Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Rib nerve pain, called intercostal neuralgia, causes a wide variety of clinical presentations. Although there are multiple causal mechanisms of the disease, the pain transmission pathways remain the same, leading to similarities in treatment approaches. Because intercostal neuralgia is a mononeuropathy with localized pain, peripheral nerve stimulation (PNS) is a useful treatment option.
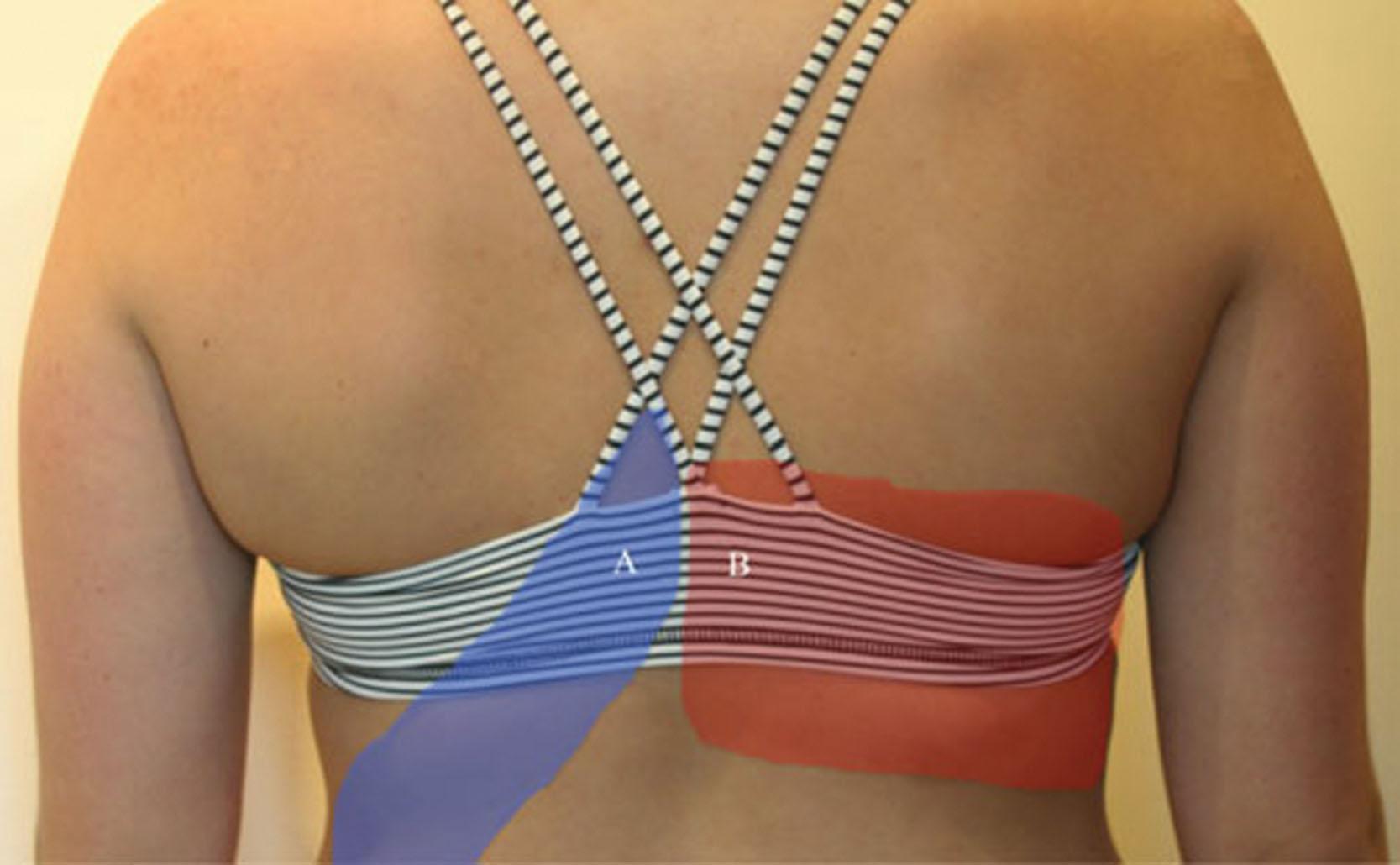
Intercostal neuralgia is neuropathic pain distributed along the affected intercostal nerve(s) pathway along the ribs, chest, or abdomen ( Fig. 16.1 ). It is characterized as a sharp, stabbing, aching, burning pain with allodynia, hyperalgesia, or paresthesia such as numbness and tingling. The pain can be intermittent or continuous. The pain may present in a dermatomal “band-like” pattern or only in localized regions ( Fig. 16.2 ). Moreover, it can present just as rib, chest wall, or upper abdominal pain. It can present as abdominal pain caused by anterior cutaneous nerve entrapment syndrome (ACNE syndrome) ( Fig. 16.3 ). Any movement of the torso or chest wall, including coughing, breathing, or sneezing, can exacerbate the symptoms.


The intercostal nerve is the anterior (ventral) ramus of the thoracic spinal nerve. Its sensory innervation is to the skin of the chest wall and abdomen, while its motor innervation is to intercostal and abdominal wall muscles. After exiting from the spine from the intervertebral foramen, the intercostal nerve travels between the pleura and the posterior intercostal membrane and subsequently traverses to lie deep to or in the internal intercostal muscle. The nerve travels along the inferior border of the corresponding rib along with the intercostal artery and vein to the anterior chest/abdominal wall.
The major branches of the typical intercostal nerves include the rami communicans, posterior cutaneous branch, muscular branches, anterior cutaneous branch, collateral branch, and lateral cutaneous branch ( Fig. 16.4 ).
The gray ramus communicans connects to the sympathetic chain and innervates the corresponding thoracic ganglion.
The posterior cutaneous intercostal branch innervates the muscles and skin of the paraspinal area.
The muscular branches supply the intercostal muscles, latissimus dorsi, serratus anterior, and abdominal wall muscles.
The anterior cutaneous branch travels along the subcostal groove. The anterior branch exits near the midline and divides into medial and lateral branches to supply the anterior portion of the chest.
The collateral branch runs along the upper border of the rib below.
The lateral cutaneous branch pierces the external intercostal muscle at the midaxillary line and divides into anterior and posterior branches to supply the lateral side of the chest.

There are atypical intercostal nerves: T1 and T2, as well as T7 through T12. T1 and T2 provide some contribution to the lower trunk of the brachial plexus, along with the ventral ramus of C8. The first intercostal nerve lacks both the lateral and anterior cutaneous branches seen in typical intercostal nerves. The second intercostal nerve has a branch named the intercostobrachial nerve, and this branch provides cutaneous information from the floor of the axilla and superior region of the upper extremity. T7 through T12 continue anteriorly and, together with L1, innervate the parietal peritoneum of the abdominal wall, called the subcostal nerve ( Fig. 16.5 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here