Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
“It is much more important to know what sort of patient has a disease than what sort of a disease a patient has.” William Osler 1849–1919
Symptoms relating to vascular insufficiency are common complaints among patients presenting to emergency departments in westernized nations. Unfortunately, vascular insufficiency is often misdiagnosed due to variability in presentation and overlap with other diseases. A careful and thorough clinical examination is a critical initial step in the workup of vascular symptoms, ranging from intermittent claudication to ischemic rest pain and gangrene. It is particularly essential to recognize acute symptoms that may be limb threatening and require immediate intervention. Moreover, many symptoms of nonvascular etiology mimic vascular insufficiency. It is important to differentiate vascular symptoms from those attributed to these other organ systems and make a differential diagnosis.
The goal of the clinical vascular examination is to identify the etiology for the patient’s symptoms, while localizing the specific lesion(s) and judging their relative severity. The astute clinician should be able to make a presumptive diagnosis after the exam, formulate a treatment strategy, and prevent the patient from undergoing unnecessary and costly tests. Although technology has greatly facilitated the ability to identify and localize vascular disease, it should not be relied upon to make the diagnosis. The use of imaging modalities should merely confirm the clinician’s diagnosis after the exam is complete. For some patients, in particular those with acute presentation, the decision to intervene often needs to be made by the end of the examination without any adjuvant studies.
The detection of vascular disease is a comprehensive process that requires careful review of the medical history to reveal significant symptoms and risk factors, a systematic physical examination from head to toe, and the use of appropriate supplementary tests to confirm the diagnosis. This chapter reviews the important elements of the clinical vascular examination, including history and physical exam, risk factors to account for, and bedside procedures that can be used to confirm a diagnosis.
Obtaining an accurate history of symptoms and their chronology is a critical initial component of a vascular exam. Many times a presumptive diagnosis can be made after a detailed history even before the patient has been examined. Conversely, a patient can be referred with an established diagnosis that is determined to be inaccurate after a careful history and exam. Knowing what questions to ask can help determine the severity and seriousness of disease and guide the diagnostic workup. Every patient must be queried as to the location of their pain, duration of symptoms, whether symptoms are intermittent or consistent, whether certain circumstances aggravate or alleviate the symptoms, and the time relationship to other medical events. It is imperative to detect symptoms in the history that indicate whether the disease is acute, compared with chronic vascular insufficiency. Moreover, the patient’s history and risk factors can help distinguish whether symptoms are caused by an embolus or thrombosis. The presentation and patterns of symptoms are discussed in more detail for specific types of peripheral vascular diseases.
The natural history of arteriosclerosis in the lower extremity can be viewed as a progression of symptoms that reflect the degree of vessel occlusion and presence of collateral circulation. Symptoms classically begin with an intermittent and reproducible pain termed claudication, a derivation of the Latin word for “limp.” Intermittent claudication is characteristically brought on by a given degree of exercise and relieved after a few minutes of rest. These symptoms reflect the demand for an increase in blood flow that cannot be met due to atherosclerotic narrowing in one or more arterial segments. The compression of stenotic arteries by exercising muscle, and lack of compensatory vasodilation in diseased segments may also contribute to limited extremity perfusion. This pain is often described as aching, cramping, weakness, or fatigue, and may present in the buttocks, thighs, calves, or foot. This diagnosis must be considered with any exertional limitation of the lower extremity muscles or any history of walking impairment that gets better shortly after rest. Among patients with claudication, 25% will experience worsening symptoms, 5% will eventually require revascularization, and only 1%–2% will come to major amputation.
The specific distribution of claudication reported by the patient is an important focus of the history. Symptoms typically occur in the muscle groups immediately distal to the region of stenosis. The exact site(s) of discomfort or pain should be recorded along with the relationship of this pain to rest or degree of exertion. Narrowing of the aortoiliac vessels classically presents with the constellation of buttock pain, impotence, and lower extremity muscle atrophy, known as Leriche syndrome . Similarly, occlusion of the femoral, popliteal, or proximal tibial arteries will present with exertional calf pain. The presence of intermittent claudication has been found by multiple studies to be reliable symptom used in the diagnosis of peripheral arterial disease. A recent meta-analysis found that the presence of claudication increased the likelihood of arterial disease being present by more than threefold, whereas its absence lowers the likelihood by half that moderate to severe disease is present.
