Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acanthamoeba keratitis is the most common exogenous parasitic infection of the cornea in the United States with the significantly greatest risk seen in contact lens wearers of all types.
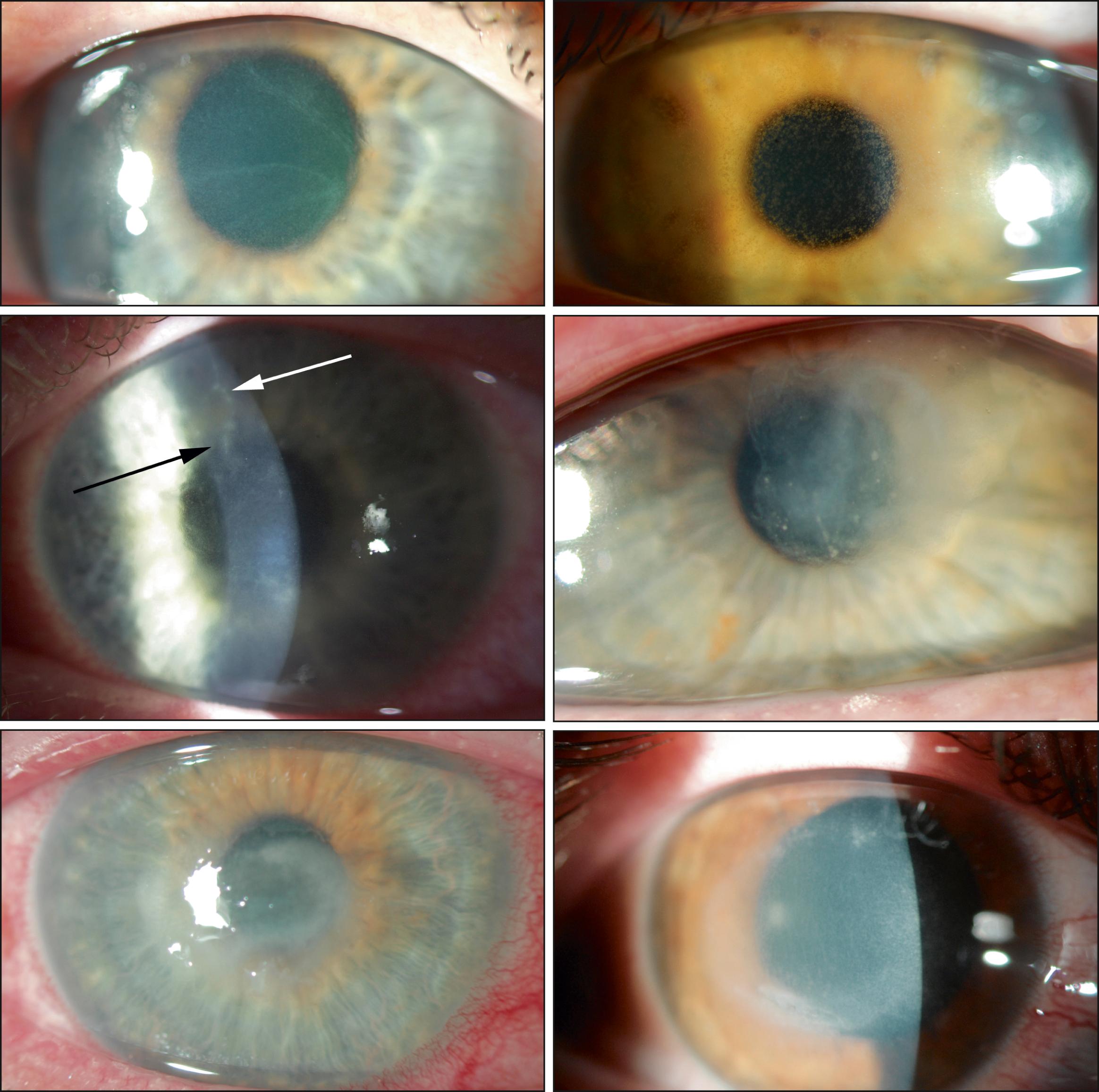
Acanthamoeba keratitis has a wide spectrum of clinical presentations that often mimics herpetic keratitis and other forms of infectious and noninfectious keratitis.
The greatest hurdle to diagnosis is recognition of the possibility of Acanthamoeba keratitis so that appropriate testing and therapy can be employed.
The treatment course for Acanthamoeba keratitis is long and difficult, with outcomes closely associated with severity of initial corneal involvement.
