Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
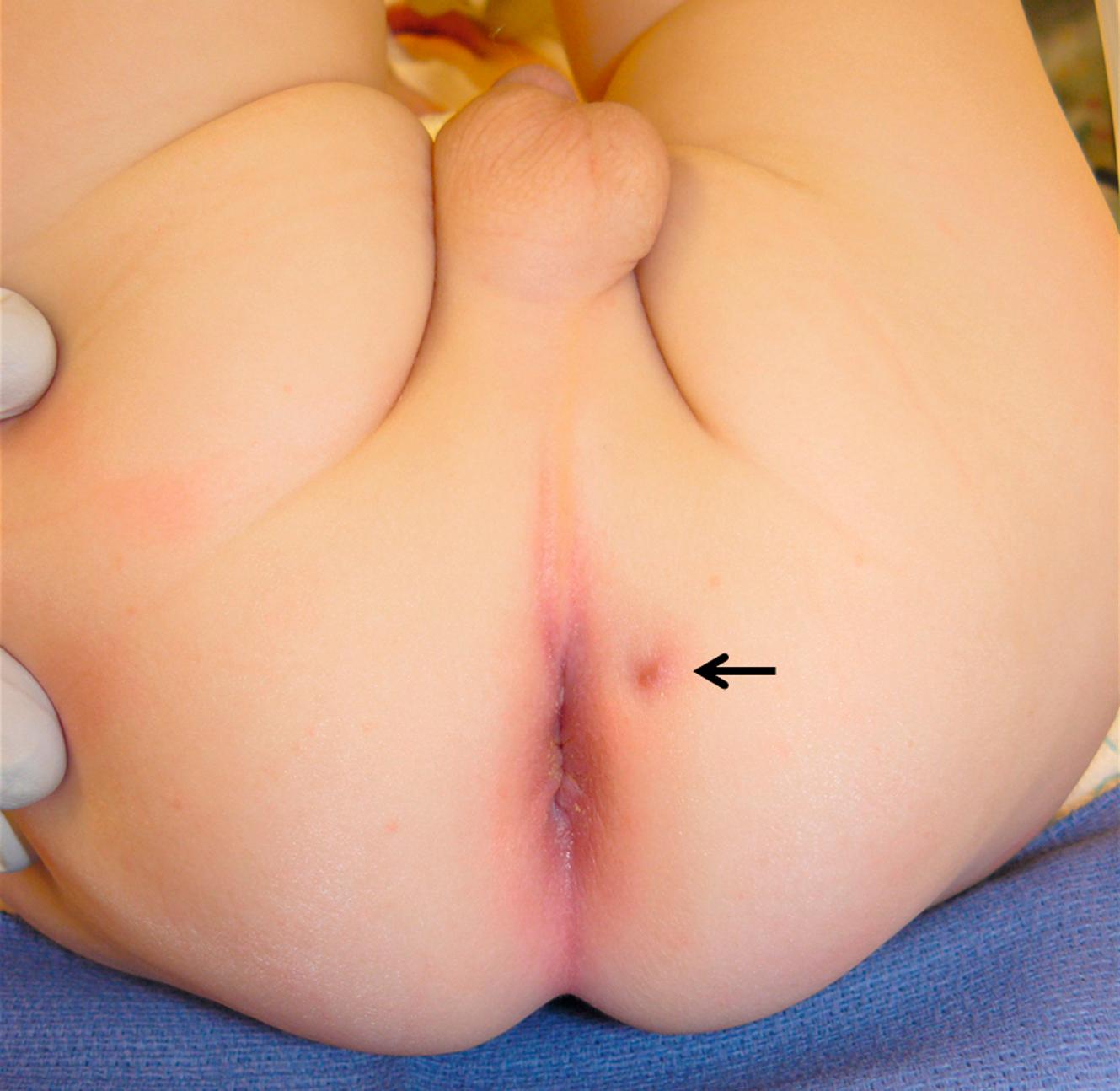
Perianal or perirectal abscesses are often encountered during infancy. The abscess typically presents as a fluctuant, tender mass in the perianal region ( Fig. 37.1 ). A history of stool abnormalities is typically not elicited. Perianal abscesses are much more common in male infants younger than 1 year of age and are infrequent in toddlers and older children. Crohn disease, immunodeficiency, glucose intolerance, and perianal trauma can be causative etiologies in the older child. It is unusual to find complex ischiorectal abscesses in children unless associated with inflammatory bowel disease (IBD).

