgeon, staff, and patients, for office efficiency, and ultimately for practice success. Identifying and designing the proper space for your practice requires a significant investment, not only in time and money but also emotionally. As such, it is important to plan carefully and seek expert design and architectural advice early in the process. This chapter is intended to serve as a starting point in the process of designing a surgical suite, and will review the various types of outpatient surgical facilities as well as design, planning, and reimbursement considerations.
Many dermatology offices have a specific room, often designated the “procedure” or “minor surgery” room, where any procedure more invasive than skin biopsy is performed. The typical layout has the advantage of being easy and relatively inexpensive to construct and has flexibility for a general dermatologist ( Fig. 51.1 ). It is ideal for a practitioner who has a primarily medical-based practice with some minor surgical procedures such as excisional, laser or minimally invasive cosmetic surgery. For a general dermatology office, this set-up can allow multiple physicians to use common procedure rooms on an as-needed basis. The disadvantages are that this design will not work for a primary surgical practice. In addition, if one anticipates that the surgical component of the medical practice may grow over time, this type of design may not be ideal.
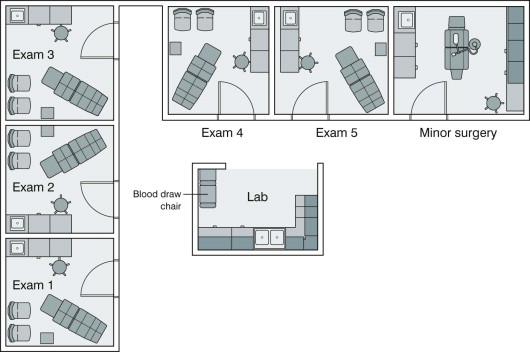
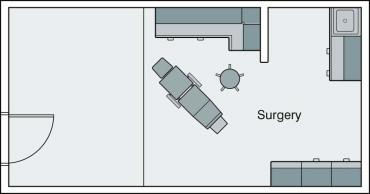
A step up from the dedicated surgical room in a standard medical office is the office-based surgery practice ( Fig. 51.2 ). Offices can be designed with multiple surgical rooms depending upon the size desired and the number of practitioners. The layout can be similar to the floor plan shown in Figure 51.1 with multiple rooms centered around a common space such as a laboratory (for Mohs micrographic surgery) or a clean/dirty room. Smaller rooms that can be used for consultations or follow-ups can be admixed with office-based surgery rooms. This office design is more suited to surgical-based practices, such as Mohs micrographic or cosmetic surgery. When designing an office-based surgical suite, consideration should be given to constructing the suite with the possibility of upgrading to a licensed ambulatory surgery center (ASC) if so desired in the future (see below). One should also decide whether office-based surgery accreditation will be pursued, as this will impact on the construction of the surgical suite (see Ch. 52 ).
Accreditation is a way to demonstrate the delivery of high-quality care to the public and medical community. Others believe that the added expense and preparation time for accreditation are not worth the benefit. Some third-party payers will allow facility fees for procedures performed in accredited offices, but usually ASC licensure and certification are necessary if facility fees are to be collected. Some states have regulations on office-based surgery, specifically with respect to requiring accreditation or state-mandated inspections. Usually these regulations exclude facilities that administer only local anesthesia. Currently, accreditation is not required in any state when only local anesthesia is used in offices.
ASCs, which are the most sophisticated of outpatient surgical facilities, have garnered attention in recent years. ASCs can be broadly classified as physician owned, partially hospital owned, and fully hospital owned. Dermatologists are most familiar with physician-owned, office-based ASCs. These tend to be extensions of a dermatologic surgery practice in which the ASC is a separate entity within the larger medical office. Most dermatologic surgery practices with ASCs will have one or two operating rooms that are used only part of the time. This is in contrast to the larger partially or fully hospital-owned freestanding ASCs that may have as many as 10–15 operating suites with a large full-time staff. The traditional ownership structure of joint-venture ASCs involves a hospital- (or national management company-)owned majority stake (51–90%) and a physician-owned minority stake (10–49%). As the majority owner, the hospital controls the facility and usually processes the billing. The ownership interests of the minority stake are spread among many physicians. Therefore, the ASC is not overly dependent on one physician's volume. More recently, hospitals have begun to take a minority stake in ASCs and physicians have emerged as the primary shareholders. ASCs have become extensions of the physicians' practice, with ASC ownership and dividend distribution taking on a group practice dynamic.
