Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The aortic root is the anatomic segment between the left ventricle and ascending aorta. From the surgical viewpoint, it consists of the aortic annulus (AA), aortic cusps, aortic sinuses, and sinotubular junction (STJ). Although the term aortic annulus may be anatomically incorrect, it is often used in surgical anatomy and pathology to describe the aortoventricular junction. Approximately 45% of the circumference of the AA is attached to muscular interventricular septum, and 55% is attached to fibrous tissue, as shown in Fig. 13.1 . This fibrous tissue is the membranous interventricular septum and the fibrous body that connects the anterior leaflet of the mitral valve to the aortic root.

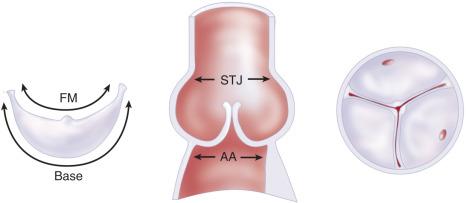
The AA is scalloped and attaches the aortic cusps to the aortic root and left ventricle. The portion of the AA corresponding to the noncoronary cusp is attached entirely to fibrous tissue, whereas the portions corresponding to the left and right coronary cusps are partially attached to fibrous tissue and partially to cardiac muscle. The highest point of the AA, where two cusps meet, is the commissure. The anatomic arrangement of the AA creates a triangular space beneath the cusps, termed the subcommissural triangle. There are three commissures and three subcommissural triangles. The STJ lies immediately above the commissures and separates the aortic root from the ascending aorta. The arterial wall contained between the AA and STJ creates the aortic sinuses, or sinuses of Valsalva. The three aortic cusps have a crescent shape and often are of different sizes, but the length of the base of a cusp is always 1.5 times longer than the length of its free margin (FM), as illustrated in Fig. 13.2 . Thus, a large cusp will have a proportionally longer base (AA), longer FM, longer intercommissural distance along the STJ, and larger aortic sinus. The noncoronary and right cusps and sinuses are often larger than the left cusp and left aortic sinus.
The AA is a three-dimensional structure that evolves along three separate planes, as illustrated in Fig. 13.3A–C . Each aortic cusp is inserted in the annulus along a horizontal plane (see Fig. 13.3D ). For practical purposes, we usually refer to its diameter as the maximal distance at the level of its nadir.
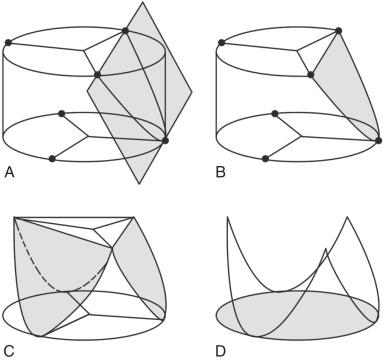
The relationship of the diameters of the AA at this level and at higher levels until reaching the commissures (STJ) varies with age. In children and young adults, the diameter of the AA is 15% to 20% larger than its diameter at the level of the commissures (STJ). As the elastic fibers of the arterial wall decrease with age, the STJ dilates and tends to become equal to the diameter of the lower AA in adults. However, the AA of each cusp evolves along a single horizontal plane (see Fig. 13.3 ).
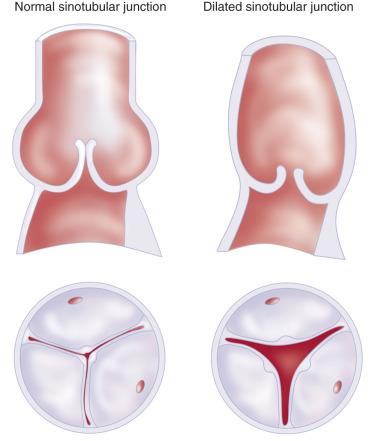
Ascending aortic aneurysms can cause aortic dissection or rupture when their transverse diameter exceeds 55 mm. Aneurysms of the ascending aorta can also cause dilation of the STJ, with consequent aortic insufficiency due to lack of coaptation of the cusps, as illustrated in Fig. 13.4 . One or more aortic sinuses may also become secondarily dilated, but the AA often remains normal. Patients with ascending aortic aneurysms and aortic insufficiency are usually in their sixth or seventh decade of life. If the aortic cusps are normal or minimally elongated along their FMs, it is possible to replace the ascending aorta with correction of the diameter of the STJ, replace one or more sinuses if necessary, repair the cusps if there is prolapse, and reestablish aortic valve competence.
