Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cyclospora, Cystoisospora, and Sarcocystis are coccidian parasites belonging to the phylum Apicomplexa, family Eimeriidae. Coccidian protozoan infections are well recognized but still relatively uncommon causes of diarrheal disease. Cryptosporidium parvum and Cyclospora cayetanensis, two of the more commonly identified coccidian pathogens in diarrheal illness, account for a small but increasing proportion of laboratory-confirmed diarrheal disease reported to the Foodborne Diseases Active Surveillance Network (FoodNet) of the US Centers for Disease Control and Prevention. In 2011, the reported incidences of cryptosporidiosis and cyclosporiasis were 2.85 and 0.05 per 100,000 population, respectively ; in 2017, these rates increased to 3.7 and 0.3 per 100,000 population (1836 and 163 cases), respectively. The almost fivefold increase in cyclosporiasis incidence may reflect, at least in part, changes in testing practices as well as increased use of culture-independent tests (e.g., molecular tests). However, these data need to be put into perspective when statistics show that Campylobacter and Salmonella infections occurred at rates of 16.0 and 19.1 per 100,000, respectively, during the same year.
Cyclospora species are genetically closely related to Eimeria and are more distantly related to Cystoisospora, Sarcocystis, and Toxoplasma. Although several species of Cyclospora have been identified, humans are the only known hosts for C. cayetanensis. Humans are also the only recognized hosts for Cystoisospora belli, and no other Cystoisospora species has been confirmed to infect humans.
Clinical signs and symptoms do not distinguish disease caused by Cyclospora, Cryptosporidium, microsporidia, Cystoisospora, or other noninflammatory causes of diarrhea. However, knowledge of endemic regions, the occurrence of global outbreaks, and the seasonal and geographic variation of diseases such as cyclosporiasis can help point to a particular pathogen. Infection with any of these agents can cause protracted and severe illness in immunocompromised hosts, in particular those with human immunodeficiency virus (HIV) infection, although the incidence of many coccidian infections has decreased since the introduction of highly active antiretroviral therapy. Cyclospora continues to be implicated in foodborne and waterborne outbreaks of diarrheal disease. In contrast, Sarcocystis infection is typically asymptomatic and rarely causes gastrointestinal symptoms.
Cyclosporiasis was first described in humans in Papua New Guinea in 1977. The organism was considered to be a blue-green alga but eluded accurate taxonomic classification until 1993, when Ortega and colleagues in Peru succeeded in inducing sporulation and thus confirmed its genus, Cyclospora. It was named C. cayetanensis after the Universidad Peruana Cayetano Heredia in Lima, Peru, a major site of research on the infection.
Cyclospora oocysts are spherical, measuring 8 to 10 µm in diameter. Ultrastructural studies of the unsporulated oocyst reveal an outer fibrillar coat and a cell wall and membrane. Unsporulated oocysts are excreted in the stool of infected individuals. Oocysts are quite resistant and can survive under diverse environmental conditions, including freezing, 2% formalin, 2% potassium dichromate, and chlorination. Sporulation is required for infectivity and requires at least 7 days of maturation outside the human host; experimentally, in moderate temperatures, sporulation occurs within 7 to 13 days. Each sporulated oocyst contains two sporocysts that each hold two sporozoites.
After ingestion of sporulated oocysts, excystation occurs in the proximal small bowel. Sporozoites penetrate the epithelial cells of the small intestine, where both asexual and sexual reproduction take place. Although the asexual life cycle can continue endogenously within the intestinal epithelium, sexual reproduction leads to the development of zygotes. Zygotes mature into oocysts within the intestinal epithelium, which in turn are released into the stool after causing rupture of the host cells.