Prevention of Acanthamoeba keratitis is improved with strict adherence to contact lens hygiene and disinfection instruction but may still occur.
The mainstay of medical treatment is the use of topical biguanides but may require other antibiotic drugs as well as immunosuppression to save the eye.
Onchocerca infections are one of the most common causes of corneal blindness in the world, and microsporidial keratitis is an increasingly recognized cause of corneal infections in Asia.
Acanthamoeba keratitis is a chronic, primarily contact lens (CL)-related infection caused by a free-living amoeba found ubiquitously in water and soil. Although classically presenting with radial keratoneuritis, a corneal ring infiltrate, and/or disproportionate, incapacitating pain, most patients will initially present with less characteristic signs and symptoms contributing to misdiagnosis ( Fig. 82.1 ). Commonly mistaken for noninfectious as well as bacterial, fungal, or viral causes of chronic keratitis, the amoebic infection is unresponsive to standard ophthalmic antimicrobial agents. Excellent outcomes are probable when the infection is diagnosed and treatment initiated before deep infiltration. , Traditional medical cure requires the use of biguanides alone or in combination with a diamidine for weeks to months or longer. , Clinical resistance does occur and may require alternative topical or systemic drugs or surgical therapy.
Since its first description in 1973, Acanthamoeba keratitis has been recognized as a generally rare infection characterized by periodic outbreaks. Incidence is expressed relative to the overall number of CL wearers, the group at far greatest risk of infection, but limited knowledge of baseline rates is available because most estimates are based on outbreak analyses. An analysis of the only comprehensive effort to identify cases in the United States encompassing an outbreak of Acanthamoeba keratitis estimated an incidence of 1.49−2.01 cases per million CL users per year. , , With the exception of a regional outbreak in Iowa, a consistently greater incidence, as high as 1 in 30,000 CL users per year or higher, had been found in the UK during the 1990s. , However, since 2003, another US outbreak has persisted, and while no comprehensive U.S. data have been collected, regional incidence estimates for the Chicago area now approach the rates reported in the UK. Furthermore, ongoing outbreaks have been identified around the world over the past decade quantified as two to three times the incidence of comparable periods prior. , Acanthamoeba keratitis is still significantly less common than other forms of CL-related and unrelated microbial keratitis, occurring in between 1 and 25 cases per 10,000 CL wearers/year, primarily dependent on wear regimen. Conversely, Acanthamoebae were identified in only 1% of all patients cultured, regardless of etiology, for possible infectious keratitis in India.
In developed countries, CL wear is the primary risk factor for the development of Acanthamoeba keratitis, with greater than 90% of cases associated with any CL use. , , Initially described in contaminated or agricultural corneal injuries, few cases were reported in the following decade until the early to mid-1980s contemporaneous to a dramatic increase in the popularity of soft CLs. Although greater than 90% of CL wearers who develop Acanthamoeba keratitis wear soft CLs, the remainder are rigid lens wearers, their total slightly below their proportional market share of overall lens wearers. The significantly lower risk of bacterial keratitis in rigid lens wear does not extend to amoebic keratitis, albeit still a lower rate than in soft CL wear. The reemergence of overnight rigid lens use for orthokeratology has led to a markedly increased risk of Acanthamoeba keratitis where epithelial thinning, inadequate hygiene, and routine tap water exposure during care may be contributing factors in these patients.