Chronic arterial insufficiency can progress to critical limb ischemia, characterized by rest pain, gangrene, or tissue loss. Rest pain represents progression of ischemia and is usually localized to the lower leg or foot, made worse by elevation (upright) and relieved by the dependent (recumbent) position. This pain may start as a dull, aching sensation in the toes, which progresses to a severe burning pain at night when the patient is lying supine. Patients may describe hanging a foot or limb over the bed or sleeping in a chair to obtain relief. The pain may intensify with cold exposure and be relieved somewhat with application of heat, although strong analgesics are usually needed to manage the discomfort. Skin ulceration and gangrene occur when the minimal nutritional and metabolic requirements of the extremity are not met by adequate blood flow. Usually, multiple levels of arterial disease (iliac, femoral, tibial) are present for this critical ischemia to occur. The pain associated with this process may intensify initially, then diminish or disappear as the tissue necrosis involves the peripheral sensory nerves.
The degree of chronic arterial insufficiency can be categorized by the Fontaine classification ( Table 3.1 ) system based on clinical symptom severity and degree of tissue loss assessed on history and physical exam. Asymptomatic patients are stage I; and patients with claudication are further stratified into those with mild claudication (stage IIA) and those with moderate-severe claudication (stage IIB). It is important to note that progression to chronic limb ischemia in patients with chronic arterial insufficiency is the same whether or not they experience symptoms, because symptomology often depends on patients’ activity levels. Fortunately, only a small proportion of patients (1%–3%) experiencing intermittent claudication will ultimately require major amputation within 5 years.
| Stage | Clinical Description |
|---|---|
| I | Asymptomatic |
| IIa | Mild claudication |
| IIb | Moderate to severe claudication |
| III | Ischemic rest pain |
| IV | Ulceration or gangrene |
Patients with ischemic rest pain are classified as stage III and those with ulcers or gangrene are deemed stage IV. The presence of these severe indicators of occlusive disease portends a poor prognosis with 1-year mortality and major amputation rates of up to 25%.
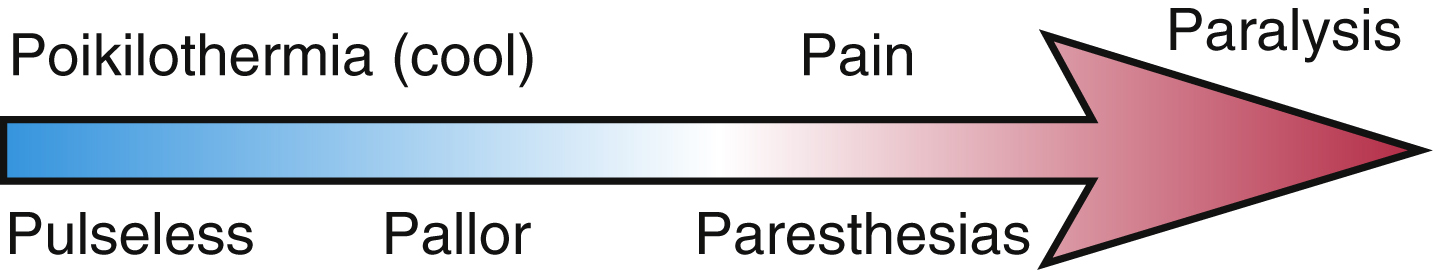
The clinical presentation of acute arterial insufficiency and limb ischemia is characterized by the new onset of extremity pain ( Table 3.2 ) with concurrent changes in neurological function. Pain is typically the first symptom to be described and is characteristically elicited by passive flexion or stretch of the extremity. This pain is usually not localized exclusively to the distal foot and is not affected by limb position, which helps differentiate it from the rest pain of chronic arterial insufficiency. Sensory loss is the earliest neurological sign, and may be very subtle at first but progresses quickly to frank paresthesias. When extremity perfusion continues to be compromised, muscle strength and motor control become diminished. This spectrum of clinical symptoms and findings are termed the “6 P’s,” which stand for pain, pallor, poikilothermia, paresthesias, paralysis, and pulselessness ( Fig. 3.1 ).