Cyclospora infections occur worldwide, sporadically and in clusters, with a major increase in reported cases after its widespread recognition in the mid-1990s. Cases have been reported from all regions of the world. The majority have been described in developing countries of the tropics and subtropics, where the disease seems to be endemic; sporadic cases of disease occur commonly in underdeveloped areas. Prevalence studies in stool samples from developed countries have identified Cyclospora in no more than 0.5% of samples. Cases in developed nations tend to be more frequently associated with recognized waterborne and foodborne outbreaks. Outbreaks in North America in the early and mid-1990s—notably, one outbreak among employees of a Chicago hospital that was attributed to ingestion of water from a contaminated water storage tank and a more widespread outbreak throughout the United States and Canada associated with consumption of contaminated raspberries imported from Guatemala —brought considerable attention to this organism. Other produce, including lettuce, basil, cilantro, watercress, and sugar snap and snow peas, has been implicated in North American foodborne outbreaks since 2000. Produce is presumably contaminated by being washed or sprayed with contaminated surface water. Cyclospora can also cause traveler's diarrhea, although it is not one of the major causes of this illness. Travelers accounted for 37% of all cyclosporiasis cases reported to FoodNet in 2015, but only 1.3% of all travel-related enteric infections were attributed to Cyclospora in the same year. Cyclosporiasis is a recognized opportunistic infection in those with HIV infection and other immunosuppressed conditions.
Humans are the only known hosts for C. cayetanensis. Transmission occurs via the fecal-oral route. The risk for transmission and infection depends on the level of sanitation, as well as the availability of water and food that are at risk of being contaminated. Direct person-to-person spread is unlikely, owing to the need for oocysts to sporulate to become infectious. The infectious dose has not been determined but is presumed to be low. In developing countries infection is more common in children younger than 10 years of age, with the risk for infection decreasing with increasing age. Infants may be somewhat protected through breastfeeding and the absence of exposure to environmental sources of the parasite. Infection occurs seasonally but varies according to geography, with the highest incidence in spring and summer (May through July) in Canada and the United States, in the warm season (April through June) in Peru, before and during the monsoon season (May through October) in Nepal, during drier months (January through March) in Haiti, and during the rainy season (May to August) in Honduras. Factors affecting seasonality and possible reservoirs during the off-season have not yet been defined. Multilocus sequence (genetic) typing suggests that there are geographic differences in circulating subpopulations of C. cayetanensis, which could potentially benefit outbreak investigations by facilitating identification of the source(s) of an outbreak.
Cyclospora cayetanensis –like oocysts have been recovered from a variety of other animals, including mice, rats, dogs, chickens, ducks, and nonhuman primates. Attempts to infect mammals and birds in the laboratory setting have been largely unsuccessful. It is unclear what if any role animals play in the spread of infection and whether oocysts recovered from animal feces represent coprophagy or other zoonotic organisms that resemble Cyclospora. Oocysts have also been identified in sewage and vegetable washings.
The clinical manifestations of Cyclospora infection are varied and differ according to age as well as the degree of endemnicity of the region in which infected individuals live. Asymptomatic infection is more common in the indigenous populations of developing countries, particularly in adults but also in children, suggesting that previous exposure may induce some degree of protective immunity among residents of these regions. However, asymptomatic infection may also occur in others, including those with HIV infection.
Symptomatic disease occurs in both endemic and nonendemic regions. In developing countries, symptomatic disease is more likely to develop in the absence of previous exposure and is thus more common in children. After an incubation of 1 to 11 days (mean, 7 days), illness begins abruptly. A flulike illness may precede the onset of diarrhea, which is invariably present with a median of 6 (range, 5 to 15) watery stools per day. Fatigue, anorexia, myalgia, abdominal cramps, flatus, and nausea occur frequently. Fever is present in approximately 25% of cases. Illness generally lasts from 1 to 7 weeks or longer and may result in dehydration and significant weight loss. Diarrhea can be cyclic or relapsing, especially in the absence of therapy. Disease may be severe in the elderly and life threatening in the immunocompromised; diarrhea and weight loss tend to be more severe, and illness can be prolonged, in individuals with acquired immunodeficiency syndrome (AIDS). Postinfectious fatigue can be profound in some individuals and may persist long after the resolution of other clinical symptoms. It is unknown whether the pathogenesis of disease is due to enterocyte dysfunction or whether toxins are secreted.