In both soft and rigid lens wearers, trauma, swimming in lenses, and noncompliance with CL disinfection systems are associated with an increased risk of Acanthamoeba keratitis. Other hygiene-related variables include wearing CL during hot tub use as well as rinsing lenses or cases in nonsterile water. 16,18,20,31,32 A case-control study of the national US outbreak of the mid-1980s found the main association was the use of homemade saline utilizing salt tablets and nonsterile water (odds ratio [OR], infinity) with a smaller association with swimming in lenses (OR, 6.2) and less frequent disinfection (OR, 5.8). Despite numerous changes in CL materials and disinfection systems to improve upon these acknowledged universal poor hygiene practices, little change has been seen in the rates of other forms of CL-related microbial keratitis, further suggesting that periodic outbreaks of Acanthamoeba keratitis may be due to other factors. , ,
While no specific soft lens type has yet been associated with Acanthamoeba keratitis, specific CL care systems have been associated with greater risk. , The systems most effective against both morphologic forms of the amoeba are heat and hydrogen peroxide disinfection, specifically the two-step type, which ensures extended disinfectant exposure time prior to neutralization, which is absent in current one-step systems. Cysts are highly resistant to chlorine and most current multipurpose solutions (MPSs). , , Consequently, the use of one-step hydrogen peroxide systems, , chlorine-based disinfection, and, historically, AMO Complete Moisture Plus, an MPS, has been associated with a relative increased risk of Acanthamoeba keratitis. , , , It should be noted that nearly 50% of patients in the most recent US outbreak were using other disinfectants, mostly other MPSs, suggesting that many of these systems may present additional risk. Similarly, no soft CL wearing schedule, for example, overnight wear and frequent replacement, has yet been associated with Acanthamoeba keratitis, but daily replacement lenses may be protective because solutions are not utilized in their care. Other lens care practices such as solution reuse (“topping off”), not rubbing or rinsing lenses, and household water exposure during lens care or wear have also been suggested as risk factors but are likely secondary factors when compared with the profound effect of water contamination. , , , A moderate decline in cases of Acanthamoeba keratitis in the earlier UK outbreak was thought to be, in part, due to education and modification of these factors. ,