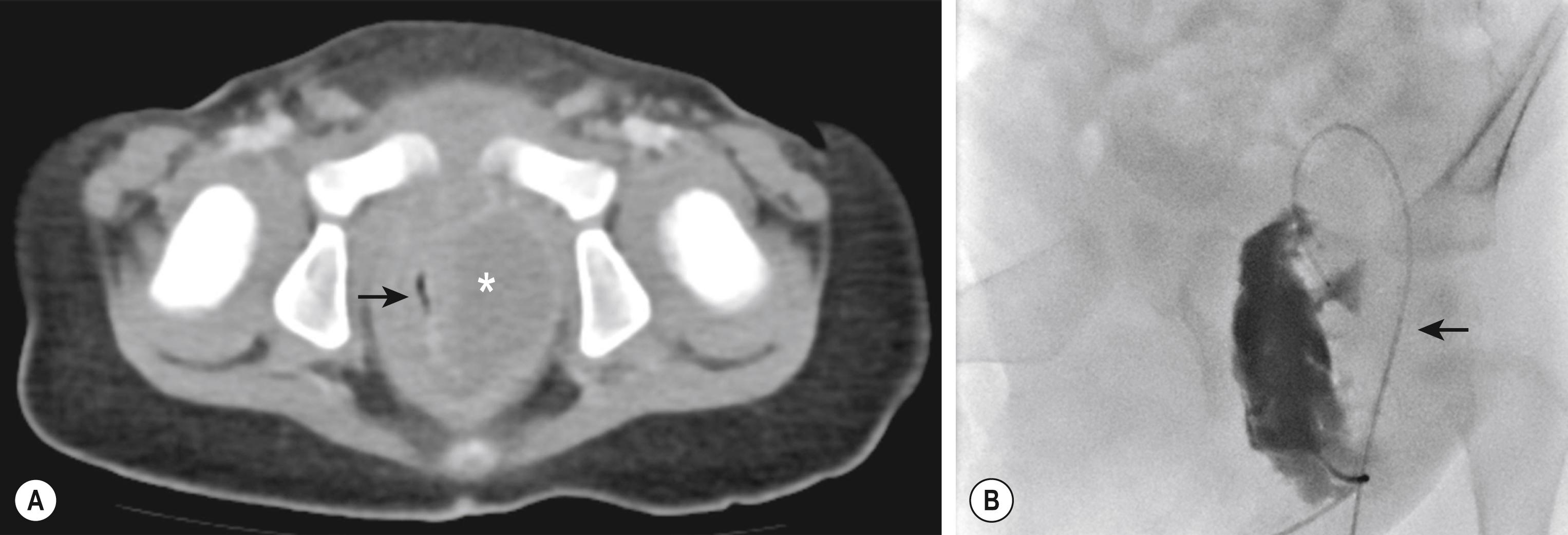
For the infant, sitz baths are prescribed if the abscess does not appear to be fluctuant. Approximately 30–80% of abscesses thus treated resolve without recurrence. Experience with needle aspiration is limited but may be effective in select patients. Initial incision and drainage is reserved for those with significant discomfort, fever, or a large abscess that is unlikely to or has not responded favorably to conservative treatment. Although drainage can be accomplished in the infant without general or topical anesthesia, we prefer a brief inhalational anesthetic to allow for adequate drainage and optimal patient comfort. Considerable debate exists with regard to making an effort to delineate a fistula at the time of abscess drainage, yet we prefer simple abscess drainage as the initial step. The patient begins sitz baths on the first postoperative day. One study suggests that the addition of antibiotics reduces the development of a fistula-in-ano, but not recurrence of an abscess. However, practice patterns differ widely, and evidence supporting additional antibiotic use is not definitive. Complex ischiorectal or supralevator abscesses are rare in infants and children apart from the population with IBD, yet when they occur, drainage may be performed transrectally under image guidance ( Fig. 37.2 ).