Extraintestinal complications of Cyclospora infection are exceedingly uncommon. Reactive arthritis and Guillain-Barré syndrome have both been reported after infection with Cyclospora. Biliary tract disease has been described in patients with AIDS.
The diagnosis of cyclosporiasis generally relies on the microscopic identification of oocysts in stool samples ( Fig. 283.1A ). Shedding of oocysts in stool can precede the onset of clinical illness, but the disappearance of symptoms and oocysts usually occurs simultaneously. Oocysts may be shed in low numbers during infection, and both concentration of stool specimens and collection of multiple specimens may be required to make the diagnosis.
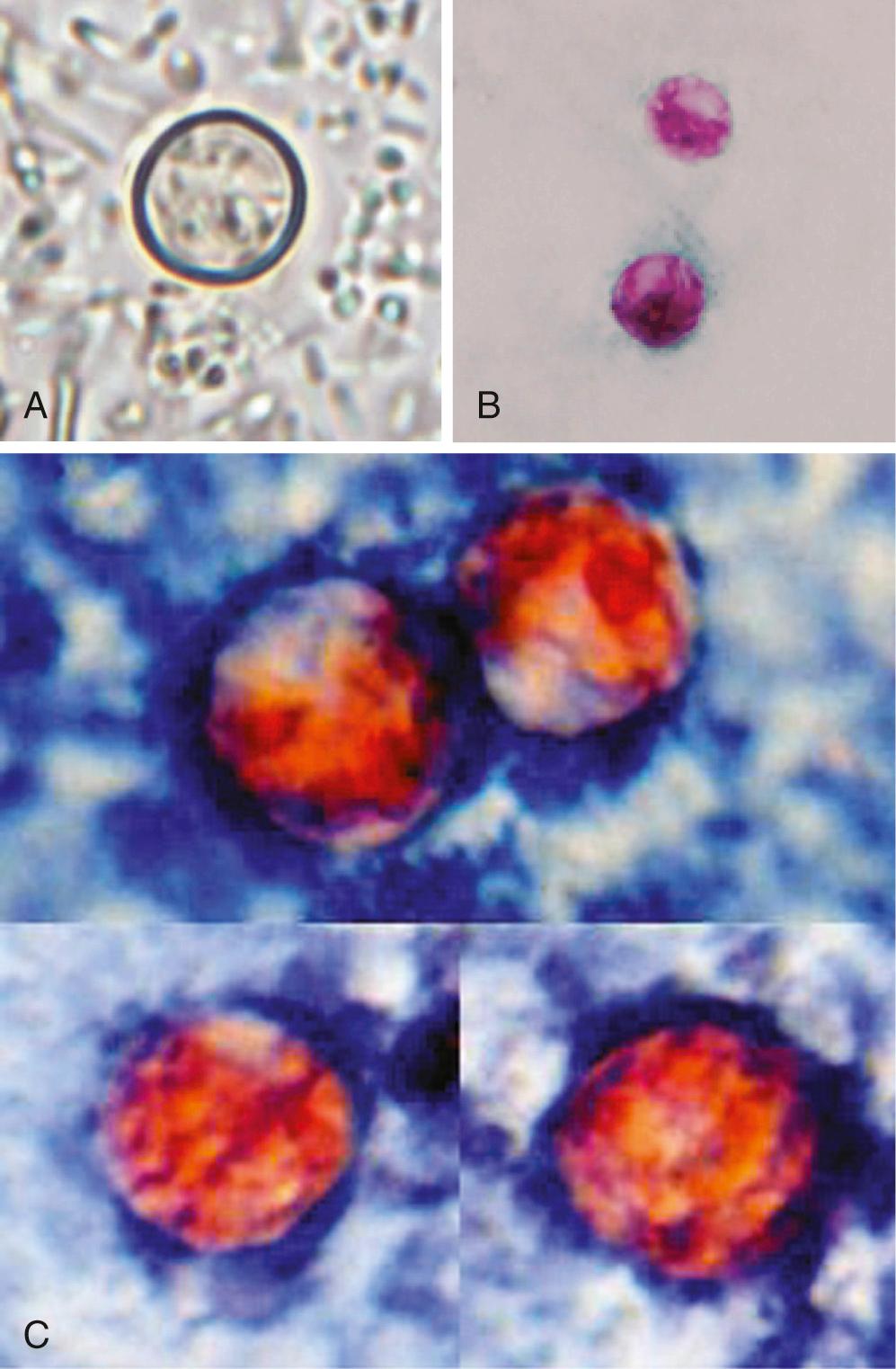
Although Cyclospora oocysts are approximately twice the size of Cryptosporidium oocysts, the two may be confused if oocysts are not measured. The organism is variably acid-fast on modified Ziehl-Neelsen or Kinyoun stain (see Fig. 283.1B ), and such techniques are superior to the examination of routine wet mounts, which require a trained eye for identification of the organism. Therefore if cyclosporiasis is suspected, notification of the laboratory is prudent so that appropriate tests can be performed. Demonstration of blue autofluorescence of the oocysts under ultraviolet epifluorescence microscopy is both rapid and sensitive, although not specific. Additional stains, including auramine, safranin (see Fig. 283.1C ), and lactophenol cotton blue, can also be used. Oocysts cannot be identified using Giemsa and trichrome stains.
Species-specific real-time polymerase chain reaction (PCR) assays have been developed that are capable of detecting low concentrations of oocysts in stool. Newer multiplex PCR-based diagnostic panels include Cyclospora. Although PCR assays may be more sensitive than conventional diagnostic methods, they are costly and may lead to an increased number of diagnosed cases that in turn may require more expert decision making to interpret the results, particularly in endemic settings. Flow cytometry has been proposed as an alternate method of diagnosis. Antibodies to Cyclospora can be detected, but serologic tests are not commercially available.