Regardless, the geographical variation found in larger outbreaks remains unexplained. It has been suggested that variations in the level of contamination of the domestic water supply may play a role. , , , Previous surveys have demonstrated a significant geographic variation in Acanthamoeba contamination. , Furthermore, the risk in counties most affected by severe regional flooding was significantly higher (OR, 10.83), and, further, those with private wells rather than municipal water were protected (OR, 0.12) during an outbreak in Iowa. The hardness of domestic water (relative risk [RR], 3.37) and the use of rooftop cisterns have also been identified as risk factors, with microbiologic studies confirming the presence of genotypically identical organisms from patients with keratitis and their cold water taps. , The nonrandom distribution of cases in the Chicago area also suggests a geographic risk factor, which has been hypothesized to be due to changing domestic water disinfection standards combined with an extended water distribution system. Perhaps, this is consistent with the common use of MPS and one-step hydrogen peroxide systems more reliant on control of the ancillary food source, other microorganisms, of Acanthamoebae rather than direct sterilization efficacy. ,
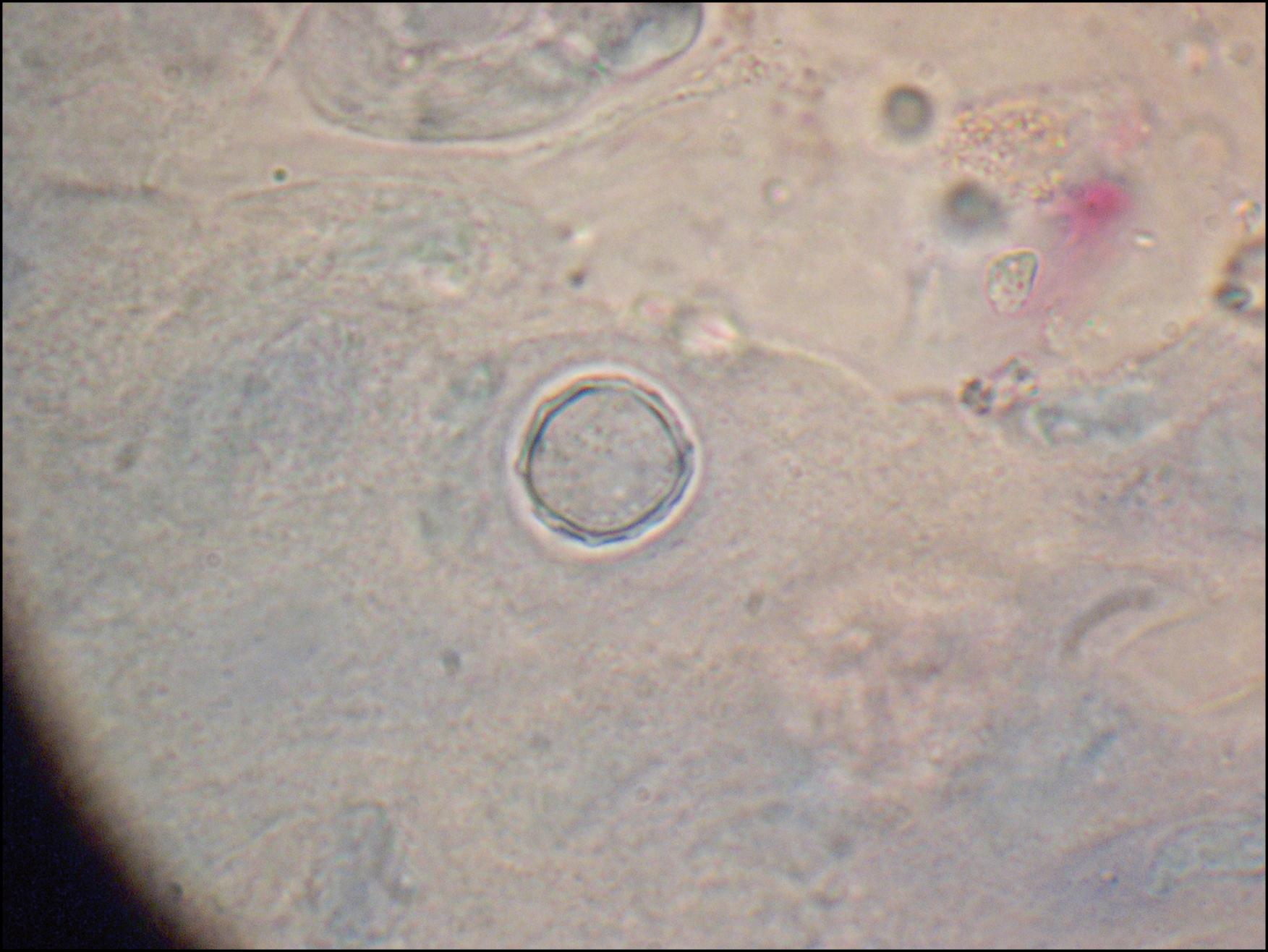
Acanthamoebae are free-living organisms commonly found in water and soil, which prey on other microorganisms. They exist as a more vulnerable, freely mobile trophozoite and as a characteristic double-walled cyst ( Fig. 82.2 ) extremely resistant to extremes of temperature, desiccation, irradiation, antimicrobial agents, and other changes in the environment. Furthermore, when challenged, trophozoites can encyst rapidly, within hours, preserving the ability to produce viable trophozoites decades later. Its primary human disease is keratitis, but in immunocompromised hosts, it may cause the rare conditions granulomatous amebic encephalitis (GAE), disseminated cutaneous amebiasis, as well as visceral forms. A. castellanii is the most common species associated with keratitis, while A. polyphaga and A. hachetti are also commonly identified in larger series. A . culbertsoni, A. rhysodes, A. lugdunensis, A. quina, and A. griffini have also been described. 18S ribosomal DNA typing does not correlate well with earlier nomenclature but permits consistent genotypic classification with most keratitis isolates grouped as T4, with T3 second in frequency. Other genotype groups have constituted a very small minority of reported keratitis isolates.
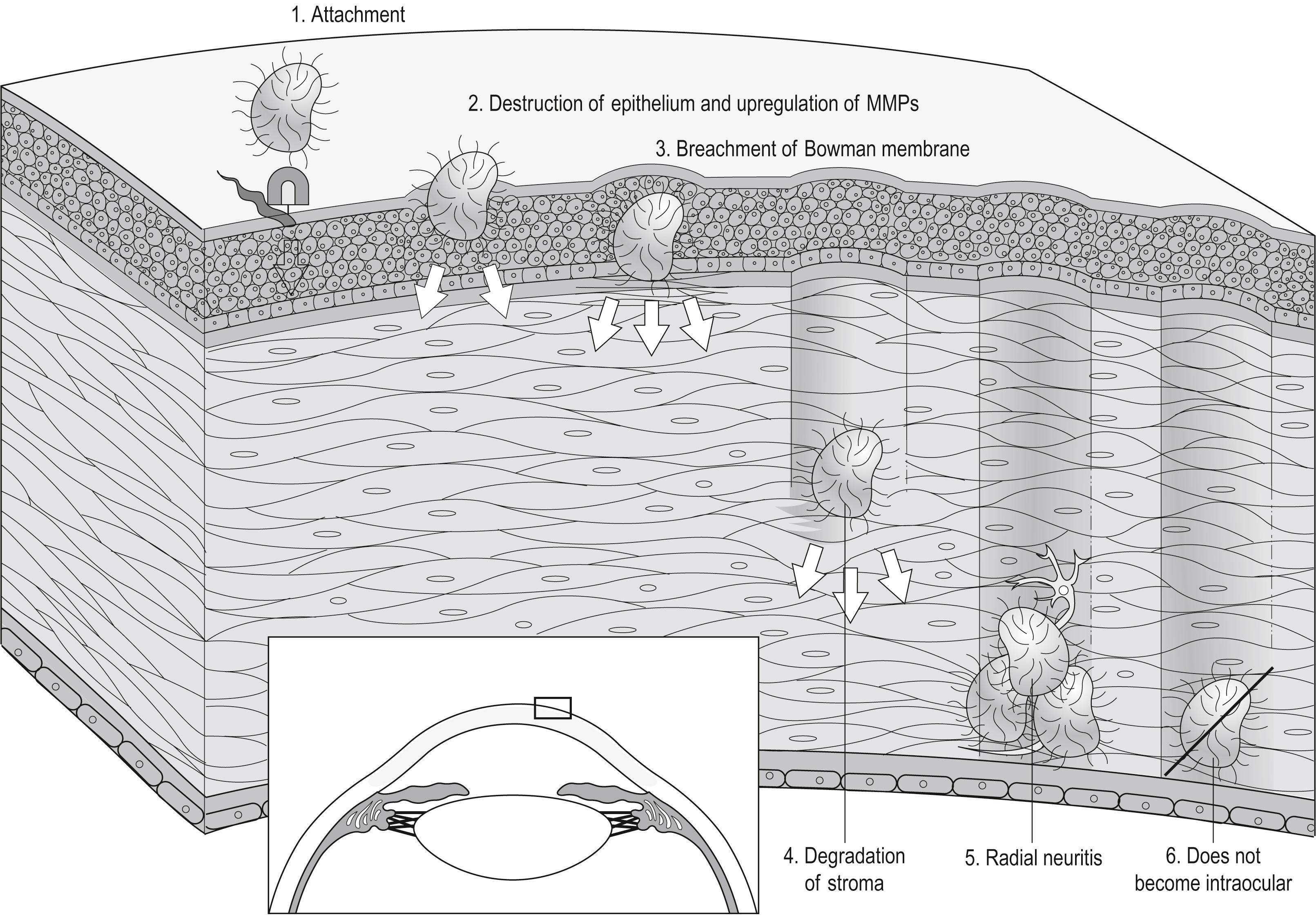