As many as 50% of perianal abscesses may progress to a fistula-in-ano, although generally a rate of 20% is often quoted. The child is usually seen after two or more “flare ups” of a perianal abscess that either continues to drain or forms a small pustule that ruptures, only to form again ( Fig. 37.3 ). The fistula is commonly located lateral to the anus rather than in the midline. An intriguing theory has been suggested that fistula-in-ano results from infection in abnormally deep crypts that are under the influence of androgens. The fact that fistula-in-ano rarely follows a perianal abscess in female infants lends credence to this theory.
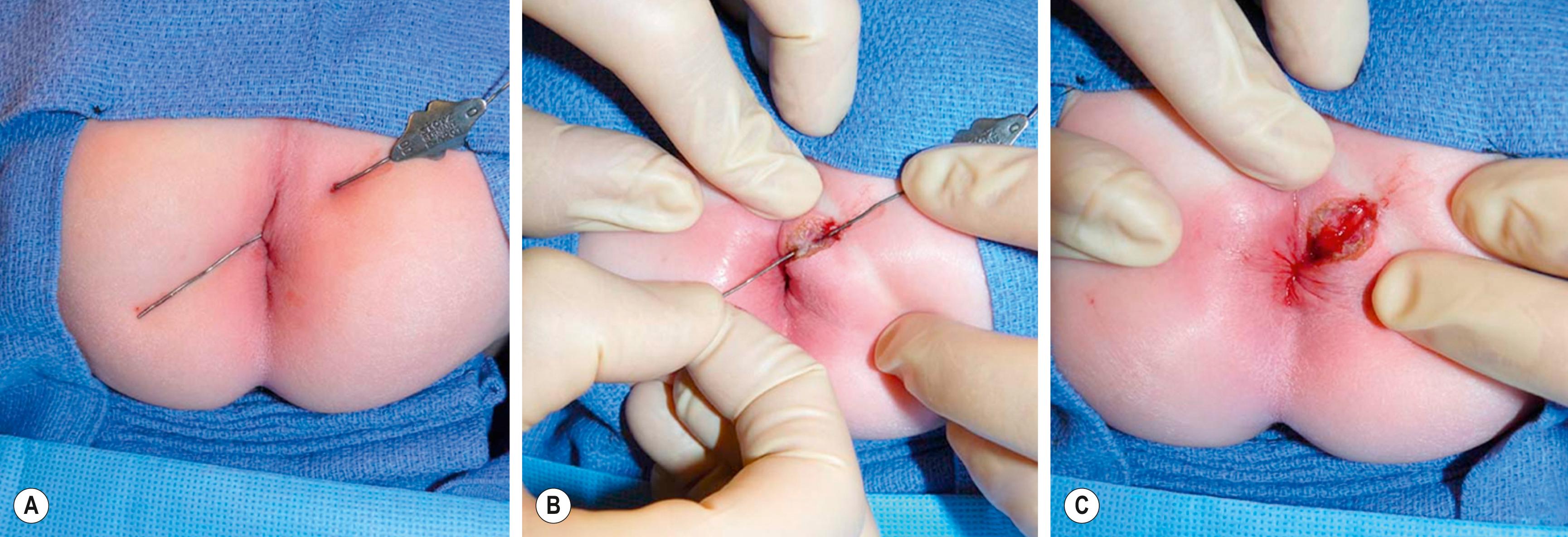
Our preferred operative technique for a fistula-in-ano is fistulotomy ( Fig. 37.4 ). Following the procedure, we instruct the parents to place the infant in a sitz bath after each bowel movement, at least twice daily, and to separate the skin edges of the fistulotomy during bathing to promote healing by secondary intention. We reserve cryptectomy for patients with recurrence, which is rare after an adequate fistulotomy. Additional studies demonstrate acceptable results with seton or fistula plug placement for refractory disease.
In patients with perianal Crohn disease, surgical management focuses on infection control with incision and drainage of the abscess(es) or loose placement of a seton for a fistula-in-ano. Fistulotomy is safe and effective for superficial and low intersphincteric fistulas. Current management after surgical management for the infection varies, but consensus guidelines support biologic agents such as infliximab or adalimumab for induction and maintenance therapy, possibly in combination with immunomodulators such as azathioprine and 6-mercaptopurine.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here