The diagnosis may also be made by histopathologic or electron microscope examination of jejunal aspirates or biopsy specimens. Endoscopic findings may be normal or may demonstrate inflammation. Microscopic examination of tissue reveals altered histologic architecture of the small bowel, and loss of the brush border and altered epithelial cell morphology may be noted. Villous atrophy, acute and chronic inflammation in the lamina propria, and vascular dilation may be seen. Routine hematoxylin and eosin staining of biopsy material may not permit adequate visualization of the organisms. Tissue sections may reveal Cyclospora in supranuclear locations within the cytoplasm, distinguishing them from Cryptosporidium, which are on the surface of enterocytes.
Trimethoprim-sulfamethoxazole (TMP-SMX) is the recommended therapy for cyclosporiasis ( Table 283.1 ). One double-strength tablet (160 mg TMP/800 mg SMX) given twice daily is the usual dose for adults with normal renal function; for children, weight-based dosage (TMP 5 mg/kg twice daily) should be used. Treatment is continued for 7 days in immunocompetent hosts and for 7 to 10 days in patients with HIV infection. Eradication of oocysts correlates with treatment success. Suppressive therapy (TMP-SMX 160/800 mg three times weekly for 4 weeks) may be required in HIV-infected patients because of the historically high relapse rate (almost 50%) in this population.
| DRUG a | THERAPEUTIC DOSAGE | PROPHYLACTIC DOSAGE |
|---|---|---|
| Trimethoprim-sulfamethoxazole | 1 DS tablet b PO bid for 7–10 days | 1 DS tablet PO 3 times weekly |
| Ciprofloxacin | 500 mg PO bid for 7 days | 500 mg PO 3 times weekly |
| Nitazoxanide | 500 mg PO bid for 7 days |
a Drugs are listed in order of preference.
b One DS tablet contains 160 mg trimethoprim/800 mg sulfamethoxazole.