| Disorder | Pain Location | Pain Description | Symptoms Onset | Effect of Rest | Positional Effects |
|---|---|---|---|---|---|
| Intermittent claudication | Buttock, thigh, or calf muscles | Cramping, aching, fatigue or weakness | After same degree of exercise | Relieves pain quickly | None |
| Rest pain | Foot | Severe deep pain | At rest | None | Pain alleviated by elevation |
| Nerve root compression/herniated disk | Radiates down posterior leg | Sharp pain | With exercise, but may also occur at rest | Not quickly relieved | Adjusting back position may help |
| Spinal stenosis (pseudoclaudication) | Follows dermatome distribution | Pain associated with motor weakness | After varying amounts of movement or exercise | Relief with changes in body position | Flexion of lumbar spine forward may help |
| Arthritis | Hip, knee, foot | Aching pain | After varying amounts of exercise | Not quickly relieved | Weight taken off joints may help |
| Symptomatic adventitial cysts (Baker cyst) | Behind knee, down calf | Tenderness, swelling | Present at rest and with exercise | Does not help | None |
| Compartment/entrapment syndromes | Usually calf muscles in a muscular patient | Tight, bursting pain | After strenuous exercise | Subsides slowly | Helped by elevation |
| Venous claudication | Entire leg | Tight, bursting pain | After minimal exercise | Subsides slowly | Helped by elevation |
The onset and pattern of these symptoms is an important clue to the cause of blood flow obstruction. The diagnosis of arterial embolism is suggested by the sudden onset of severe pain in an extremity not previously affected by claudication or other symptoms of occlusive arterial disease. This acute pain may be described as crippling and often may leave the distal extremity weakened. A careful review of the patient’s history will usually reveal the source of emboli or associated risk factors. This includes ventricular thrombi generated weeks to months after a myocardial infarction or during atrial fibrillation with or without adequate anticoagulation. Other origins of emboli include deep venous thrombus with a patent foramen ovale, mechanical heart valves, endocarditis, or aneurysms located in the aorta or infrainguinal arterial system.
Acute arterial thrombosis is the other main cause of acute insufficiency and is frequently superimposed on an already narrow atherosclerotic lesion. The pain associated with thrombosis is usually not as abrupt, typically following a crescendo course. Classically a history of claudication or poor circulation is obtained in these patients. The severity and duration of symptoms often correlate with the presence of collateral circulation in the region of the narrowed vessel, which helps to restore distal perfusion. In the absence of collaterals, the pain of thrombosis may be similar to embolic disease. It is important to assess whether the patient has an antecedent coagulation disorder that may predispose to arterial thrombosis. In comparison, patients with deep vein thrombosis may have complaints related to swelling, erythema, and dull pain in the affected extremity. The presence of palpable pulses and/or signs of adequate perfusion in the affected extremity helps differentiate venous thrombosis from an arterial etiology.
The Rutherford classification for acute limb ischemia ( Table 3.3 ) quantifies the degree of ischemia and provides guidelines for determining when to intervene. Based on clinical assessment of motor and sensory function as well as the presence or absence of Doppler signals, a limb can be classified as viable (class I), marginally threatened (class IIA), immediately threatened (class IIB), or irreversibly damaged (class III). It can be difficult to differentiate between class IIB and class III limb ischemia, especially when patients present early. Although class IIB and class III limbs are typically managed differently—with immediate revascularization indicated for the former and delayed revascularization after angiographic investigation offered for the latter—an important exception is the class III limb that presents very soon after onset due to an embolic occlusion. This subgroup of patients can often achieve functional limb salvage after immediate revascularization. Therefore it is crucial to distinguish between an embolic versus thrombotic occlusion, particularly in patients with class III limbs.
| Findings on Exam | Doppler Signals | ||||
|---|---|---|---|---|---|
| Category | Prognosis | Sensory | Motor | Arterial | Venous |
|
Not immediately threatened | None | None | Audible | Audible |
|
|||||
|
Salvageable with prompt treatment | Minimal loss (limited to toes) or none | None | Inaudible | Audible |
|
Salvageable with immediate revascularization | Loss of sensation beyond toes, associated with rest pain | Mild, moderate weakness | Inaudible | Audible |
|
Major tissue loss or permanent nerve damage inevitable | Profound sensory loss, anesthetic | Profound weakness, paralysis, rigor | Inaudible | Inaudible |
It cannot be stressed enough the importance of early diagnosis and intervention: the earlier that an acutely ischemic limb can be recognized and revascularized, the better the patient’s outcome. However, even with widespread utilization of endovascular revascularization techniques such as thrombolysis, up to 15% of patients with acute limb ischemia will require amputation within 1 year.
Patients presenting with carotid disease usually have had a recent transient ischemic attack, stroke in evolution, or completed stroke with persistent neurological deficits. Transient ischemic attacks may include an account of transient monocular blindness or amaurosis fugax. These brief visual impairments are often described by patients as a “fog,” “shade,” or “curtain falling over the eye.” When neurological deficits are fixed, their distribution should be correlated with a point of occlusion in the cerebrovascular circulation. It is important to document the location and chronology of neurological symptoms in all of these patients. Furthermore, a great number of patients with carotid artery disease will be asymptomatic at presentation, but may be identified by certain clues in the history. A recent report of nonspecific visual changes may be the first clues that a patient has significant carotid stenosis. Other sources of embolic disease must also be ruled out, including a patient history of cardiac arrhythmias or known patent foramen ovale.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here