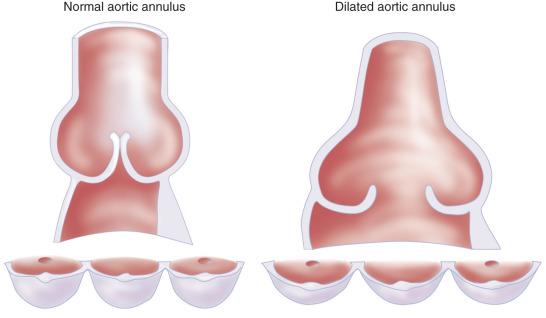
Aortic root aneurysms usually start with dilation of the aortic sinuses and, with time, the dilation extends proximally into the AA and distally into the STJ. Patients with an aortic root aneurysm are usually in the second to fourth decade of life when they need surgery, and the aneurysm is often associated with genetic syndromes, such as Marfan syndrome, Loeys-Dietz syndrome, and others. The two subcommissural triangles of the noncoronary cusp flatten as the AA dilates, which decreases the coaptation area of the cusps and may cause aortic insufficiency ( Fig. 13.5 ). The indication for surgery is usually based on the diameter of the aortic sinuses and family history of aortic dissection. In most cases, surgery is recommended when the diameter reaches 50 mm and less if there is a family history of aortic dissection.
This chapter reviews the operative techniques used to preserve the aortic valve in patients with ascending aortic aneurysm and aortic insufficiency, as well as patients with aortic root aneurysm, with or without aortic insufficiency. The term aortic valve-sparing operation was introduced to describe these procedures.
Patients with an ascending aortic aneurysm are usually asymptomatic, even if they have aortic insufficiency. Although echocardiography often establishes the diagnosis of an ascending aortic aneurysm and provides information regarding aortic valve function, computed tomography (CT) or magnetic resonance imaging (MRI) of the aorta is necessary to determine the extent of the aneurysm. The transverse arch is often involved in older patients with aneurysm of the ascending aorta and aortic insufficiency.
Most patients with aortic root aneurysm are asymptomatic and have only mild or no aortic insufficiency. Some patients complain of vague chest pain. Severe chest pain is suggestive of rapid expansion or an intimal tear with dissection. Echocardiography establishes the diagnosis and gives information regarding aortic valve function. CT or MRI of the aorta is also diagnostic and provides useful information on the remaining thoracic aorta, although the transverse arch is seldom involved.
Transesophageal echocardiography (TEE) is the best diagnostic tool to study the aortic valve and the mechanism of aortic insufficiency in patients with ascending aortic or aortic root aneurysm, as well as to measure the diameters of the AA, STJ, and cusp height. Each component of the aortic root must be carefully interrogated, particularly the aortic cusps. The number of cusps, their thickness, appearance of their FMs, and excursion of each cusp during the cardiac cycle must be examined in multiple views. The coaptation lines of the aortic cusps should be interrogated by color Doppler imaging. The direction and size of the regurgitant jets should be recorded in many views. Information regarding the morphologic features of the AA, aortic sinuses, STJ, and ascending aorta should be obtained. Obviously, the aortic cusps are the most important determinant of aortic valve repair. If the cusps are thin and mobile and have smooth FMs, the feasibility of aortic valve repair is very high, including patients with bicuspid aortic valves.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here