Individuals who cannot tolerate TMP-SMX may be treated with ciprofloxacin 500 mg twice daily for 7 days, based on a study conducted in HIV-infected patients. If suppressive therapy is indicated, a dose of 500 mg three times weekly may be used. Ciprofloxacin was, however, slightly less efficacious than TMP-SMX for both treatment and prophylaxis. The thiazolide agent nitazoxanide (500 mg twice daily for 7 days) has also been used successfully to treat cyclosporiasis in an immunocompetent adult and was efficacious in the treatment of mixed parasitic infections (including cyclosporiasis) in children. However, studies demonstrating its efficacy in the treatment of cyclosporiasis in HIV-infected patients are lacking.
Cystoisospora belli (formerly Isospora belli ) was first described in 1915. It is the only one of more than 200 identified Cystoisospora species that is known to cause human infection. Human infections previously attributed to Cystoisospora hominis are more likely to have been caused either by Sarcocystis species or by misidentified C. belli.
Immature Cystoisospora oocysts, each containing a single sporoblast, are excreted in the stool of infected hosts. Oocysts can remain viable in the environment for months. Sporulation in the environment is required before oocysts become infectious. Sporulation generally requires 24 to 48 hours but can occur within 16 hours in ideal conditions (30°C–37°C) and is hindered at temperatures below 20°C or above 40°C. The single sporoblast divides in two, and each newly formed sporoblast subsequently matures into a sporocyst. The resulting infective elliptical oocyst (22–33 × 12–15 µm) contains two sporocysts, each with four sporozoites.
Ingestion of sporulated oocysts results in the release of sporozoites in the proximal small intestine. Sporozoites may develop into merozoites, with subsequent asexual reproduction occurring within enterocytes; over time, sexual reproduction follows, resulting in the development and passage of immature, unsporulated oocysts in feces. Rarely, sporozoites can migrate out of the intestine to various tissues, where they may remain dormant as cysts and later give rise to extraintestinal disease.
Cystoisospora species are found worldwide but predominantly in tropical and subtropical climates, especially in South America, Africa, and Southeast Asia. Cystoisospora occasionally cause traveler's diarrhea. In the United States, cystoisosporiasis has been more commonly associated with HIV infection and other immunosuppressed conditions, immigration from Latin America, daycare centers, and psychiatric institutions. In patients with AIDS in the United States, C. belli infection accounted for 2% to 3% of AIDS-defining illnesses in the 1980s, but this decreased to less than 0.1% in the late 1990s, largely because of the widespread use of TMP-SMX to prevent Pneumocystis jirovecii pneumonia. A recent systematic review of Cystoisospora in HIV infection identified a global pooled prevalence of 2.5%, with a higher prevalence in Africa and southeast Asia.
Cystoisospora species other than C. belli have been found in a wide variety of animals, including cats and dogs. It is unclear whether most animals develop clinical disease or whether they merely act as paratenic hosts. Pigs are notable exceptions; Cystoisospora suis can cause severe diarrheal disease and death in piglets and has been implicated in outbreaks of disease among nursing piglets.
The pathogenesis of cystoisosporiasis has not been determined but may be the result of cell damage from direct consequences of parasite invasion, cell-mediated inflammation, or proteins and oxidants released from mast cells.
In immunocompetent hosts, Cystoisospora infection is indistinguishable from other noninflammatory intestinal infections. After an incubation period of approximately 1 week, a self-limited diarrheal illness usually develops that lasts 2 to 3 weeks and is characterized by malaise, anorexia, weight loss, abdominal cramps, and profuse watery diarrhea without blood. Fever is uncommon and if present is usually low grade. Oocyst shedding may persist for several weeks after recovery. Rarely, chronic persistent or intermittent symptoms may continue for many years. Biliary tract disease due to Cystoisospora has been described in immunocompetent hosts.
In immunocompromised hosts, including those with HIV infection or malignancy and those receiving cytotoxic therapy, infection may result in protracted, severe diarrheal illness. Cystoisosporiasis in HIV-infected patients generally occurs with CD4 T-cell counts less than 200 cells/mm. Hemorrhagic colitis, biliary tract disease, disseminated disease, and reactive arthritis have been reported in the literature.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here