The mechanism and progression of human infection have been inferred from animal models of Acanthamoeba keratitis ( Fig. 82.3 ). Initial attachment of the amoeba is facilitated by its expression of a mannose binding protein, which binds to a corneal epithelial cell’s mannosylated glycoprotein. Corneal injury such as CL wear may increase epithelial expression as well as cytopathic effects. , Once bound, Acanthamoebae then express proteases such as MIP-133, which degrade both corneal epithelium and corneal stroma, promoting invasion and ulceration. In the corneal stroma, the organism can proliferate, subsisting on bacterial prey or, possibly, resident keratocytes.
In animal models, Acanthamoeba keratitis does not induce systemic IgG production. Human studies indicate that a majority of subjects express serum anti- Acanthamoeba IgG, likely, therefore, from other exposures. Once Acanthamoebae are established in the stroma, however, clinically both in humans and in animal models, this systemic immune sensitization appears ineffectual at clearing infection. However, experimental studies have demonstrated that inducement of IgA through oral immunization can be effective at preventing or mitigating infection in animals, presumably by preventing initial attachment or, alternatively, by neutralizing the amoeba’s proteases and thereby impairing their penetration into the deeper layers of the cornea. Interestingly, human studies have found tear IgA levels to be lower in Acanthamoeba keratitis patients versus controls, suggesting that susceptibility may play a role in some patients.
While the precise mechanism of CL-induced risk for Acanthamoeba infection in humans is unclear, it is known that they cause a significant immune deviation of the ocular surface, permitting binding of microorganisms and biofilm formation on the lens and lens paraphernalia. This provides a stable microorganism-rich food supply to encourage proliferation and extend contact time of the amoeba with corneal epithelium, increasing chances of successful binding. Numerous studies have shown increased pathogenicity of Acanthamoeba when cocultured with organisms commonly associated with human disease and also when incorporated inside the amoeba as endosymbionts. Recent in vitro studies suggest that the presence of other microorganisms may actually be necessary for Acanthamoeba infectivity. , It appears that the pathogenesis of Acanthamoeba keratitis is more complex in humans, as evidenced by its nonlinear corneal progression, chronicity of infection, and the variations in corneal pathogenicity clinically encountered.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here