Specific requirements for ASCs vary greatly from state to state. ASC licensure occurs on the state level. State licensure is separate and distinct from Medicare certification. Generally, facility fee reimbursement from third-party payers requires both state licensure and Medicare certification. Accreditation is a separate issue and is usually optional. However, some third-party payers require accreditation for reimbursement. In some states, accreditation is given deemed status for Medicare certification.
Many of the general specifications for ASCs require extensive preplanning. This may not be feasible in some office suites. Some of the requirements include a separate entrance, a separate waiting room, a dedicated recovery room, automatically-activated fireproof doors, and a ceiling sprinkler system. Other ASC design features include 1-h firebreaks in the walls, 2-h firebreaks in the floor, and a back-up emergency power source for key equipment (generator or battery power). Sinks are not permitted in the operating room of an ASC, but are allowed in the recovery room. Exceptions in the fire safety code may be allowed for offices that use only local anesthesia. Medicare and independent accrediting agencies usually require that the fire safety code for ASC construction be followed. Most local zoning boards, states, and office accrediting agencies require that a physician's office meet the commercial building code standards, which are less expensive. From the dermatology perspective, the benefit of incorporating an ASC into a surgical practice is the opportunity to offer a higher level of care and the ability to collect a facility fee. These and other specific reimbursement issues are discussed later in this chapter.
The last outpatient surgical venue is the hospital outpatient department (HOPD). This is a term for ambulatory offices owned wholly by a hospital. Any outpatient surgical service of a hospital, such as dermatologic surgery, would be considered an HOPD. The design of the HOPD surgical suite is similar to the office-based surgery practice. The Joint Commission usually accredits these facilities as they are considered part of the hospital. Physicians and staff are typically employees of the hospital or hospital-owned practice group. The hospital is often able to bill a facility fee for care that is delivered in an HOPD.
The process of planning, designing, and building a new surgical office, including state licensure, Medicare certification, and accreditation, takes approximately 12–18 months. It is helpful to divide the process into stages: (1) financial analysis; (2) legal issues and design; (3) construction and staffing; (4) licensing and other requirements; and (5) accreditation (if pursued). The scope of the project, the physician's familiarity with the process, and the dependence on external consultants will determine the length of each stage. The entire process usually takes longer than one anticipates and meticulous planning and flexibility are necessary.
The hiring of contractors, architects, and consultants is part of the process. Multiple consultants should be interviewed and estimates should be requested from all of them. The disparities may be considerable. The architect should be knowledgeable enough to guide the physician through the design and construction of an office or ASC. Many architects and contractors specialize in medical offices. An architect and contractor who are familiar with code requirements for medical offices and surgical centers will eliminate the need for expensive revisions later to meet specifications. Around $150 per square foot is typical for construction unless the facility is in a prime location in a major urban area. The architect's fee can be 6–10% of the construction cost. Some consultants will provide detailed guidance through the entire process, but can be quite expensive. However, a good consultant will often generate savings that exceed their fees. When consultants are engaged, the physician should still remain involved in the process, particularly if building an ASC or seeking office accreditation. The physician must become familiar with all the rules and regulations, because enforcement will rest with the physician in charge. Preconstruction planning is essential because changes can be very expensive.
The maxim “bigger is better” tends to hold true when referring to the surgical suite. In general, one should overestimate the amount of office space during the design process in order to account for growth and storage. Procedure rooms vary in size and, depending on the level of care and accreditation requirements, minimal square footage requirements may exist. The generally accepted minimum size for a procedure room is 12 × 12 feet (3.7 × 3.7 m), but 20 × 20 feet (6 × 6 m) offers advantages. This may not be a practical use of space for some dermatologic surgeons, especially in urban areas where office space is at a premium. The size of procedure rooms may be determined by requirements for type of anesthesia administered and type of accreditation required.
Cabinets, operating tables, and other equipment will take up a large amount of space. The surgical room must be well ventilated and temperature control is essential because lights can produce extensive “waste” heat. Windows are desirable and supply additional light, but must be secured to comply with aseptic technique. Often windows are tinted to protect patient privacy, depending on how accessible they are to the outside. If laser procedures are to be performed in a procedure room with windows, blinds or other window covers must be used.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here